Carbon Dioxide- The Missing Link: Taking a Closer Look at the Connection Between Carbon Dioxide and Stress
Sussanna Czeranko, ND, BBE
As many NDs can attest, the sympathetic nervous systems of their patients are busy adapting to the chronic stressors in contemporary Western culture. Any new natural approaches to deal with this challenge are of strong interest to us. That it is possible to suggest carbon dioxide as “the missing link” in dealing with stress is particularly intriguing. The social and health costs of stress have been well documented, and it is undeniable that stress ranks high on the list of frequent patient visits. The carbon dioxide link between stress and the symptoms of stress is worth a closer look.
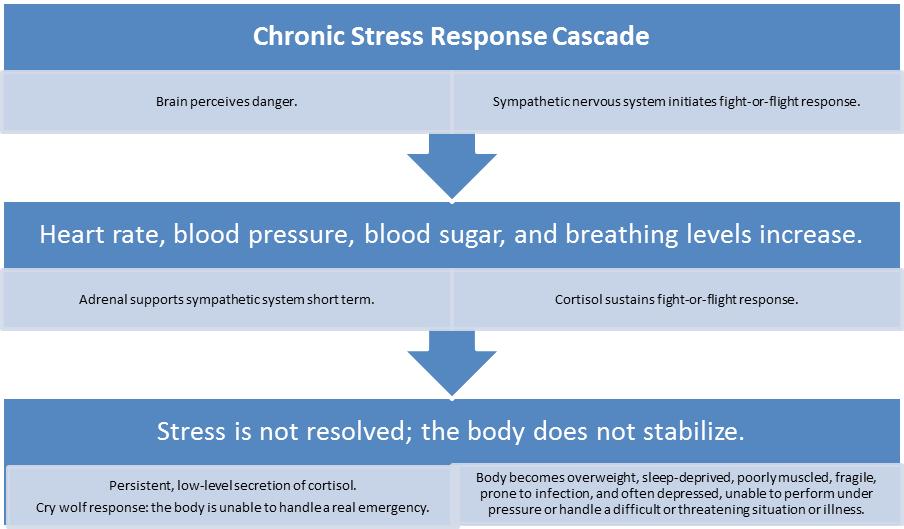
Hans Seyle,1 an early pioneer in modern stress theory, described his “general adaptation syndrome” in 1936, which associated “stages of adaptation” (alarm, resistance, and exhaustion) with changes in hormone patterns and the actual production of “stress hormones.” Our fast-acting sympathetic system enables rapid response by activating and increasing arousal. The pituitary-adrenal system, however, responds more slowly and can even prolong the hyper state of the individual. Bernard and Krupat2 pointed out that, while stress manifests routinely in human survival, prolonged stress can generate adverse health effects.
Naturopathic physicians daily encounter patient presentation in their clinics linked to stress. Unable to keep pace with the exponential avalanche of information, expectation, and obligation, their patients can experience everyday occurrences as stress ridden and even life threatening.
Fight-or-Flight Response, and More…
Our nervous system, uniquely designed to react to danger for self-preservation, preserves deeply in our viscera the same nervous system that hunters-gatherers counted on to save them when lethal danger came. However, many NDs will attest that contemporary humans are, in many ways, far from the same physiological state as primitive healthy men and women on the lookout for tigers or unfriendly clans from the next valley.
Kendall-Reed and Reed suggest in The Complete Doctor’s Stress Solutions that the chronic stress response cascade initiates metabolic syndrome. Very familiar to the naturopathic community, metabolic syndrome is a kind of one-stop shopping cart of serious health conditions parked in a single person, including “obesity [abdominal], high blood pressure, high insulin levels with insulin resistance, diabetes, high cholesterol, and increased risk of heart attack and stroke.”3
Also relevant to our considerations herein is the work of Dr Konstantin Buteyko,4 a Russian medical scientist who spent more than 50 years of his life looking at stress affecting respiration. He observed that unhealthy breathing affected every part of the body. Contending that contemporary humans were experiencing greater difficulty in breathing correctly (ie, modestly and nasally), he identified hyperventilation (or breathing too much) as a symptom of stressful lives and suggested that carbon dioxide (contrary to being a waste gas) is more important than we know.
