Jacob Schor, ND, FABNO
Emerging research links gut dysbiosis and low butyrate production to myasthenia gravis. This article explores how naturopathic medicine can translate these findings into safe, patient-centered interventions.
Abstract
Emerging research suggests that myasthenia gravis (MG), an autoimmune neuromuscular disorder, is associated with alterations in the gut microbiome and reduced production of the short-chain fatty acid butyrate. Recent studies demonstrate that dysbiosis, fecal microbiota transfer, and impaired regulatory T-cell function are linked to MG pathology, while butyrate supplementation restores immune balance and alleviates symptoms in both human and animal models. Naturopathic strategies to raise butyrate levels—through diet, prebiotics, probiotics such as Clostridium butyricum, and botanicals including curcumin—offer a translational opportunity to integrate emerging science with safe, patient-centered practice. This article reviews current evidence, highlights mechanisms of action, and underscores the importance of clinical judgment and harm minimization as naturopathic physicians consider microbiome-focused interventions for MG.
Introduction — Translating Emerging Science, Minimizing Harm
One of the strengths of naturopathic medicine is our willingness to translate new science into clinical practice with a rapidity rarely seen in mainstream medicine. Fewer defined medical protocols restrain us from experimentation. Two key philosophical underpinnings contribute to our innovative flexibility. First, we think in terms of treating the patient rather than the disease, assuming each individual is unique, and therefore appropriate treatment may vary. The second reason we are less hesitant to innovate is our avoidance of malfeasance; the injunction of ‘primo non nocere’. Concerned about potential adverse drug effects, most naturopaths still rely on simple or compounded herbal extracts and vitamins, totally eschewing pharmaceuticals (or at least my generation of practitioners did). Some rely on ultra-dilute homeopathic preparations to trigger healing responses. Even skeptics who doubt the efficacy of such medicines cannot honestly blame them for adverse reactions. Any hesitation toward adopting new therapeutics is tempered by past experience; few of us have been responsible for adverse reactions in our patients. We can honestly tell patients, “It won’t hurt, but it might help.”
Our focus on the principle of primo non nocere is likely due to the overlap in time of when this principle was first introduced to medicine in the early 1800s and the differentiation of our own profession from the common schools of medicine during that same time era.
What Do We Mean by “Translational Medicine”?
The initial purpose of this article was to share information from recent studies regarding myasthenia gravis and see if this data is adequate for us to translate into tentative suggestions of how we might better aid patients afflicted with the disease.
On the verge of suggesting a ‘new protocol’, I find myself stepping back and pondering the differences between Translational Medicine and what I have been calling naturopathic translational medicine.
Bench to Bedside vs Naturopathic Translation
The term “Translational Medicine” is relatively new, first appearing in a Lancet article by James Geraghty in 1996.1 The concept, however, isn’t. For some decades, the term “bench to bedside” was used to reference the time gap between emerging science and utilization in clinical practice. The goal was to shorten the time interval during which new knowledge could save lives. The goal of Translational Medicine is to shorten that gap, though some might argue that the gap was between new science and making a profit from it.
For mainstream medicine, the turning point in formalizing Translational Medicine and stomping on the gas pedal to accelerate the bench-to-bedside journey was the 2003 NIH Roadmap for Medical Research. Clearly, a lot of enthusiasm has gone into this effort. There are now over a hundred PhD programs offering doctorate degrees in Translational Medicine. This drive is clearly motivated by beneficence, a desire to reduce suffering. As mentioned, some might also suspect that avarice comes into play as drug manufacturers have recognized the potential profit of accelerating the process of bringing new profitable patented drugs to the marketplace. Assuming that natural therapies are not patentable, one distinct difference in naturopathic translational medicine is that it is rarely driven by financial incentives.
Myasthenia Gravis (MG) — Clinical Overview
Let me again try to shift gears and these ruminations and turn our focus to myasthenia gravis (MG). Symptoms of myasthenia gravis were first described in 1672 by the English physician Thomas Willis, when he wrote about a patient with fluctuating muscle weakness that improved with rest.2 We now know that myasthenia gravis (MG) is an autoimmune neuromuscular disorder that causes “…varying weakness and rapid fatigue of the skeletal muscles triggered by the host’s
antibodies against the acetylcholine receptor (AChR) in the postsynaptic muscle membrane at the neuromuscular junction (NMJ).”
