Hydrogen Sulfide Dysbiosis: A Case Study
Nirala Jacobi, BHSc, ND
Naturopathic Perspective
“Mary,” a 65-year-old woman, was referred to me for further treatment for small intestinal bacterial overgrowth (SIBO). She had been given the diagnosis of SIBO in 2015 following a lactulose breath test, and despite numerous herbal treatments and dietary interventions, she reported that “Nothing has ever improved with SIBO treatment.”
The Case
Mary’s main complaints were constipation, fatigue, depression, fibromyalgia, gas and bloating, pain around the umbilicus (which occurred randomly), and gastric reflux due to a hiatal hernia. Past medical history was negative for recalling any case of food poisoning and was positive for having had a cholecystectomy many years prior.
Her bowel movements occurred 2-3 times weekly and were a 1 or 2 on the Bristol Stool Chart. She was observing a low-FODMAP diet, but had stopped being very regimented with her diet.
Evaluation
She had not been retested for SIBO in almost 2 years, so I decided to get a good understanding of her digestive tract. I ordered a lactulose breath test and a comprehensive stool analysis including microbiome DNA analysis. I sent Mary home with a bottle of herbal bitters (gentian, Oregon grape, dandelion root, baical skullcap), with instructions to take 3 dropperfuls 3 times per day before meals. I also started her on Phase 1 of the SIBO Bi-phasic diet.
I often start my treatment this way while I await test results. The SIBO Bi-phasic diet is a phased protocol that helps practitioners to organize their treatment approach. Phase 1 is quite restricted, removing all dairy and most FODMAPs, grains, and fruit. By the time the patient with SIBO (confirmed by lactulose breath testing) returns, they often report improvement before antimicrobials are even prescribed.
Four-Week Follow-up
Mary returned for her second appointment 4 weeks later. Instead of feeling better, she felt “much worse.” Her fatigue, body aches, mood, and constipation had all worsened and she felt like giving up.
Lactulose Breath Test
Her breath test (Figure 1) revealed a “flatlining” result for hydrogen, and a mildly positive result for SIBO in the combined hydrogen/methane category. During a 3-hour lactulose breath test, a significant rise in hydrogen is expected when the substrate (lactulose) arrives in the colon where hydrogen-producing bacteria are abundant. In cases where methanogenic bacteria are plentiful in the small intestine, hydrogen can be utilized by methanogens to produce methane – the reason that both gases should be measured in a breath test. In Mary’s case, no such rise occurred, which raised my suspicion for the possible presence of hydrogen sulfide-producing bacteria. Hydrogen sulfide cannot be revealed on a lactulose breath test.
Figure 1. Lactulose Breath Test
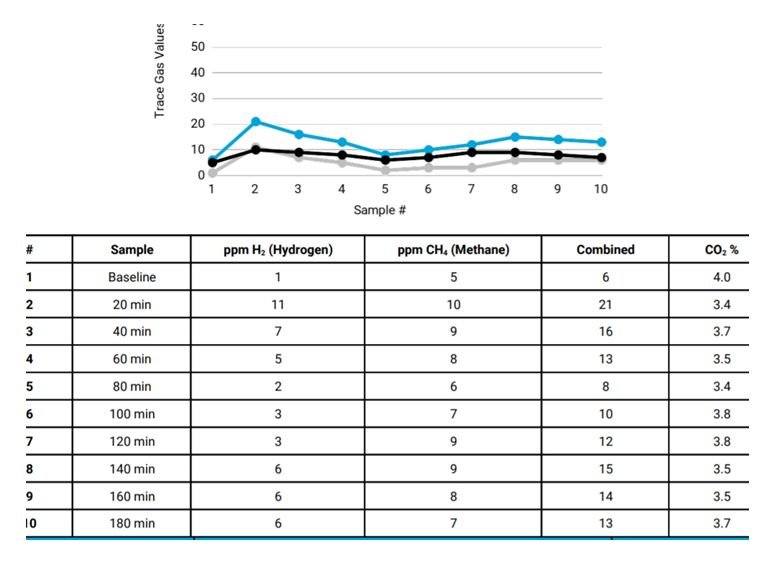
(Blue dots represent methane; black dots represent hydrogen.)