In 1952, Buteyko4 theorized that alveoli hyperventilation or deep breathing was the cause of “diseases of civilization,” such as allergies and vascular and bronchial spasms. He based his theory on the fundamental laws of physiology, biochemistry, and biology. He postulated that in deep breathing too much carbon dioxide was lost (hypocapnia), causing the alkalizing of blood pH and a leftward shift in the oxygen-hemoglobin dissociation curve (Bohr effect). The deeper the breathing, the more hypoxic were the brain, heart, kidneys, and other organs.
When overbreathing causes an excessive loss of carbon dioxide, respiratory alkalosis occurs. This is followed by the development of metabolic acidosis, which is caused by the accumulation of underoxidized products owing to hypoxia and represents a compensatory reaction against respiratory alkalosis. Buteyko4 postulated that enzymes and hormones dysfunctioned as a result of hypocapnia; he believed that diabetes mellitus was caused by carbon dioxide deficiency and that lack of carbon dioxide leads to spasms of bronchial smooth muscles, brain vessels, heart, intestines, gall ducts, and other organs.
Supporting the findings by Buteyko4 and addressing the benefits of carbon dioxide in dealing with stress, Dr Ray Peat comments:
A quick reduction of carbon dioxide caused by hyperventilation can provoke an epileptic seizure, and can increase muscle spasms and vascular leakiness, and (by releasing serotonin and histamine) contribute to inflammation and clotting disorders. On a slightly longer time scale, a reduction of carbon dioxide can increase the production of lactic acid, which is a promoter of inflammation and fibrosis. A prolonged decrease in carbon dioxide can increase the susceptibility of proteins to glycation (the addition of aldehydes, from polyunsaturated fat peroxidation or methylglyoxal from lactate metabolism, to amino groups), and a similar process is likely to contribute to the methylation of histones, a process that increases with aging. Histones regulate genetic activity.5
He adds:
The therapeutic effects of increasing carbon dioxide are being more widely recognized in recent years. Even Jane Brody, the NY Times writer on health topics, has favorably mentioned the use of the Buteyko method for asthma, and the idea of ‘permissive hypercapnia’ during mechanical ventilation, to prevent lung damage from excess oxygen, has been discussed in medical journals. But still very few biologists recognize its role as a fundamental, universal protective factor. I think it will be helpful to consider some of the ways carbon dioxide might be controlling situations that otherwise are poorly understood.5
Because the curricula in our contemporary naturopathic education programs do not emphasize breathing in the way our elders once did, it may be useful to pause here to review what we know about breathing itself. It is widely held in the profession that our body is designed to take in about 10 to 12 breaths/min. The regulation of respiration is determined by 3 groups of neurons located bilaterally in the medulla oblongata and pons. The dorsal respiratory group mainly causes inspiration; the ventral respiratory group effects expiration, and the pneumotaxic center controls the rate and depth of breathing. The rhythm of normal breathing is controlled by the nervous signals that are transmitted to the inspiratory muscles, mainly the diaphragm, which occur in a steady ramp manner for about 2 seconds. Expiration is initiated when the inspiratory signals stop abruptly during the next 3 seconds for the inspiratory muscles to relax and for expiration to occur.6,7 Breathing is regulated to maintain a stable Pco2 and pH within the systemic arterial blood and to prevent significant hypoxemia.6 Current knowledge attributes carbon dioxide as an essential component in pH homeostasis. Yale University (New Haven, Connecticut) applied physiology professor Yandell Henderson considered carbon dioxide as a “chief hormone of the entire body; it is the only one that is produced by every tissue and that probably acts on every organ.”8
When we see patients with symptoms of multiorgan system disease, we tend not to think of dysfunctional breathing as a possible cause. Breathing is relegated to respiratory diseases, and breathing exercises often do not benefit from the clinical relevance and currency of research, such as that by Buteyko,4 Peat,5 and others. When we consider the purpose of respiration, we think of inhaling as much oxygen as possible because of its vital role in metabolism and because of misconceptions about carbon dioxide, referenced earlier.
In our efforts to address the complexities of multiple symptoms and disease patterns erupting from stressful origins, we prescribe multiple remedies or perhaps even diaphragmatic deep breathing. It is useful for the contemporary ND to consider another strategy and highlight what a difference it makes when we change our focus in solving a problem. But first, let us delve into the world of respiration.
