Irregular Menstruation: Overview and Case Studies
Marie Rodriguez, ND
Many women report getting periods early, late or even skipping a period altogether during times of greater stress – a move, travel, new job, etc. Irregular periods can affect up to 20% of women, and are often harmless. It is when a woman reports never having a regular period or begins to experience irregularity more frequently that a deeper investigation into underlying causes is warranted.
Regular menstruation results from a complex hormonal interaction among the hypothalamus, pituitary and ovaries. It is a sign that the female body is producing appropriate levels of hormones in a balanced manner according to a rhythm that is optimal for reproduction. A textbook period happens every 24-29 days, but cycles varying from 23-35 days are common.
Factors for Irregular Menses
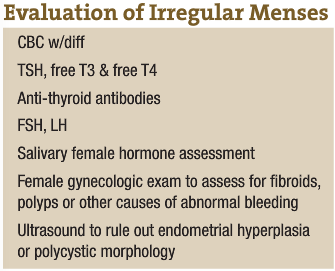
Causes of irregular menstruation are numerous and diverse, ranging from some common hormonal imbalances to lesser-known etiologies. For this reason, a thorough evaluation is needed to define underlying causation. (See the Evaluation of Irregular Menses box for details.)
The hormonal imbalances involved in perimenopause and those resulting from hypothyroidism are two common causes of irregular menstruation. Polycystic ovarian syndrome (PCOS) must be investigated in women afflicted with irregular menstruation. This disorder affects 6%-7% of reproductive-age women, making it the most common endocrine disorder in this population. It is characterized by chronic anovulation and hyperandrogenism. With PCOS, the ovaries produce a quantity of follicles that generates high levels of estrogen, but never release an egg.
In addition, significant weight gain or loss, intense exercise, smoking and medications can contribute to menstrual irregularity. Sudden weight loss or intense exercise reduces body fat and estrogen levels, which may result in anovulation. Poor nutrition, stress and a variety of negative emotions can alter the hormone cascade necessary for optimal hypothalamic-pituitary-ovarian axis function and optimal cycling.
Systemic candidiasis can play a role in irregular menses. Candida albicans secretes human-like hormones that generate the release of anti-ovarian and anti-thymic antibodies.
Structurally, if the uterus is not in optimal position within the pelvic cavity, it may pull on ligaments and surrounding tissues, compromising blood flow, lymphatic flow and nerve transmission to the ovaries. This can result in inconsistent ovulation and irregular menstruation.
Modern lifestyle may influence the periodicity of women’s menstrual cycles. Stress, over-stimulation and toxicity are some of the factors that can disrupt the delicate orchestra of hormones that influences periodic cycling.
In older times, women lived much closer to nature and fulfilled societal roles that had them living in close community with one another. Women’s tissue fluid levels (and hormonal levels within the tissues) are under the same lunar influence as the ocean tides. Women cycled together – ovulating with the full moon and menstruating with the new moon. At the time of the new moon, women ceremoniously left their work in the community and took time to rest together – drinking herbal teas, eating nourishing food and applying healing treatments to one another.
What a stark contrast to modern times, when the menstrual cycle is regarded as an inconvenience. There are birth control methods that can prevent women from cycling altogether! Perhaps irregular menstrual cycles are a reflection of our disconnection from the earth. Throw in modern-day stressors, toxic exposures and nutrient deficiencies … It is no wonder that women experience irregular cycles.
Case Study 1
CW, a 25-year-old law student, reported experiencing extreme stress, anxiety and mood swings exacerbated by PMS. CW was unhappy in law school and focused on just getting through her final two years. Her family history was significant for mental illness. She had a longstanding history of menstrual irregularity, and reported only having regular periods when she was on birth control pills. She discontinued an oral contraceptive, drospirenone and ethinyl estradiol, two months prior to her appointment with me, and since then had only had one menstruation of 8 days duration. CW described feeling bloated, fatigued, crampy, irritated, angry and generally emotional around the time of her period. She had a suboptimal diet due to a hectic schedule. She reported drinking two cups of coffee a day, but intake was up to six cups a day during exam week. She also drank one caffeinated soda daily.
Initial treatment focused on:
- Relieving PMS, anxiety and low moods with an encapsulated herbal formulation containing Vitex, Angelica sinensis, Passiflora, Taraxacum officinalis and Hypericum perforatum.
