Recognizing Anaphylaxis in Infants and Children
Signs, Tiggers, and Criteria to Diagnose and Treat Pediatric Anaphylaxis
Tamara Cullen, ND
You have just given the second diphtheria and tetanus toxoids and pertussis vaccination in the series to a healthy 7-month-old girl in your office, and she seemed to tolerate it well, like she did in the past. As her mother was checking out at the front desk, she noticed that her infant was drooling a bit more than usual. The receptionist calls for you to evaluate the situation because the mother is starting to become anxious about the child. You come to the front and see that the infant is, in fact, drooling quite a lot and is chewing on her tongue, which seems enlarged in her mouth. You have the mother sit down with the infant so that you can better assess her. You perceive no signs of respiratory distress, hear no wheezing, and see no hives. However, you notice that the infant’s cheeks are looking flushed bilaterally. What is your concern at this moment, and what do you do? Does this infant meet the criteria for anaphylaxis? Do you have injectable epinephrine in your office, and do you know how to use it?
What Does Anaphylaxis Look Like in an Infant?
We know from case studies that anaphylaxis is underrecognized and undertreated, especially in infants and children.1 As you can imagine, anaphylaxis may be difficult to recognize in infancy for many reasons, including the following2: (1) Anaphylaxis
is sometimes the first clinical manifestation of sensitization to a triggering allergen.
(2) The symptoms of anaphylaxis cannot be described by infants. (3) Many of the signs of anaphylaxis are nonspecific and are also seen in healthy infants for other reasons (eg, loss of sphincter control, regurgitation or spitting up after feeding, and sudden crying and irritability with colic or flushing, hoarseness, or dysphonia after a crying spell). (4) Sometimes, the only symptoms at the onset of anaphylaxis in infancy are the sudden onset of lethargy or hypotonia and the abrupt cessation of activity.
Who Is at Risk?
It is important to note who the at-risk infants are in your practice so that you can be more aware of the possibility of anaphylaxis before an event. These children include those with atopic dermatitis, those with urticaria pigmentosa or mastocytosis, and those with respiratory diseases such as asthma, bronchiolitis, and croup.3
What Are the Typical Triggers?
Food is a common anaphylactic trigger, and while egg and cow’s milk are the most common in infancy, any food can be a trigger. This includes foods often presumed to be harmless (eg, probiotics, cross-contaminated formulas, and goat’s milk or hypoallergenic formulas)4 and foods less frequently given to infants (eg, sesame). Infants can be sensitized to foods in utero through breast milk, through ingestion of the food directly, or through accidental exposure (eg, food encountered and put in the mouth by a crawling infant or food given to the infant by an older sibling or a caregiver).5
Less common triggers include the following: insect stings, inhalants (eg, cat, horse, and hamster dander), natural rubber latex (eg, bottle nipples, pacifiers, and toys), medications (antibiotics, especially β-lactam antibiotics, and nonsteroidal anti-inflammatory drugs such as ibuprofen), and vaccines (usually due to a vaccine constituent such as gelatin, egg, latex, or yeast rather than the microbial agent in the vaccine). Even nonimmune triggers such as cold air or water exposure can be implicated.
How Do You Diagnose Anaphylaxis?
Three criteria diagnose anaphylaxis, with each reflecting a different clinical presentation. Anaphylaxis is likely when any 1 of the following 3 criteria is met6.
Criterion 1
The first criterion is acute onset of an illness (during minutes to several hours) involving the skin, mucosal tissue, or both (eg, generalized hives, pruritus or flushing, and swollen lips, tongue, or uvula) and at least 1 of the following: (1) respiratory compromise (eg, stridor, dyspnea, hypoxemia, wheeze-bronchospasm, or reduced peak expiratory flow) or (2) reduced blood pressure (BP) or associated symptoms of end-organ dysfunction (eg, hypotonia, syncope, or incontinence).
Note that cutaneous symptoms are present in up to 90% of anaphylactic reactions. Therefore, this finding will frequently be helpful in making the diagnosis.
Criterion 2
The second criterion is the occurrence of 2 or more of the following rapidly after exposure to a likely allergen for that
patient (during minutes to several hours):
(1) involvement of the skin-mucosal tissue (eg, itch-flush, generalized hives, or swollen lips, tongue, or uvula), (2) respiratory compromise (eg, stridor, dyspnea, hypoxemia, wheeze-bronchospasm, or reduced peak expiratory flow), (3) reduced BP or associated symptoms (eg, hypotonia, syncope, or incontinence), or (4) persistent gastrointestinal symptoms (eg, crampy abdominal pain or vomiting).
Note that skin symptoms or signs are absent or unrecognized in 10% to 20% of anaphylactic episodes. This criterion incorporates symptoms in other organ systems and is applied to patients with exposure to a substance that is a likely allergen for them.
Criterion 3
The third criterion is reduced BP after exposure to a known allergen for the patient (during minutes to several hours). Reduced BP in adults is defined as a systolic BP of less than 90 mm Hg or a decrease from that person’s baseline exceeding 30%. Reduced BP in infants and children is defined as a low systolic BP (age specific, as defined herein) or a decrease in the systolic BP exceeding 30%. Low systolic BP for children is defined as less than 70 mm Hg for those aged 1 month to under 1 year, less than 70 mm Hg plus twice the age for those aged 1 to 10 years, and less than 90 mm Hg for those aged 11 to 17 years.