Carbon Dioxide as a Waste Gas? NOT!
We hardly think of carbon dioxide as being so important as it is. Our perception, supported by current medical paradigms and the use of oxygen treatment for so many conditions in the critical care unit, galvanizes the belief that oxygen is gold and that carbon dioxide is superfluous. The concept of carbon dioxide being nonessential was first voiced by Antoine-Laurent Lavoisier (1743-1794). His work on carbon dioxide demonstrated the parallels between combustion of fire and human respiratory metabolism (both needed oxygen, and both generated carbon dio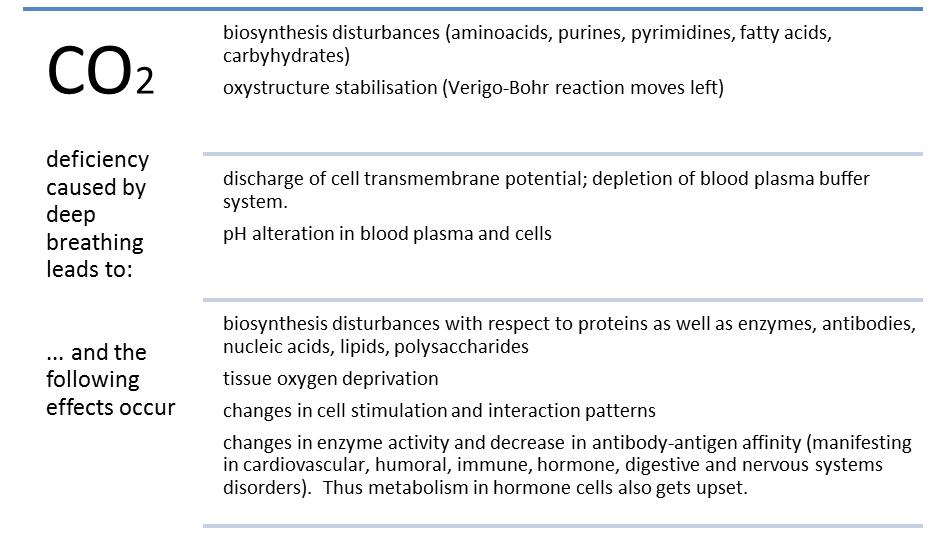 xide and heat). His admonition (still virtually gospel in academia and gymnasiums across the land) that oxygen is the bearer of life and that carbon dioxide is a waste gas has affected our understanding of carbon dioxide significantly. Nothing could be further from the truth. It seems that Lavoisier’s stamp on carbon dioxide as a waste gas in fact has become one of medicine’s greatest misconceptions.8 The importance of carbon dioxide is immense.
xide and heat). His admonition (still virtually gospel in academia and gymnasiums across the land) that oxygen is the bearer of life and that carbon dioxide is a waste gas has affected our understanding of carbon dioxide significantly. Nothing could be further from the truth. It seems that Lavoisier’s stamp on carbon dioxide as a waste gas in fact has become one of medicine’s greatest misconceptions.8 The importance of carbon dioxide is immense.
From notes of “To the theory of diabetes mellitus pathogenesis: basic principles of the hormonotherapy” by Buteyko.4
Stress and Hyperventilation
How stress relates to our breathing patterns and instigates pathologic conditions has been studied with much interest. Although it is undeniable that stress is one of the most important factors in the development of disease today, the ill effects that stress has on human physiological function do not necessarily permeate into treatment protocols. In fact, how medical scientists view stress determines the route taken in dealing with the sequelae. Nowhere is medicine more undecided than when modern technologically propelled biomedicine meets dysfunctional breathing.
