Resting the Shen: Refining Treatment of Sleep Disturbance Using TCM
Kristina Conner, ND, MSOM, Dipl OM
Tolle Causam
Sleep touches our well-being in every way – a refreshing night’s sleep helps you take on the world; a poor night’s sleep casts a dark shadow over both health and mood. It’s no wonder that sleep disorders are a common complaint to complementary and alternative medicine (CAM) practitioners. Individual stories range from those seeking relief for severe chronic insomnia, to those in good health searching for additional ways to prevent and optimize, and everything in between. Naturopathic physicians find numerous ways to treat sleep disorders, but to improve upon what we do and to find increased success with tough cases, it helps to examine other disciplines. This article will discuss sleep disorders from a Traditional Chinese Medicine (TCM) perspective, then review naturopathic treatments with that framework, in the hopes of refining to improve outcomes. My approach to this topic reflects my background as an experienced naturopathic doctor and a newer TCM practitioner. The way I find myself integrating the 2 is by revisiting my naturopathic treatments with new information from Chinese medicine, and retaining the best of both approaches.
Patterns of Insomnia & Herbal Solutions
There are several types of insomnia: difficulty falling asleep, difficulty maintaining sleep, and non-restorative sleep. These basic categories correlate to the major divisions in common TCM sleep disorder patterns: blood & Qi deficiency, yin deficiency, and excess (heat, fire, phlegm-fire, or food retention). All of these can potentially agitate the shen (spirit), leading to sleep disturbance. Figure 1 breaks down common patterns in TCM that present with sleep issues, and lists their characteristic signs or symptoms.1
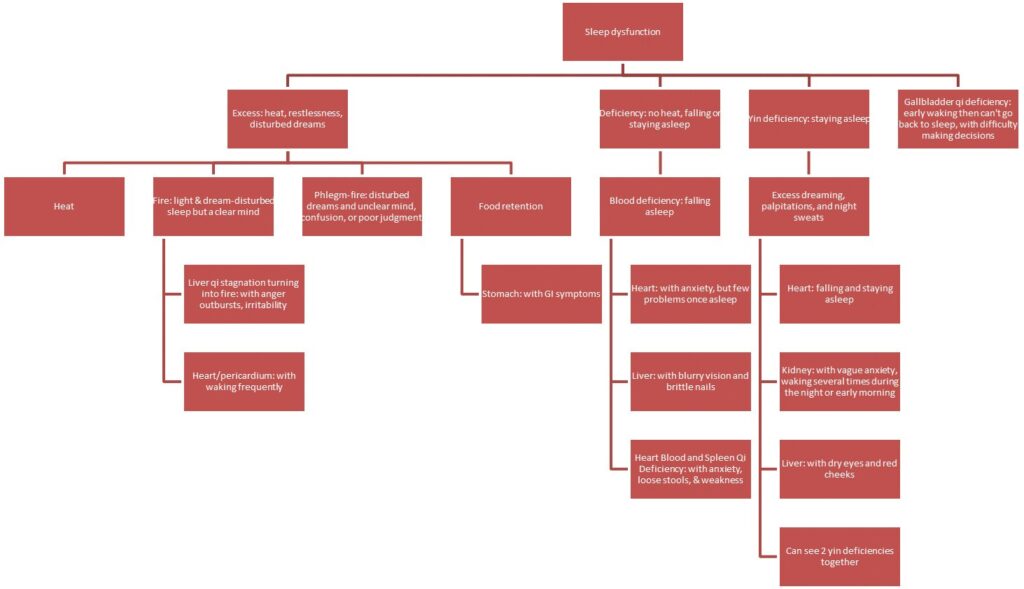 Figure 1. Patterns of Sleep Dysfunction
Figure 1. Patterns of Sleep Dysfunction
The first differentiation of symptoms is whether the presentation is excess or deficiency; it is essential to determine which is the main contributor. Excess patterns are often due to heat/fire or stagnation, which means the disturbed sleep is likely to be accompanied by excess or disturbing dreams, restlessness, and feelings of heat. Deficiency patterns are more likely to present as difficulty falling or staying asleep, without heat or agitation. A large percentage of patients are determined to have a mixed excess/ deficiency pattern when assessing their entire health history, yet the sleep disorder will relate primarily to one.
