Thermography: A Preventive Screening Tool for Breast Health
Erika Horowitz, ND, MSOM
Breast cancer is the second-leading cause of death among women, behind lung cancer. According to the American Cancer Association, in 2007 an estimated 178,480 new cases of invasive breast cancer will be diagnosed among women, as well as an estimated 62,030 additional cases of in situ breast cancer. In addition, approximately 40,460 women are expected to have died from breast cancer in 2007 (American Cancer Association, n.d.). Epidemiological studies estimate that one in eight women will develop breast cancer during their lifetimes. Moreover, one in five women with breast cancer will die of the disease, despite the considerable advances in treatment (Keyserlingk, 1998). Given these circumstances, early detection of breast cancer is considered an important prognostic factor. There is general consensus that earlier detection of breast cancer can improve survival rates, resulting in a 30%-40% reduction in deaths from breast cancer within 10 years from detection (Roebuck, 1986). Adoption of screening programs has been based on the premise that early detection leads to early treatment, which leads to better survival rates.
Considering the current emphasis on earlier detection, there is an increasing need for better imaging and earlier screening criteria. As NDs, we believe that prevention is the best medicine. With that principle in mind, are there better options for earlier detection of breast cancer? The following is a review of available research on the use of thermography as a screening tool for detecting breast cancer, and its comparison with mammography.
Mammography
Mammography is still considered the “gold standard” for imaging, with clinical examination being the first-line strategy for detecting breast abnormalities. However, there are limitations to both of these modalities.
Mammography has been studied since the early 1960s, and while it has been shown to reduce mortality rates from breast cancer by 30%-40% (Roebuck, 1986), the potential risks of mammography are of recent concern. The question of whether low-dose radiation can cause cancer is the most troublesome. There is evidence that high doses of irradiation cause breast cancer, especially in younger patients (Roebuck, 1986). Other concerns with mammography are tissue compression and the possible spread of cancerous cells by trauma. Contributing factors of variable interpretation and increased tissue density as seen in younger patients and women on hormone replacement therapy make mammography less than ideal.
New techniques in digital mammography show a reduction in radiation compared to film, yet the cost is prohibitive for mainstream use (NCI, n.d.). Current guidelines from the U.S. Department of Health and Human Services (HHS), American Cancer Society (ACS), American Medical Association (AMA) and American College of Radiology (ACR) recommend a screening mammography every year for women beginning at age 40. Women in higher-risk categories are advised to start mammograms earlier and repeat them at more frequent intervals.
It is important to make the distinction that mammography detects anatomical changes and looks at the structure of breast tissue. A mammogram is a soft tissue x-ray of the breast. Mammography shows the variations in density between normal breast tissue and tumors or calcifications, as well as displays the distortion patterns of normal tissue by these lesions (Clark, 1973). Mammograms can detect lesions as small as a few millimeters in diameter, which typically are impalpable. However, a tumor or calcification that is detectable on x-ray is already present in breast tissue by the time a lesion is found. This makes preventive measures impossible to implement.
 Thermography
Thermography
According to the American Academy of Thermology: “… Thermology is the medical science that derives diagnostic indications from highly detailed and sensitive infrared images of the human body. Thermology is sometimes referred to as medical infrared imaging or telethermology, and utilizes highly resolute and sensitive infrared (thermographic) cameras. Thermology is completely non-contact and involves no form of energy imparted onto or into the body. Thermology has recognized applications in breast oncology, chiropractic, dentistry, neurology, orthopedics, occupational medicine, pain management, vascular medicine/cardiology and veterinary medicine” (n.d.).
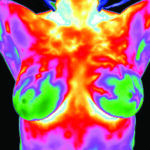
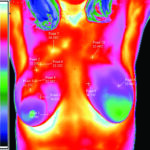
Thermography detects physiological changes in breast tissue and blood flow. Also known as digital infrared thermal imaging (DITI), thermography detects subtle changes by the use of ultra-sensitive infrared cameras to create an image of breast surface temperature. Advanced digital technology is used to detect, analyze and produce high-resolution, diagnostic images of these temperature and vascular changes. Thermography, being sensitive to fluctuations in temperature, detects these changes in the breasts and displays them graphically as variations in color on a thermogram.