Dysfunctional breathing is distressing to the patient and is expensive if left untreated.9 As stated by Magarian et al, “Stress is often associated with a hyperadrenergic state that is known to provoke hyperventilatory responses.”10(p733) Hyperventilation is defined as a “condition in which minute ventilation exceeds metabolic demands, resulting in hemodynamic and chemical changes,”11 which acutely leads to a reduction in the level of arterial Pco2 (hypocapnia).12 Hyperventilation acts by blowing off excessive quantities of carbon dioxide, producing respiratory alkalosis that can affect any part of the body, with a wide range of symptoms.13,14
Acute hyperventilation attacks occurring under acute stress are unmistakable, and the standard treatment of breathing into a paper bag as a quick remedy is well accepted. Chronic hyperventilation is not as easily recognized and is often overlooked, missed, or ignored in diagnostic workups. The reason is multifactorial. For example, the absence of conspicuous overbreathing and shortness of breath is often overshadowed by the patient’s visible anxiety and panic.15 Another difficulty in accepting hyperventilation as a disease stems from the long history in which so many names have been given to its symptoms. Chronic hyperventilation was first recognized by J. M. Da Costa during the Civil War, with soldiers out of breath, annoyed with dizziness, and experiencing palpitations and chest pain.16 The association of hyperventilation and chest pain with extreme effort and disorders of the heart and circulation was acknowledged in the names subsequently ascribed to it, such as vasomotor ataxia, soldier’s heart, and effort syndrome.16
Lum described the symptoms experienced by persons with chronic habitual hyperventilation as a complex “fat folder syndrome” because patients would “present with symptoms relating to virtually any organ or system, suggesting, for example, thyroid, cardiac, gastrointestinal, respiratory or central nervous system disease, leading to much fruitless investigation and the accumulation of a dossier more remarkable for size than for clinical relevance.”17(p1) Naturopaths are all too familiar with patients who come in with normal laboratory test results, multiple and complicated case presentations, and a long list of specialists they have seen. We often happen to be at the end of their desperate search for relief.
For most patients who seek medical care, stress is a big factor. The role of carbon dioxide in governing the activity of the nervous system is vital, and when there are marked fluctuations in carbon dioxide level, disturbances in the autonomic nervous system ensue. When arterial carbon dioxide level drops, carbon dioxide rapidly leaves nerve cells, causing the intracellular pH to rise.16 There is a concomitant increase in neuronal activity and more motor and sensory hyperirritability, with tenseness, tremors, or tetany and numbness or pins-and-needles sensations. Cluff details: “The speed of somatic motor reflexes (e.g. pupillary and knee jerks) is increased and there is a selective depression of the parasympathetic system so that the clinical state of the patient reflects sympathetic dominance, i.e. hyperactivity, tension, emotional sweating and instability, and various visceral disturbance of heart, gut and bladder,”18(p856) which were observations shared by others.19 Essentially, a disturbance in carbon dioxide level leaves no organ system in the body untouched.
Early proponents of hyperventilation syndrome (HVS) saw overbreathing as the problem that needed to be addressed. Hyperventilation and mental stress produced coronary spasms, which are often linked to cardiac pain.20 Because many overbreathers found themselves in emergency departments with symptoms mimicking heart attacks, one group of physicians counseled that “failure to recognise this role of hyperventilation is an error: its neglect prevents a rational approach to the dynamic factors that are capable of reducing the coronary circulation,…it invites a needlessly high surgical referral rate,…and takes away the possibility of dealing with a major cause of illness behaviour after myocardial infarction….”21(p) The management of chronic HVS has found alleviation of symptoms with the use of β-blockers, which depress ventilation via central mechanisms and by suppression of peripheral chemoreceptor drive. These effects may account for the increased Paco2 observed in hyperventilating patients treated with β-blockers, thereby reversing some of the clinical manifestations of hyperventilation.19
Although β-blockers and other medications can control hyperventilation symptoms, another strategy with equally if not superior outcomes is the use of breathing exercises to address the symptoms of HVS. Patients are often reluctant to take drugs that may be associated with adverse reactions and poorer quality of life. The use of breathing exercises to treat hyperventilation has been well documented.22,23
What Is a Healthy Normal Respiration Rate?
