Antibiotics & Endometriosis Clinical Observations and Pearls
Justin Gallant, ND, BKin
While taking a thorough health history, I always ask my patients the golden question, “What happened right before this condition came on?” Time and time again, they have responded by saying they were on antibiotics at the time. There seems to be a strong association between antibiotic use and several different conditions, namely autoimmune in nature. Lately, after asking what happened around the onset of endometriosis in my endometriosis patients, I’m getting the same response. Here are some common themes in these patients:
- Patient is diagnosed with Stage 1 endometriosis via laparoscopic exploration
- A strong antibiotic was given before the procedure to prevent infection
- After laparoscopic exploration, the endometriosis worsened to a debilitating state
- Patient is unaware of food-related flare-ups until she charts nutrition and symptoms
- Foods that cause flare-ups include chocolate, citrus, refined sugar, apples
- Patient is addicted to the main food that causes flare-ups
- Patient suffers from chronic constipation and high stress
- Patient has concomitant autoimmune condition
Treatment Protocol
If we can identify endometriosis clinically rather than surgically, we should treat for it accordingly in order to prevent potential further damage caused by antibiotics. If the patient absolutely requires laparoscopic exploration, we should prepare them with probiotics, N-acetyl-glucosamine, and L-glutamine, along with our other standard surgical remedies. We should encourage our patients and their gynecologists to give us at least 2-4 months before they perform laparoscopy.
I recommend the following treatment protocol for endometriosis patients:
- Have the patient keep a nutrition log that correlates symptoms with food
- Get the patient to identify which foods cause flare-ups
- Rule out concomitant autoimmune conditions
- Completely remove these foods from the diet
- Support stress reduction
- Introduce a good quality, multi-strain probiotic
- Introduce proper dosages of L-glutamine and N-acetyl-glucosamine
- If symptoms don’t resolve completely after 2 months, remove dairy and gluten if not already removed
Comments
In my experience with endometriosis, hormonal imbalances have not been consistently present. Although hormonal imbalance should definitely be ruled out, hormone-modulating treatments should not be relied upon if hormones are in balance.
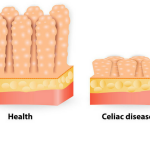
I suspect that our approach to endometriosis should be similar to that of inflammatory bowel disease. Even though endometriosis hasn’t been proven to be autoimmune in etiology, these patterns indicate that this may be the case. In a large 2007 study, anti-endometrial antibodies (ANA) demonstrated positive prediction, negative prediction, sensitivity, and specificity to all be greater than 85% for diagnosing endometriosis.1 In an earlier study, ANA was elevated in 63% of endometriosis patients.2 Perhaps we should explore anti-endometrial antibodies as a marker of endometriosis before relying on explorative surgery.
 Justin Gallant, ND, BKin, graduated from the Canadian College of Naturopathic Medicine in 2012, and has a private practice in Hamilton, Ontario. Prior to receiving his Doctorate of Naturopathy, he received a Bachelor of Kinesiology degree. Dr Gallant maintains an educational blog which receives over 20K views per month. Website: www.DrJustinGallantND.com/blog
Justin Gallant, ND, BKin, graduated from the Canadian College of Naturopathic Medicine in 2012, and has a private practice in Hamilton, Ontario. Prior to receiving his Doctorate of Naturopathy, he received a Bachelor of Kinesiology degree. Dr Gallant maintains an educational blog which receives over 20K views per month. Website: www.DrJustinGallantND.com/blog
References:
- Randall GW, Gannt PA, Poe-Zeigler RL, et al. Serum antiendometrial antibodies and diagnosis of endometriosis. Am J Reprod Immul. 2007;58(4):374-382.
- Malinowski A, Szpakowski M, Wilczynski J, et al. Occurrence of antinuclear antibodies in women with endometriosis and unexplained infertility. Ginekol Pol. 1995;66(7):420-424.