According to Dr. Hoekstra, chief thermologist of a clinical laboratory and independent diagnostic reference laboratory certified by the American Board of Thermology: “Thermology interpretative standards necessarily involve a quantitative analysis of the data. An objective analytic system was created in 1975 from the results of studies at Pasteur University in Marseille, France. Termed the Marseille system, this analytic method provides for a TH1-TH5 scale as a summary based upon specific, objective and quantitative thermal features and differential levels of infrared energy. Thermal features are divided into signs and criteria based upon their established characterization of breast disease” (n.d.).
Thermography detection is based on the idea that cancer produces “hot spots” on the surface of skin over a known tumor. Research has shown that malignant change brings increased circulation and heat output. Most breast cancers are hotter than their arterial supply and venous drainage (Clark, 1973). Regional angiogenesis, neovascularization and nitric oxide-induced regional vasodilatation are frequently associated with tumor initiation and progression. The ability of thermography to quantitate minute temperature variations and qualify abnormal vascular patterns indicates its usefulness in early detection and prediction of breast cancer (Keyserlingk, 1998). These heat patterns appear years before the tumor can be detected by mammograms, clinical exams or self-exams. The local temperature elevation produced by a tumor has a correlation with the ultimate prognosis. The hotter the lesion, the greater the degree of malignancy and the worse the prognosis. Research has shown that small tumors frequently exhibit greater heat increases than many of the larger ones. Long-term follow-up suggests that thermograms may provide the first indication of the presence of a malignant tumor (Clark, 1973). However, many benign conditions of the breast as well as carcinoma produce abnormal findings on a thermogram. Hormonal imbalances that place women at greater risk for developing cancer also have characteristic thermal signs. Fibrocystic changes typically show increased vascularization in a more uniform fashion, allowing for effective differentiation between fibrocystic breast disease and tumors. According to the Association for the Advancement of Diagnostic Thermal Imaging: “A woman should get a baseline breast thermography at age 20. Between ages 20 and 30, she should get a breast thermography every three years. Above the age of 30, she should get a breast thermography on a yearly basis. Additional breast thermographies may be performed more frequently for higher-risk women or based on suspicions from prior thermographic examination at the doctor’s discretion” (n.d.).
History of Thermography
Thermography dates back to the 1800s; the first “heat picture” was produced in 1840 by Sir John Herschel. In the early 1900s, infrared research was classified by the military and unavailable for medical application. It was not until 1956 that technical information on thermography was declassified, and in 1961 the first images were used in medical research to confirm that skin temperatures were elevated on the surface of the breast over a cancer (Clark, 1973). A flurry of thermography research was done in the 1970s through the early 1980s, with mixed reviews on its use. Most research was conducted on microscopically confirmed tumors and the comparison between clinical exam, mammograms and thermography in terms of their sensitivity and specificity of detecting tumors. According to the International Academy of Clinical Thermography (IACT): “Breast thermography has been researched for over 30 years, and over 800 peer-reviewed breast thermography studies exist in the index-medicus.” IACT states that in this database “well over 250,000 women have been included as study participants. The numbers of participants in many studies are very large, ranging from 37,000 to 118,000 women. Some of these studies have followed patients up to 12 years. Breast thermography has an average sensitivity and specificity of 90%” (n.d.).
Mammography vs. Thermography
In my review of research, the sensitivity rate for thermography ranges from 70%-90% depending on the type and date of the study. The main drawback of most of these studies is that they compare thermography to mammography, which is comparing apples to oranges. They are each unique in their detection capacities, one measuring anatomy and the other measuring physiology. The incidence of higher false-positive rates for thermography compared to mammography is cited in many early studies as a negative aspect of thermography, leading to conclusions that it is not a viable standalone screening tool (Nathan et al., 1972). Despite this fact, studies show that patients with a false-positive (abnormal) thermogram are at a higher risk of developing breast cancer (Ng et al., 2004).