Respiration rate is an important indicator of a person’s health but often is not even observed or recorded in the acute hospital ward when the patient’s primary problem is a respiratory condition.24 In discussing the normal respiration rate with nursing colleagues, I was told that fewer than 18 breaths/min was considered slow feeble breathing and that administration of medications would be withheld until breathing normalized. Fieselmann et al25 reported that a respiration rate higher than 27 breaths/min was the most important predictor of cardiac arrest in hospital wards. If a rate of 27 breaths/min causes alarm, then one needs to contemplate why there is so much variation in defining the healthy normal respiration rate, ranging from 12 to 24 breaths/min in adults at rest and 16 to 25 in older persons.26,27
How persons with chronic hyperventilation breathe is another characteristic that differentiates them from healthy breathers. The diaphragm, shaped like a dome at the inferior end of the thoracic cage, is the primary muscle of respiration. Normally, diaphragmatic breathing is marked by movement of the diaphragm and by little movement of the upper thoracic cage. Cluff states: “Inspiration is the active phase, and expiration is a passive relaxation of the inspiratory muscles.”18 In an individual who hyperventilates, breathing consists of predominantly upper thoracic movement, with little or no diaphragmatic involvement. Breathing is highly erratic, with wide variations in rate and rhythm and punctuated with frequent sighs and forced audible expirations. The erratic breathing characteristic of HVS causes a wildly fluctuating Pco2.18,28
The problem that arises from overbreathing is the excessive elimination of carbon dioxide. As stated by Cluff and confirmed by Lum,23 “A single deep breath may cause a momentary fall of 20-25% in the level of carbon dioxide in the blood, while sustained overbreathing can rapidly drop it to half and maintain it at this level.”18(p855) Magarian et al write: “Hypocapnia and respiratory alkalosis develop rapidly upon onset of hyperventilation and can easily be maintained indefinitely, by nearly imperceptible hyperventilation, such as by taking an occasional deep breath while maintaining a normal respiratory rate.”10(p733) Buteyko4 saw the relationship between hyperventilation and chronic disease. He studied the effects of dysfunctional breathing and developed breathing exercises to correct the outcomes.
Wilkinson and colleagues point out: “
Muscular disorders are to be expected when chronic overbreathing promotes acidosis by depleting the body’s buffer base reserves; it causes loss of potassium and magnesium, retention of salt and water, and abnormality of calcium ionisation.”29(p1577)
With the loss of electrolytes, smooth muscle spasms in the bronchial airways, gastrointestinal tract, reproductive organs, and arterial and coronary vessels are affected by diminished changes in Pco2. For example, hypocapnia affects cerebral blood flow, and the caliber of cerebral arteries is dependent on carbon dioxide. Hypocapnia causes vasoconstriction, resulting in cerebral hypoxia manifested by cerebral blood flow decreases, combined with the oxygen-hemoglobin dissociation curve shifts to the left (Bohr effect). Hypoxia leads to cognitive disturbances, vertigo, faintness, and visual disorders.17,18
When blood glucose level is below the middle of the normal range (ie, <79 mg/dL), the effects of overbreathing are progressively enhanced at lower levels (to convert glucose level to millimoles per liter, multiply by 0.0555). This can be the crucial factor in precipitating panic attacks, seizures, and migraines. To keep blood glucose level in the upper half of the normal range, diet modification is essential to treatment.30 Among 78 patients diagnosed as having chronic hyperventilation, the most common major symptoms during an attack were vertigo and lightheadedness (59%), followed by dyspnea (53%), heart palpations (42%), paresthesias (36%), and nausea (19%).19
In another study, Rosen reports: “In 100 consecutive patients, whose CFS [chronic fatigue syndrome] had been attributed to ME [myalgic encephalomyelitis] or PVS [postviral syndrome], the time course of their illness and the respiratory psychophysiological studies were characteristic of chronic habitual hyperventilation in 93.”31(p761) As well, Neil and Hattenhauer32 have shown that hyperventilation compromises myocardial oxygen supply caused by coronary vasoconstriction, which decreases coronary blood flow, coupled with an increase in the oxygen affinity of the blood in the coronary capillaries (Bohr shift to the left). Furthermore, Freeman and Nixon contend: “As coronary vasospasm is increasingly implicated in angina after myocardial infarction the role of hyperventilation should be considered more often.”33(p851)
In any case, as Bass reports, “Many physicians believe that the hyperventilation syndrome is always secondary to undiagnosed organic diseases.”34(p1387) Voicing his skepticism for the HVS diagnosis, Gardner writes: “Hyperventilation syndrome falls into the shadowy hinterland between physiology, psychiatry, psychology and medicine.”35(p755) The difficulty with hyperventilation, it seems, is to find a place where it fits. Gardner considered hyperventilation a pathophysiological process rather than a disease state, which nullified its usefulness in diagnosis and treatment protocols. The snag with the simplification posited by Gardner and others is that, rather than addressing the problems with overbreathing, the focus to deal with symptoms from overbreathing displaced the importance of the breathing pattern itself. By relegating hyperventilation to a secondary role, the main thrusts of biomedicine have been on establishing investigations, assessments, and treatment protocols centered on the disease, not on the cause. As a result, biomedicine has chosen to tread a more invasive path and to advance technologies that move into the realm of obtuse and unfathomable implications. The pharmaceutical fixes are inundated with adverse effects that are discounted in the name of medical progress and science. Their usual approaches deal with only the symptomological treatment, while disregarding the cause. As NDs, we are quite familiar with the price paid when we settle for treating symptoms of the disease and neglect the unified presentation of the patient and fail to zero in on the underlying cause.