- CW was advised to wean herself off coffee and begin an adrenal support formula containing Cordyceps, Rhodiola and Panax ginseng.
- We discussed stress management and reframing negative emotional experiences and reducing self-blame.
- Flower essences were incorporated to help ease hyper-ideation, mood swings and low self-esteem (gorse, gentian, mustard, white chestnut, pine). See the accompanying text for the properties of these essences.
- The patient was given a month-long salivary hormone collection to complete.
Six weeks later, CW had not noticed much improvement in her hormonal symptoms. She was feeling depressed, lethargic, bloated and had no menses after 5 weeks. Pressures at law school had been increasing, and she noticed more and more episodes of self-criticism, especially after an emotionally difficult day. She reported having a depressive “fit” during which she cried on and off for an entire day. The patient also expressed interest in counseling, and she was referred to a local therapist to help her work on her self-esteem, breaking her recurrent cycle of negative thinking and re-framing her interpretation of life events.
CW’s female hormone panel results were significant for increased levels of testosterone, suboptimal progesterone, moderate estrogen dominance and a delayed ovulation around day 24, which could be due to suboptimal HPO axis function secondary to stress.
She was given a single dose of Pulsatilla nig. 1M. Natural progesterone was dosed at 35mg BID days 14-28. She was started on a glandular product to support optimal HPO axis function, and fractionated pectin powder to begin colonic absorption of excess estrogen.
Two months later she had two 21-day cycles – a first in her menstrual history. Her mood swings were much less severe, but she continued feeling depressed and had some breast tenderness.
She was re-dosed with Pulsatilla, this time with a 10M potency. Her progesterone was reduced to 25mg BID days 14-28. She was also given a homeopathic hormone combination to take for emotional PMS days. The remedy contains ascending potencies (6x-200x) of estradiol, estriol, DHEA, testosterone, progesterone, androstenedione and aldosterone.
At her six week follow-up, CW reported her first 4-week cycle, and did not notice any bloating, breast tenderness or cramping. Her moods were more stable and she began noticing when she was moving into periods of cyclic negative thinking. Most importantly, she was able to shift her thinking. She also reported a single episode of negative feelings and irritability, at which point she began taking the hormone combination every hour. Her symptoms resolved within a few hours.
 Properties of Flower Essences
Properties of Flower Essences
- Gorse: encourages a more positive perspective in those feeling hopeless
- Gentian: eases discouragement due to setbacks
- Mustard: brings back joy and cheerfulness when gloom descends for no apparent reason
- White chestnut: encourages a peaceful and calm mind for continuous over-thinking and mental agitation
- Pine: helps to ease guilt and self-blame
Case Study 2
A 31-year-old female, GR, had been diagnosed at age 19 with PCOS via ultrasound and had previously experienced numerous PCOS symptoms: irregular periods, hair growth on her chin, weight gain and acne. At the time of the visit, GR reported not having menstruated in two years. She no longer reported the chin hair growth, but did experience cyclic hormonal symptoms of moodiness, acne breakouts on the chin and carbohydrate cravings. GR was slightly overweight – 129 lbs at 5’2’’ – and had difficulty losing weight despite vigorous exercise. The patient had seen a variety of practitioners for PCOS, had done her own research and had tried various treatments, including a low-carb, Atkins-like diet without success. She was currently on a vegan diet.
Our treatment was multifactorial:
- Adequate protein intake was recommended to support her active lifestyle and exercise routine – 45g daily
- Homeopathic ovarian support remedies were to be taken once weekly as follows: Hypophysinum 200K, 3 pellets SL at next new moon; Folliculinum 200K, 3 pellets SL on day 8; Ovarinum 200K, 3 pellets SL on day 15; Luteinum 200K, 3 pellets SL on day 22; flax oil, 1Tbsp days 1-14 (new moon to full moon); evening primrose oil, 500mg BID (full moon to next new moon)
- A biotherapeutic drainage formula consisting of remedies to support female reproductive function and liver detoxification was given – 5 drops of each of three remedies TID
- Homeopathic organotherapy combination was prescribed for support of the female reproductive system (uterinum, ovarinum: 10 drops BID)
- She was advised to place castor oil packs on the abdominal region nightly, and to begin saliva collection for female hormone panel with new moon
At our second visit two months later, GR was thrilled to report that she had had two menstrual cycles, the second one occurring 28 days after the first. Incidentally, she reported taking the homeopathic ovarian support remedies daily instead of weekly. Her first period was three weeks after our initial visit. She experienced significant fatigue, some muscle weakness with her exercise and cramping. The second period was one week ago – she had no cramping, some bloating.