Gut Microbiome Analysis
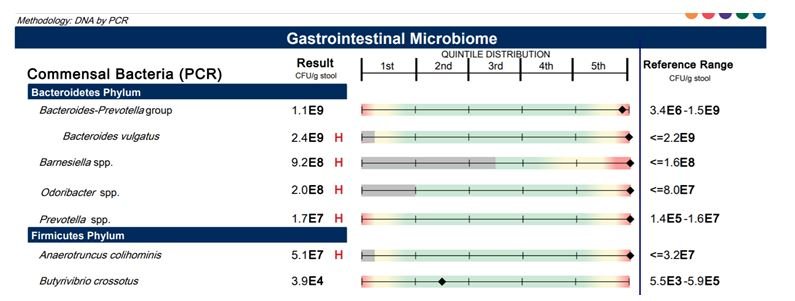
The result of Mary’s stool test was even more revealing. While all digestive and inflammatory markers were within range, the following pertinent abnormalities were found:
- Short-chain fatty acid (SCFA) levels (Figure 2) below detectable levels! I had never seen such an extreme lack of short-chain fatty acids, and wondered if this marker of microbiome health could be responsible for some of Mary’s symptoms, especially the fatigue and body aches. SCFA have been shown to be involved in energy production, prevention of leaky gut and absorption of endotoxin (aka lipopolysaccharide, or LPS), upregulation of mitochondrial function, enhancement of colonic motility, and decreasing systemic inflammation.1,2
Figure 2. Short-Chain Fatty Acids

- Elevated levels of Bacteroides spp (Figure 3). This finding has been associated with reduced bacterial diversity, an inflammatory phenotype, elevated beta-glucuronidase, production of secondary bile acids, and higher adiposity.3
Figure 3. Gastrointestinal Microbiome
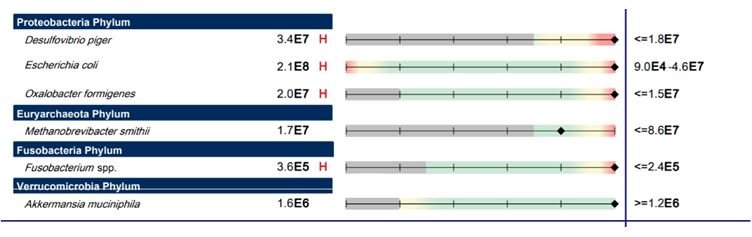
- Elevated levels of Escherichia coli and the hydrogen sulfide-producing bacteria, Desulfovibrio piger (Figure 4). Besides LPS production, higher E coli counts can lead to toxic indole production. Excessive hydrogen sulfide has been linked to colon cancer, abdominal pain, and leaky gut.4,5
Figure 4. Gastrointestinal Microbiome (cont)
Treatment
From the results of Mary’s stool test, it was clear that we needed to change her diet. Bacteroides spp, E coli, and particularly Desulfovibrio, thrive on bile acids and a diet high in animal fat and animal protein.6 Additionally, a diet high in saturated fat (including coconut oil) has been shown to increase the absorption of LPS.9 To reduce harmful bacteria and LPS, and to increase short-chain fatty acids, I recommended a low-fat vegan diet that was rich in high-fiber foods. I also prescribed the following prebiotics:
- Lactulose: This prebiotic has been shown to decrease E coli and Bacteroides spp and to increase beneficial bacteria.7 Lactulose is also the substrate used for SIBO breath testing, so I asked her to start with 5 g daily and to slowly increase it to 10 g, only if no excessive bloating was noted.
- Galacto-oligosaccharides: GOS been shown to minimize growth and production of hydrogen sulfide-producing bacteria, and to increase beneficial Bifidobacterium8
Because green tea has antioxidant and prebiotic effects, I also asked Mary to drink 5-6 cups of green tea daily to further support colonic health. Besides avoiding animal fat and protein, she was also to avoid-sulfite containing preservatives. Lastly, I prescribed zinc chelate, 30 mg 2 times daily, for mucosal/leaky gut support.