In a review of the most common types of TCM patterns found in insomnia,2 10 patterns were found to account for 80% of sleep disturbances. Among these 10 patterns were heart (blood) with spleen (Qi) deficiency; kidney yin deficiency with hyperactive fire; liver Qi stagnation transforming into fire; food retention; and heart and gallbladder Qi deficiency.2
Listed below are common formulas used to treat these patterns.1 Herbs also used by Western practitioners, or familiar foods, are noted in parentheses:
- Heart blood and spleen Qi deficiency: Gui Pi Tang (Astragalus, Panax ginseng, Angelica sinensis)
- Heart and kidney yin deficiency with hyperactive fire: Tian Wang Wu Bu Xing Dan (Rehmannia, Schisandra, Panax ginseng, Angelica sinensis)
- Liver qi stagnation transforming into fire: Long Dan Xie Gan Tang (Gentiana, Angelica sinensis, Bupleurum, Glycyrrhiza, Rehmannia, Scutellaria)
- Food retention: Bao He Wan (Crataegus, fermented grain, radish seed, tangerine peel)
- Gallbladder deficiency: An Shen Ding Zhi Wan (Panax ginseng, oyster shell, bone)
Recommendations
A simple treatment would be to include ingredients from these formulas, several times a day in a form that works best (tea, food, or by supplement). However, TCM and Western uses of an herb do not always match; Angelica sinensis, for instance, is widely used in TCM as a blood mover and builder, but is primarily used in Western herbalism for its estrogen-like effects. One might not feel comfortable prescribing it for a sleep issue if the patient had a contraindication to taking Angelica from the hormone-regulation standpoint. Since that tactic may not yield the best results, here’s where TCM indications can refine your choice of Western botanicals.
First, take Valeriana… Using TCM principles, Valeriana is best for heart and kidney yin deficiency, as well as heart blood deficiency with spleen Qi deficiency.3 These are both very common combination disorders leading to sleep problems, so it makes sense that one of our most common Western herbs for insomnia works from the TCM perspective as well. If your patient fits this description well, no need to change from what you are already prescribing. However, if the patient reports more excessive symptoms, like disturbed dreams and restlessness, perhaps a better primary herb is Passiflora (for liver fire or heart/ pericardium phlegm-fire) or Lavandula (for heart fire).3 If the excessive symptoms are accompanied by dyspepsia-like symptoms, then Crataegus (as a component of Bao He Wan formula, as mentioned above) or aromatic digestives like cardamom might be the best choice, since insomnia from food retention may not respond at all to a nervine-based combination.
Understanding the TCM perspective on a Western botanical may also explain non-response to treatment. For example, although Matricaria chamomilla is commonly used as a relaxant and calmative herbal, I have personally never found it to be clinically effective by itself for insomnia. Looking from the TCM perspective, 2 major indications for chamomile are digestive disorders due to stagnation, and pain disorders due to wind.3 While both conditions can lead to insomnia, it now makes more sense to me why chamomile “didn’t work” in those cases where insomnia was the sole complaint.
Beyond botanical medicine, Chinese medicine can also inform other aspects of treatment. Again using the concept of excess/deficiency, there is a strong emphasis on diet to restore deficiency states, especially long-term ones. Diet prescriptions to build blood would include red and organ meats, bone broth, watercress, wheatgrass, other dark greens/grasses, berries, sweet rice, and oats. Yin-building foods include tofu, sesame, alfalfa, bean sprouts, sea veggies and animals, beans, and eggs.4 The underlying concept for both is mineral-rich foods, particularly high in iron and/or calcium; by extension, direct mineral supplements could also be added.