Gut Microbiome Links to MG — From Dysbiosis to SCFAs
In 2018, Qiu et al. reported that, like other autoimmune disorders, MG is linked to the gut microbiome and dysbiosis3 “Compared to healthy individuals, the gut microbiota of those with MG was changed in terms of the relative abundances of bacterial taxa, with sharply reduced microbial richness, particularly in the genus Clostridium. The fecal SCFA content was significantly lower in the MG group. The degree of microbial dysbiosis was closely related to the levels of inflammatory biomarkers in the sera of MG patients.”
Evidence Synthesis and FMT Signals
A review paper by Angel Thye et al., published in April 20224, explored this concept further and summarized the data that links dysbiosis with MG. Not only did the microbiome differ in MG patients, but also the microbial metabolites differed, so much so that Thyer’s team suggested that the gut biome and metabolites might be utilized as a tool to diagnose the disease. They considered the possibility that probiotics, prebiotics, and fecal material transplant (FMT) might be therapeutic. Zheng et al.’s experiments, in which they transferred MG symptoms from affected mice to healthy mice via stool transplants, were described.5
Large-Scale Analyses and Directionality
In November 2023, a paper by Su et al. provided compelling evidence6 on the association between an altered gut microbiome and MG. Using data on the microbiomes from 426 MG patients compared with 373,848 controls, Su et al. performed some sophisticated analyses to assess the causal relationship between gut microbiota and MG. The data suggested the direction of causality, that is, what causes what, worked “…in both directions between gut microbiota and myasthenia gravis. We identified specific types of microbes associated with myasthenia gravis, which offers a fresh window into the pathogenesis of this disease and the possibility of developing treatment strategies.”
From Species to Metabolites — The Butyrate Pivot
In recent years, a transition has occurred in how we think about the microbiome; the initial focus was on identifying the specific species of bacteria associated with a disease, as if they were solely to blame and might be targeted for eradication. The interpretation of the situation has shifted to a broader view that asks what bacterial metabolites produced by an individual’s microbiome are associated with a condition and whether such a deficiency leads to disease or whether increasing specific metabolites might be beneficial. It has repeatedly turned out that there are multiple possible microbial ecosystems that may be linked to a condition, but that their common denominator is often the metabolites they produce. In MG research, this shift from bacterial species to metabolites occurred in the Spring of 2024 when research attention focused on low levels of butyrate and their association with MG.
2024–2025 Findings on Butyrate and MG
The idea that by treating gut dysbiosis to raise butyrate production to treat a systemic disease isn’t unique to MG, of course; such a plan should be considered in several autoimmune diseases. A 2025 review of 62 studies (n=3126 patients compared with n=29843 healthy people) reported a decrease in short-chain fatty acid (SCFA)-producing bacteria in patients with autoimmune encephalitis, neuromyelitis Optica, multiple sclerosis, and, to our specific interest here, myasthenia gravis.7
In April of 2024, He et al. announced that butyrate-producing bacteria restored Treg cell function by enhancing differentiation in MG patients through the inhibition of mTOR signaling, leading to the activation of autophagy.8
By June 2024, the website “Rare Disease Advisor” had posted that “Butyrate from Gut Microbiota May Have Therapeutic Effects in AChR MG.”9
A few months later, in November 2024, Sun et al. reported on mouse experiments that showed that by improving the gut microbiota and modulating immune responses, they had successfully alleviated MG symptoms.10
Why Butyrate Matters — Immune & Barrier Effects
Butyrate is a short-chain fatty acid produced by gut microbiota and plays a role in maintaining gut health and immune homeostasis. We’ve known it’s important for a long time. Comprehensive stool analysis tests have reported SCFA and butyrate levels for forty or more years. Using butyrate therapeutically has been tried, but it has been a challenge as oral doses are destroyed by digestion. Some readers will remember that years ago, butyrate enemas were suggested to achieve therapeutic benefit. Unsurprisingly, patient compliance was poor, and the practice was a hard habit to instill in patients. Our retired chemistry professor and now esteemed naturopathic doctor, Dr. Davis Lamson, has been raving about a specific oral form of butyrate whose chemical structure protects the butyrate from digestion and reports seeing significant therapeutic benefits in patients with inflammatory bowel disease.11 Specific product brand names are not mentioned in this venue. The common method to increase butyrate levels is to enhance production by gut microflora via encouraging the growth of butyrate-producing species.
In my opinion, this data appears adequate to start a potential experimental protocol with MG patients. With such patients, we should initially test a stool sample for SCFA levels and specifically for butyrate. If the patient’s butyrate level is below the mean, interventions should be initiated to increase butyrate levels. Testing stool samples poses no risk to the patient.