Female hormone panel results showed:
- Low luteal phase progesterone:estradiol balance (P/E2) ratio of 15 (target range: 20-30)
- Elevated estrogen priming index (quantification of estrogen exposure in target tissues) of 1291 (355-923)
- Normal DHEA at 5 (3-10ng/ml)
- Slightly elevated testosterone at 21 (8-20ng/ml)
Bloodwork – CBC, chem panel, thyroid – all fell within normal limits except:
- MCV elevated at 98mm3
- FSH: LH ratio of 3:1, sometimes indicative though not diagnostic of PCOS
- low chloride at 12mmol/L
- neutrophils elevated
GR was advised to:
- Begin taking electrolytes during or after training to replace chloride loss through sweat. Easy home electrolyte recipe: 1tsp baking soda, ½tsp salt, juice of ½ lemon and maple syrup to taste in 1L filtered water
- Switch from flax oil to 2Tbsp flax seeds daily in the first half of her cycle to encourage removal of excess estrogens
In addition:
- A low-dose, graduated prescription of natural progesterone was given to support her insufficient progesterone levels in the luteal phase, and to help reduce PMS and bloating: 25mg BID days 15-17; 35mg BID days 18-20; 50mg BID days 21-23; 35mg BID days 24-26; and 25mg BID days 27-28.
- Biotherapeutic drainage remedies were prescribed to continue to support regular menstruation, elimination of degenerated cells and hormonal buildup: 5 drops of each remedy TID.
- B12 was prescribed at 2,000µg QD.
- Folic acid 800IU QD was recommended to support muscle energy during workout and treat the slight deficiency that shows up on elevated MCV.
- Finally, digestive enzymes containing bromelain and papain were recommended to be taken away from food to help reduce premenstrual bloating and to treat inflammation/muscle injury from training.
 Marie Rodriguez, ND graduated from Bastyr University in 2002. After graduation, Dr. Rodriguez completed a residency in Seattle focusing on women’s health and hormonal issues. She also completed a year of volunteer work at a free clinic in Nicaragua. Dr. Rodriguez has been in private practice in the District of Columbia for more than four years. She treats a wide variety of chronic conditions in her practice, and has a special interest in endocrinology and women’s reproductive issues. She practices eclectically using nutritional therapy, herbal medicine, biotherapeutic drainage, homeopathy and craniosacral therapy.
Marie Rodriguez, ND graduated from Bastyr University in 2002. After graduation, Dr. Rodriguez completed a residency in Seattle focusing on women’s health and hormonal issues. She also completed a year of volunteer work at a free clinic in Nicaragua. Dr. Rodriguez has been in private practice in the District of Columbia for more than four years. She treats a wide variety of chronic conditions in her practice, and has a special interest in endocrinology and women’s reproductive issues. She practices eclectically using nutritional therapy, herbal medicine, biotherapeutic drainage, homeopathy and craniosacral therapy.
References
Arvigo R: Uterine Health and Fertility Enhancement, Medicines from the Earth annual symposium May 31-June 2, 2008, p. 4-8.
Barron ML: Light exposure, melatonin secretion, and menstrual cycle parameters: an integrative review, Biol Res Nurs July; 9(1):49-69, 2007.
Buttram VC Jr: The immature HPO axis, J Reprod Med Jan; (14)1:21-5, 1975.
Lin HT et al: The impact of self-perceived job stress on the menstrual patterns of Tiawanese nurses, Ind Health Oct; 45(5):709-14, 2007.
McQuade Crawford A: Herbal Remedies for Women. Rocklin, 1997, Prima Publishing, p. 41.
Northrup C: Women’s Bodies, Women’s Wisdom. New York, 1998, Bantam Books, pp. 104-110,144.
Pick M: Irregular Periods. Available online: www.womentowomen.com.
Setji TL and Brown AJ: Polycystic ovary syndrome: diagnosis and treatment, Am J Med Feb; 120(2):128-32, 2007.
Thom D: Biotherapeutic Drainage Using the UNDA Numbers. Portland, 2003, JELD Publications, p. 211-212.
Williams L: Radical Medicine. San Francisco, 2007, International Med. Arts Pub p. 327-28.