Following from this imperative to get to the root of the problem, Perkin and Joseph comment: “Patients need to be convinced that their symptoms are brought on by forced breathing before they are likely to respond to advice on breathing techniques.”19(p450) Instead of rapid-effect drugs or invasive machines or apparatuses), the naturopathic management of the metabolic consequences of chronic respiratory alkalosis consists of rest, followed by breathing education and restoration of activity at a rate calculated to avoid relapse.29
From certain perspectives, carbon dioxide can indeed be seen as the missing link in dealing with stress. We have explored how depleted carbon dioxide, or hypocapnia, can have a role in altering pH levels, disrupting oxygen delivery to the tissues, and perpetuating stress. Dr Buteyko developed a series of breathing exercises that transformed the lives of more than 100 000 patients he treated. Rather than focusing on the symptoms, he treated the hypocapnia caused by hyperventilation, and the symptoms were dramatically resolved. As NDs working in the trenches of primary healthcare, having tools to deal with stress in our own patients is a persistent challenge as we address the cause and not the symptoms. Here we find one more tool for our naturopathic practice.
 Sussanna Czeranko, ND, BBE, is a faculty member working as the rare books curator at National College of Naturopathic Medicine, Portland, Oregon. She is currently compiling several books based on the journals published by Benedict Lust. In addition to her work in balneotherapy, she is founder of the Breathing Academy, a training program for NDs to incorporate a scientific model of breathing therapy called Buteyko into their practice.
Sussanna Czeranko, ND, BBE, is a faculty member working as the rare books curator at National College of Naturopathic Medicine, Portland, Oregon. She is currently compiling several books based on the journals published by Benedict Lust. In addition to her work in balneotherapy, she is founder of the Breathing Academy, a training program for NDs to incorporate a scientific model of breathing therapy called Buteyko into their practice.
References
- Selye H. The nature of stress. http://www.icnr.com/articles/thenatureofstress.html. Accessed June 30, 2011.
- Bernard LC, Krupat E. Health Psychology: Biopsychosocial Factors in Health and Illness. New York, NY: Harcourt Brace College Publishers; 1994.
- Kendall-Reed P, Reed S. The Complete Doctor’s Stress Solutions. Toronto, ON: Robert Rose Publishing; 2004.
- Buteyko KP. To the theory of diabetes mellitus pathogenesis: basic principles of the hormonotherapy. Inventor Efficiency Expert. 1962;(5).
- Peat R. Protective co2 and aging. 2009. http://www.raypeat.com/articles/articles/co2.shtml. Accessed June 1, 2011.
- Appleyard RF. Respiratory Physiology. Lombard, IL: National University of Health Sciences; 2006.
- Guyton CG, Hall JE. Guyton and Hall Textbook of Medical Physiology. Philadelphia, PA: Saunders, Elsevier; 2011.
- Henderson Y. Carbon dioxide: from the Cyclopedia of Medicine. 1940. http://www.goldenworks.us/buteyko2.html. Accessed June 30, 2011.
- Chaitow L, Bradley D, Gilbert C. Multidisciplinary Approaches to Breathing Pattern Disorders. New York, NY: Elsevier Science Publishing; 2002.
- Magarian GJ, Middaugh DA, Linz DH. Hyperventilation syndrome: a diagnosis begging for recognition. West J Med. 1983;138(5):733-736.
- Kern B, Rosh AJ. Hyperventilation syndrome. 2009. http://emedicine.medscape.com/article/807277-print. Accessed June 30, 2011.