Some Non-Herbal Approaches
What about melatonin, 5-hydroxytryptophan (5-HTP), inositol, and other common supplements? In this area, there is no straightforward answer, as it’s unclear how to categorize new supplements according to TCM principles. But examining them more closely may yield a few suggestions.
Take melatonin, a common supplement for sleep enhancement… The function of the pineal gland is recognized in Chinese medicine, but there is no Chinese herbal recognized to stimulate it; there is, however, an acupuncture point. Yin tang, an extra point located between the eyebrows, correlates to the 6th chakra and is also known as the “third eye.” Yin tang is widely used for sleep disorders and stress management in TCM, and may stimulate what would be considered pineal gland function in Western medicine. For non-acupuncturists, acupressure could be substituted at that point. Even making the area a focal point through meditation or relaxation techniques might be a starting point, since it’s likely to be part of any naturopathic prescription for sleep disturbance.
Among other treatments for insomnia, tai chi has also been shown to be effective for sleep disturbance in the elderly.5,6 In one study, comparing cognitive behavioral therapy (CBT) to tai chi for insomnia, tai chi improved sleep quality and reduced fatigue, though CBT was overall more effective.7 However, both were shown to reduce inflammation: tai chi reduced cellular inflammation, and CBT reduced systemic inflammation.8
Summary
In conclusion, these examples show how TCM theory can positively influence naturopathic medicine treatment of sleep disorders. Using a simple assessment of the patient’s symptoms for typical excess or deficiency patterns, we can expand naturopathic treatment with additional tools for sub-pathology states and creative substitutions for common Western botanicals in treatment of insomnia.
 Kristina Conner, ND, MSOM, Dipl OM, is Professor of Clinical Sciences at National University of Health Sciences in Lombard, IL, where she teaches courses in nutrition, naturopathic medicine, and hydrotherapy. Dr Conner received her ND from Bastyr University and her MSOM from NUHS. She completed a residency at the University of Bridgeport, where she later served as clinical faculty. Dr Conner practiced in Indiana before becoming a founding faculty member for the ND program at NUHS. In addition to maintaining a part-time practice at World Tree Natural Medicine, Dr Conner currently serves as president of the Illinois Association of Naturopathic Physicians.
Kristina Conner, ND, MSOM, Dipl OM, is Professor of Clinical Sciences at National University of Health Sciences in Lombard, IL, where she teaches courses in nutrition, naturopathic medicine, and hydrotherapy. Dr Conner received her ND from Bastyr University and her MSOM from NUHS. She completed a residency at the University of Bridgeport, where she later served as clinical faculty. Dr Conner practiced in Indiana before becoming a founding faculty member for the ND program at NUHS. In addition to maintaining a part-time practice at World Tree Natural Medicine, Dr Conner currently serves as president of the Illinois Association of Naturopathic Physicians.
References:
- Maciocia G. The Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists. Oxford, UK: Churchill Livingstone; 2005.
- Poon MM, Chung KF, Yeung WF, et al. Classification of insomnia using the traditional Chinese medicine system: a systematic review. Evid Based Complement Alternat Med. 2012;2012:735078.
- Holmes P. The Energetics of Western Herbs: Treatment Strategies Integrating Western & Oriental Herbal Medicine. Boulder, CO: Snow Lotus Press, Inc; 1997.
- Pitchford P. Healing with Whole Foods: Oriental Traditions and Modern Nutrition. Berkeley, CA: North Atlantic Books; 1993.
- Li F, Fisher KJ, Harmer P, et al. Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc. 2004;52(6):892-900.
- Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: A randomized controlled trial of Tai Chi Chih. 2008;31(7):1001-1008.
- Irwin MR, Olmstead R, Carrillo C, et al. Cognitive behavioral therapy vs. Tai Chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial. 2014;37(9):1543-1552.
- Irwin MR, Olmstead R, Breen EC, et al. Cognitive Behavioral Therapy and Tai Chi Reverse Cellular and Genomic Markers of Inflammation in Late-Life Insomnia: A Randomized Controlled Trial. Biol Psychiatry. 2015;78(10):721-729.