Most MG patients (>80%) are positive for anti-acetylcholine receptor antibodies (AChR), and so these specific antibodies are commonly used as a diagnostic marker for the disease. These antibodies attack the acetylcholine receptors that are essential for nerves to communicate with muscles, and this leads to muscle weakness and fatigue.
Production of these antibodies is regulated by T cells (Tregs) and MG patients who have impaired Treg function and low Treg numbers. Butyrate maintains Treg populations. Recall that Sun et al showed that butyrate-producing gut bacteria are low in MG patients and that butyrate supplementation enhanced Treg differentiation and resulted in lower antibody levels.
Butyrate will be useful in treating autoimmune disease in general due to several key actions:
- Treg cell regulation: Butyrate promotes the differentiation and function of regulatory T cells (Tregs) that are essential for maintaining immune tolerance and preventing autoimmune responses.
- Anti-inflammatory effects: Butyrate reduces the activation of pro-inflammatory cytokines and dampens the excessive immune response often seen in autoimmune conditions.
- Improved gut barrier function: Butyrate helps strengthen the gut lining, reducing intestinal permeability and preventing the leakage of harmful substances into the bloodstream.
Tregs, Antibodies, and What We Still Don’t Know
In April of 2024, He et al. announced that butyrate-producing bacteria restored Treg cells in MG patients through the inhibition of mTOR signaling, leading to the activation of autophagy.8
The effects of butyrate on MG have been tested in vitro and in vivo in murine models and in more recent studies in MG patients. All suggest butyrate restores Treg function, reducing antibodies. What these studies have not revealed is whether these shifts in Treg cells or antibody levels improve the symptoms of the disease in MG patients.10
Of course, correlation does not prove causation. Autoimmune diseases may lower butyrate through some still unknown mechanism, rather than being the result of low butyrate levels impairing immune function. Even if low butyrate leads to autoimmune disease and MG, human evidence is still lacking that raising butyrate will reverse the disease symptoms. To use a murine analogy, once the trap is sprung, bringing in extra cheese won’t help the poor mouse who triggered the trap.
Yet for the moment, let us assume that more cheese will help.
Raising Butyrate — Diet, Prebiotics, and Probiotics
We know quite a bit about raising butyrate levels. SCFAs are produced through bacterial fermentation of carbohydrates, though most carbohydrates have already been digested and absorbed by the time they reach the large intestine, where these fermenters reside. Thus, SCFA
production requires nondigestible carbohydrates, fibers, and resistant starches to feed the fermentation. Increasing fiber intake helps. Prebiotics, like inulin and fructans, yield SCFA as bacteria consume them. Probiotics that contain specific butyrate-producing strains of bacteria like Faecalibacterium prausnitzii, Anaerostipes, Eubacterium, and Roseburia are now being introduced to the market.12 Low levels of these bacterial species are associated with specific diseases. For example, Roseburia is associated with colorectal cancer and inflammatory bowel disease. Various studies are suggesting using butyrate-producing probiotics to treat or prevent a range of diseases. As these specific probiotics are not yet widely available, another option is to regularly consume resistant starches to increase butyrate production.
Dietary Fiber & Resistant Starch (Potato Starch)
Assuming you have found low butyrate in the stool sample of an MG patient, the simplest and safest intervention would be to make dietary recommendations to raise butyrate production. Increased fiber consumption, in particular resistant starches, will make its way to the large intestine and provide ready food for butyrate-producing microbes. Repeating stool butyrate measurements to gauge the impact would seem appropriate. Compliance with such recommendations may be hard for some patients, and some may be impatient and want a pill to fix the situation.13
To increase butyrate production by the gut microbiome:
Increase Fiber Intake:
Eat prebiotic-rich Foods, whole grains, legumes, fruits, vegetables, resistant starches, high polyphenol foods, and cool cooked starches before eating them. The easiest but probably inadequate dietary change might be to eat more chocolate, as it is high in polyphenols.
Potato starch, a resistant starch, raises levels of butyrate by increasing the growth of butyrate-producing bacteria and giving them an ideal food source. [The product used in this research was Bob’s Red Mill potato starch.] Thus, a specific intervention could be to add potato starch to the diet, mixing a spoonful or so into yogurt or applesauce. For those more skilled in the kitchen, it adds a nice touch to baked goods such as muffins or cookies. Too much at a time or in a day will cause excess flatus, so dose to “bowel tolerance.”