A recent Canadian study retrospectively reviewed the relative ability of preoperative clinical exam, mammography and infrared imaging to detect 100 new cases of ductal carcinoma in situ (DCIS), stage I and II breast cancer. Palpation was reported to have a sensitivity rate below 65%. Mammography was shown to have an 85% sensitivity rate, and thermography showed an 83% sensitivity. The sensitivity rate increased to 95% when both imaging modalities were combined (Keyserlingk, 1998). This particular study concluded that when done concomitantly with clinical exam and mammography, high-resolution DITI could provide additional safe, practical and objective information (Keyserlingk, 1998).
Advances in breast thermography now make it possible to detect breast cancer, fibrocystic disease, hormonal imbalances, infections and other breast conditions much sooner and with greater accuracy, safety and ease than ever before. There is no one definitive screening test, and they all have their benefits and drawbacks.
To date, a biopsy with a pathology report is the only procedure able to diagnose breast cancer. The current multimodal approach for breast screening calls for clinical examination and thermography followed by an ultrasound or MRI. The ability of thermograms to detect precancerous physiological changes up to 8-10 years before a mammogram makes thermography – with its non-radiation, non-invasive nature and low cost – a useful tool for early screening and prevention. Thermography is especially useful for women who are on hormone replacement; nursing; have had a lumpectomy or mastectomy; or have fibrocystic, large, dense or enhanced breasts. By using basic naturopathic principles of diet, lifestyle interventions and hormone balancing to promote breast health, thermography can be utilized for ongoing monitoring and treatment of breast disease.
 Erika Horowitz, MSOM, ND graduated from NCNM, where she completed a dual degree program. She was awarded the degree of Doctor of Naturopathic Medicine in 2005 and a Masters of Science in Oriental Medicine in 2006. She is a licensed ND in California and a member of both the AANP and CNDA. She is currently practicing in San Francisco at SOMA Acupuncture and Natural Health Clinic as well as in Marin at Naturopathic Family Health Clinic. She practices general family medicine with an emphasis on women’s health and integrative endocrinology.
Erika Horowitz, MSOM, ND graduated from NCNM, where she completed a dual degree program. She was awarded the degree of Doctor of Naturopathic Medicine in 2005 and a Masters of Science in Oriental Medicine in 2006. She is a licensed ND in California and a member of both the AANP and CNDA. She is currently practicing in San Francisco at SOMA Acupuncture and Natural Health Clinic as well as in Marin at Naturopathic Family Health Clinic. She practices general family medicine with an emphasis on women’s health and integrative endocrinology.
References
American Academy of Thermology: www.americanacademyofthermology.org.
American Cancer Association: Breast cancer facts and figures 2007-2008, www.cancer.org.
American College of Clinical Thermology: www.thermologyonline.org.
Clark RM: An approach to the detection and management of early breast cancer, CMA Journal 108:599-606, 1973.
International Academy of Clinical Thermography: www.iact-org.org.
Keyserlingk JR: Infrared imaging of the breast: initial reappraisal using high-resolution digital technology in 100 successive cases of stage I and II breast cancer, The Breast Journal 4:4 245-251, 1998.
Nathan BE et al: Value of mammary thermography in differential diagnosis, British Medical Journal 2:316-317, 1972.
National Cancer Institute: Digital mammography, www.cancer.gov.
Ng E, Sudharsan NM: Computer simulation in conjunction with medical thermography as an adjunct tool for early detection of breast cancer, Bio Med Central Cancer 4:17, 2004.
Roebuck EJ: Mammography and screening for breast cancer, British Medical Journal 292:223-226,1986.
Therma-Scan: www.thermascan.com.