- Shu BC, Chang YY, Lee FY, Tzeng DS, Lin HY, Lung FW. Parental attachment, premorbid personality, and mental health in young males with hyperventilation syndrome. Psychiatry Res. 2006;153:163-170.
- Kerr WJ, Gliebe PA, Dalton JW. Physical phenomena associated with anxiety states: the hyperventilation syndrome. Cal West Med. 1938;48(1):12-16.
- Lum LC. Hyperventilation as a cause of chest pain mimicking angina. Pract Cardiol.1981;7:131-139.
- Magarian GJ. Hyperventilation syndromes: infrequently recognized common expressions of anxiety and stress. Medicine. 1982;62:219-336.
- Freeman LJ, Nixon PG. Chest pain and the hyperventilation syndrome: some aetiological considerations. Postgrad Med J. 1985;61(721):957-961.
- Lum LC. Hyperventilation and anxiety state. J R Soc Med. 1981;74(1):1-4.
- Cluff RA. Chronic hyperventilation and its treatment by physiotherapy: discussion paper. J R Soc Med. 1984;77(10):855-862.
- Perkin GD, Joseph R. Neurological manifestations of the hyperventilation syndrome. J R Soc Med. 1986;79(8):448-450.
- Chauhan A, Mullins PA, Taylor G, Petch MC, Schofield PM. Effect of hyperventilation and mental stress on coronary blood flow in syndrome X. Br Heart J. 1993;69:516-524.
- King JC, Nixon PG. Da Costa’s syndrome or neurocirculatory asthenia. Br Heart J. 1988;59(6):727-728.
- Wang SZ, Li S, Xu XY, et al. Effect of slow abdominal breathing combined with biofeedback on blood pressure and heart rate variability in prehypertension. J Altern Complement Med. 2010;16:1039-1045.
- Lum LC. Hyperventilation syndromes in medicine and psychiatry: a review. J R Soc Med. 1987;80:229-231.
- Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust. 2008;188(11):657-659.
- Fieselmann JF, Hendryx MS, Helms CM, et al. Respiratory rate predicts cardiopulmonary arrest for internal medicine patients. J Gen Intern Med. 1993;8:354-360.
- McFadden JP, Price RC, Eastwood HD, Briggs RS. Raised respiratory rate in elderly patients: a valuable physical sign. Br Med J (Clin Res Ed). 1982;284(6316):626-627.
- Ohio State University Medical Center. Vital signs (body temperature, pulse rate, respiration rate, blood pressure). http://medicalcenter.osu.edu/patientcare/healthcare_services/emergency_services/non_traumatic_emergencies/vital_signs/pages/index.aspx. Accessed June 30, 2011.
- Han JN, Stegen K, Simkens K, et al. Unsteadiness of breathing in patients with hyperventilation syndrome and anxiety disorders. Eur Respir J. 1997;10:167-176.
- Wilkinson JB, King J, Nixon PGF. Hyperventilation and neurasthenia. BMJ. 1989;298(6687):e1577. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1836790/pdf/bmj00235-0051a.pdf. Accessed July 2, 2011.
- Lum LC. Treatment difficulties and failures: causes and clinical management. Paper presented at: International Society for the Advancement of Respiratory Psychophysiology, 14th International Symposium on Respiratory Psychophysiology, 2nd Annual Meeting; October 9-11, 1995; Toronto, ON.
- Rosen SD, King JC, Wilkinson JB, Nixon PG. Is chronic fatigue syndrome synonymous with effort syndrome? J R Soc Med. 1990;83(12):761-764.
- Neil WA, Hattenhauer M. Impairment of myocardial o2 supply due to hyperventilation. Circulation. 1975;52(5):854-858.
- Freeman LJ, Nixon PGF. Are coronary artery spasm and progressive damage to the heart associated with the hyperventilation syndrome? Br Med J (Clin Res Ed). 1985;291(6499):851-852.
- Bass C, Gardner WN. Respiratory and psychiatric abnormalities in chronic symptomatic hyperventilation. Br Med J (Clin Res Ed). 1985;290(6479):1387-1390.
- Gardner W. Hyperventilation disorders. J R Soc Med. 1990;83(12):755-757.