Botanicals (Turmeric) — Preclinical Signals
In mice, feeding them turmeric supplements increases butyrate levels and reduces MG symptoms. This was first reported by Wang et al in 2018 and confirmed by Sun et al. in 2024.15
Clostridium butyricum (CBM588) — A Butyrate Producer
A more established strategy to increase butyrate levels is a specific oral probiotic called Clostridium butyricum. It was first isolated in 1933 in Japan by Dr. Chikaji Miyairi from human feces. However, the bacteria currently used were isolated in 1963 from a soil sample in Japan and are sold as Clostridium butyricum Miyairi 588 (CBM588). This product has been sold for decades in Japan, China, and other Asian countries. It has also been approved for use in Europe. It can be purchased through eBay or Amazon.
What sets this clostridial species apart from related species is that it produces butyrate. The other thing that sets them apart is their lack the toxin toxin-producing genes, common in the genus. CBM588 may be familiar, as it’s the probiotic that increases response rates to cancer immunotherapy and extends cancer survival times.16
Clinical Judgment, Safety, and Ethical Transparency
Choosing therapeutics to enhance butyrate production in MG patients would be congruent with the principles of naturopathic medicine: treating the cause, but I don’t think I need to point that out.
There is an additional piece of information to fit into this puzzle of MG and immune function: a paper by Kylie Fletcher et al. published in June 2025.17 She and her colleagues have been tracking the frequency and intensity of adverse effects experienced by cancer patients (N=135) with autoimmune disease who are undergoing treatment with checkpoint inhibitors. They report that exacerbations of underlying autoimmune disease were more common in MG patients than in any other autoimmune disease. This is of interest as CBM588, as mentioned, is garnering some attention for its potential benefit as an adjunct during this form of cancer therapy.18 Putting these two ideas together might lead one to hypothesize that MG patients are particularly deficient in butyrate and that this impairs their immune regulation and worsens their chances of responding poorly to treatment.
Is there a risk to increasing butyrate? High butyrate levels can be seen in patients with bacterial overgrowth in their intestines. We would not want to increase fiber or encourage further overgrowth of these bacteria, so a careful consideration of the patient’s GI symptoms would be appropriate. Elevated butyrate levels are not known to cause any disease.
Discussions of the ethics of Translational Medicine in the literature focus on issues of patient autonomy and informed consent; often, proposed treatments are risky, and an honest practitioner needs the patient to know they are enrolling in an experiment that is potentially dangerous. We, too, must honor our patients’ autonomy and present them with our rationale for a suggested therapy, especially one that is experimental, and give them a free choice whether to try it or not. This is where we use that line, “It won’t hurt and might help.”
What doesn’t get mentioned in ethical discussions regarding Translational Medicine is the spectrum of possible motivations behind the effort. While the obvious reason to move new science into patients’ hands is one of compassion and kindness, the less spoken about motivation, which turns this process into a race to be first, is avarice. New drugs, especially for difficult-to-treat diseases, can be profitable; it is known that some people strive hard to be rich.
Obviously, few of the therapeutics in a naturopath’s medicine cabinet are patentable. If eating more fiber reduces MG symptoms, no one will get rich from knowing this. Nevertheless, being clear with your patients about any conflict of interest is ethically appropriate.
Data Sharing and Professional Learning
There is also an ethical obligation to share our experience and data when we ‘experiment’ with a new approach to disease treatment. At this point, we have limited ways to do this, and an effort should be made to establish such a mechanism that is readily accessible to the profession.