Note that this criterion is intended to detect episodes of anaphylaxis that consist of isolated cardiovascular symptoms. It is applied to individuals who have been exposed to a substance to which they are known to be allergic.
How Do You Treat Anaphylaxis?
Epinephrine is the first-line therapy for anaphylaxis, and there is no known equivalent substitute. A systematic review of the literature revealed no randomized controlled trials that support the use of H1 antihistamines (such as cetirizine hydrochloride and diphenhydramine) in anaphylaxis.7 Despite this, H1 antihistamines are the most commonly administered medications to treat anaphylaxis. These agents only mitigate itching and hives and do nothing to relieve shock, hypotension, and upper or lower airway obstruction. In addition, the first-generation H1 antihistamines (such as diphenhydramine) may, in fact, complicate anaphylaxis by leading to sedation and inability to recognize further progression of the anaphylaxis.8 In overdose, they can lead to respiratory distress and even death in infants.
For infants and children, the recommended epinephrine dose (1.00 mg/mL) is 0.01 mg/kg (up to 0.50 mg per dose), injected intramuscularly into the mid anterolateral thigh (vastus lateralis muscle). The dose should be drawn up using a 1.00-mL syringe. This treatment may be repeated at 5-minute to 15-minute intervals.
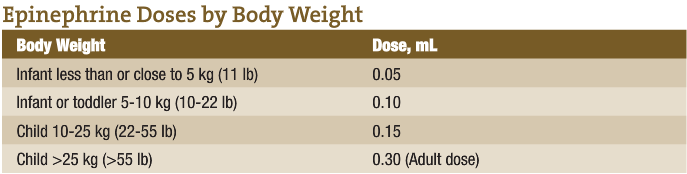
Epinephrine Doses by Body Weight
Epinephrine can also be administered into the mid anterolateral thigh using an autoinjector. These are available in 0.15-mg and 0.30-mg doses. Children weighing 25 kg or less should receive the 0.15-mg dose.9 Most infants weigh less than 15 kg. This presents a dilemma for clinicians who want to prescribe an epinephrine dose of 0.01 mg/kg; therefore, a drawn syringe would be more appropriate in these cases. Autoinjector needle length is also a concern. The optimal needle length for intramuscular injection
in the thigh in infants and toddlers is 2.2
to 2.5 cm. However, most epinephrine
autoinjector needles are approximately
1.4 cm, which is not long enough to provide intramuscular injection for some infants and toddlers.
Remember that there are no contraindications to the use of epinephrine as the first-line treatment of anaphylaxis. Knowing how to correctly identify and treat anaphylaxis in infants and children will save lives.
 Tamara Cullen, ND is a 1999 graduate of Bastyr University and practices primary care medicine in Seattle. She currently serves as adjunct faculty at the Bastyr Center for Natural Health and as the advanced pediatrics professor at Bastyr University. She is a founding board member of the newly formed PedANP, and co-author of The Baby Cuisine Cookbook. She spends the majority of her time at her private practice, Naturopathic Family Medicine, and loves to swim, run, travel, and spend time with her family.
Tamara Cullen, ND is a 1999 graduate of Bastyr University and practices primary care medicine in Seattle. She currently serves as adjunct faculty at the Bastyr Center for Natural Health and as the advanced pediatrics professor at Bastyr University. She is a founding board member of the newly formed PedANP, and co-author of The Baby Cuisine Cookbook. She spends the majority of her time at her private practice, Naturopathic Family Medicine, and loves to swim, run, travel, and spend time with her family.
References
Lin RY, Anderson AS, Shah SN, Nurruzzaman F. Increasing anaphylaxis hospitalizations in the first 2 decades of life: New York State, 1990-2006. Ann Allergy Asthma Immunol. 2008;101(4):387-393.
Rudders SA, Banerji A, Clark S, Camargo CA Jr. Age-related differences in the clinical presentation of food-induced anaphylaxis. J Pediatr. 2011;158(2):326-328.
Brockow K, Jofer C, Behrendt H, Ring J. Anaphylaxis in patients with mastocytosis: a study on history, clinical features and risk factors in 120 patients. Allergy. 2008;63(2):226-232.
Lee TT, Morisset M, Astier C, et al. Contamination of probiotic preparations with milk allergens can cause anaphylaxis in children with cow’s milk allergy.
J Allergy Clin Immunol. 2007;119(3):746-747.
Boyce JA, Assa’ad A, Burks AW, et al; NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-Sponsored Expert Panel report. J Allergy Clin Immunol. 2010;126(6):1105-1118.
Sampson HA, Muñoz-Furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report: second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117(2):391-397.
Sheikh A, Ten Broek V, Brown SG, Simons FE. H1-antihistamines for the treatment of anaphylaxis: Cochrane systematic review. Allergy. 2007;62(8):830-837.
Soar J, Pumphrey R, Cant A, et al; Working Group of the Resuscitation Council (UK). Emergency treatment of anaphylactic reactions: guidelines for healthcare providers. Resuscitation. 2008;77(2):157-169.
Simons FE. First-aid treatment of anaphylaxis to food: focus on epinephrine [published correction appears in J Allergy Clin Immunol. 2004;113(6):1039]. J Allergy Clin Immunol. 2004;113:837(5):837-844.