Four Weeks Later
Mary returned 4 weeks after starting this simple diet and prebiotic prescription feeling much more energized and optimistic. Her constipation had changed over to 2 normal bowel motions daily, the reflux resolved “on day 1 of the diet,” and gas and bloating and the peri-umbilical pain had resolved. She was sleeping through the night and had days with bursts of energy. Though the aches and pains of fibromyalgia had not yet improved, she was very pleased with this outcome, especially since she had struggled for years with unresolved digestive issues and systemic symptoms.
In SIBO, hydrogen sulfide production has been linked to “rotten egg”-smelling gas, diarrhea, and flatlining hydrogen breath tests. These symptoms were not present in this case, indicating a more complex scenario. Besides Desulfovibrio spp, Bilophilia wadsworthia is also a hydrogen sulfide-producing species, and there is some question about other species. Another question on my mind is whether high sulfur-containing vegetables such as brassicas might contribute to hydrogen sulfide production? And what about sulfur-containing amino acids such as N-acetylcysteine (NAC)?
Though questions remain about an ideal diet to reduce hydrogen sulfide-producing bacteria, this case demonstrates that microbiome-enhancing therapies don’t always have to include probiotic supplementation or antimicrobials. Especially in the case of suspected hydrogen sulfide production, treatment can include a high-fiber, low-fat vegan diet and targeted prebiotic supplementation.
References:
- Canani RB, Costanzo MD, Leone L, et al. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol. 2011;17(12):1519-1528.
- Schwiertz A, Taras D, Schäfer K. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring). 2010;18(1):190-195.
- Wexler HM. Bacteroides: the good, the bad, and the nitty-gritty. Clin Microbiol Rev. 2007;20(4):593-621.
- Medani M, Collins D, Docherty NG, et al. Emerging role of hydrogen sulfide in colonic physiology and pathophysiology. Inflamm Bowel Dis.2011;17(7):1620-1625.
- Singh SB, Lin HC. Hydrogen Sulfide in Physiology and Diseases of the Digestive Tract. Microorganisms. 2015;3(4):866-889.
- Wolf P, Cummings P, Shah N, et al. Sulfidogenic Bacteria Abundance in Colonic Mucosa is Positively Correlated with Milk and Animal Fat Intake and Negatively Correlated with Mono and Polyunsaturated Fatty Acids. FASB J. 2015;29(1 Suppl 598):10.
- Salminen S, Salminen E. Lactulose, lactic acid bacteria, intestinal microecology and mucosal protection. Scand J Gastroenterol Suppl.1997;222:45-48.
- Vulevic J, Drakoularakou A, Yaqoob P, et al. Modulation of the fecal microflora profile and immune function by a novel trans-galactooligosaccharide mixture (B-GOS) in healthy elderly volunteers. Am J Clin Nutr.2008;88(5):1438-1446.
- Lyte JM, Gabler NK, Hollis JH. Postprandial serum endotoxin in healthy humans is modulated by dietary fat in a randomized, controlled, cross-over study. Lipids Health Dis.2016;15(1):186.
Image Copyright: <a href=’https://www.123rf.com/profile_racorn’>racorn / 123RF Stock Photo</a>
 Nirala Jacobi, BHSc, ND (USA), graduated from Bastyr University in 1998 with a doctorate in naturopathic medicine. She practiced as a primary care physician in Montana for 7 years before moving to Australia. Nirala is considered one of Australia’s leading experts in the treatment of SIBO. She is the medical director for SIBOtest, an online testing and educational service for practitioners, and is also the host of the popular podcast “The SIBO Doctor” for practitioners. Nirala is the medical director and senior naturopathic physician at The Biome Clinic, the Centre for Functional Digestive Disorders, in Mullumbimby, New South Wales. Website: www.thebiomeclinic.com
Nirala Jacobi, BHSc, ND (USA), graduated from Bastyr University in 1998 with a doctorate in naturopathic medicine. She practiced as a primary care physician in Montana for 7 years before moving to Australia. Nirala is considered one of Australia’s leading experts in the treatment of SIBO. She is the medical director for SIBOtest, an online testing and educational service for practitioners, and is also the host of the popular podcast “The SIBO Doctor” for practitioners. Nirala is the medical director and senior naturopathic physician at The Biome Clinic, the Centre for Functional Digestive Disorders, in Mullumbimby, New South Wales. Website: www.thebiomeclinic.com