English physician Thomas Willis provided the first description of what is now known as myasthenia gravis, detailing a patient with fluctuating muscle weakness that improved with rest:
“… though they are well in their stomach, and have a good and laudable pulse and urine, yet they are as if they were enervated, and cannot stand upright, and dare scarce enter upon local motions, or if they do, cannot perform them long: yea, some without any notable sickness, are for a long time fixed in their Bed, as if they were every day about to dye; whilst they lie undisturbed, talk with their Friends, and are chearful, but they will not, nor dare not move or walk; yea, they shun all motion as a most horrid thing … in the morning [they] are able to walk firmly, to fling about their Arms hither and thither, or to take up any heavy thing, before noon the stock of Spirits being spent, which had flowed into the Muscles, they are scarce able to move Hand or Foot.”2
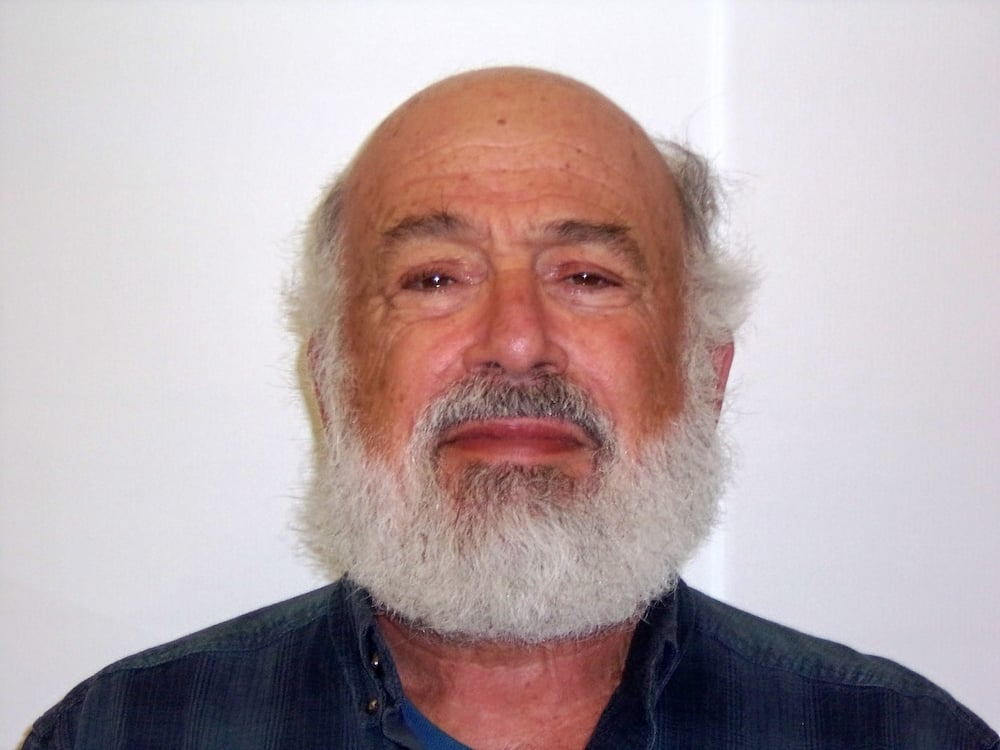
Jacob Schor, ND, FABNO, A graduate of the National College of Naturopathic Medicine (1991), Dr. Schor co-founded the Denver Naturopathic Clinic, where he practiced for nearly three decades with a focus on integrative oncology. He has been a Fellow of the Oncology Association of Naturopathic Physicians (FABNO) since 2008 and is a past president of the organization. Dr. Schor has also served on the board of the American Association of Naturopathic Physicians and was the first recipient of its Vis Award. He is an associate editor of the Natural Medicine Journal and a regular contributor to Townsend Letter, Naturopathic Doctors News and Review, and Integrative Medicine: A Clinician’s Journal. Dr. Schor retired from clinical practice just prior to the COVID-19 pandemic and now lives in Maine with his wife, Dr. Rena Bloom.
References
- Geraghty, J. (1996). Adenomatous polyposis coli and translational medicine. The Lancet, 348(9025), 422. https://doi.org/10.1016/S0140-6736(05)65033-6
- Keynes, G. (1961). The history of myasthenia gravis. Medical History, 5(4), 313–326. https://doi.org/10.1017/S0025727300027278
- Qiu, D., Xia, Z., Jiao, X., Deng, J., Zhang, L., & Li, J. (2018). Altered gut microbiota in myasthenia gravis. Frontiers in Microbiology, 9, 2627. https://doi.org/10.3389/fmicb.2018.02627
- Thye, A. Y., Law, J. W., Tan, L. T., Pusparajah, P., Ser, H. L., Thurairajasingam, S., … Chan, K. G. (2022). Exploring the gut microbiome in myasthenia gravis. Nutrients, 14(8), 1647. https://doi.org/10.3390/nu14081647
- Zheng, P., Li, Y., Wu, J., Zhang, H., Huang, Y., Tan, X., … Xie, P. (2019). Perturbed microbial ecology in myasthenia gravis: Evidence from the gut microbiome and fecal metabolome. Advanced Science, 6(18), 1901441. https://doi.org/10.1002/advs.201901441
- Su, T., Yin, X., Ren, J., Lang, Y., Zhang, W., & Cui, L. (2023). Causal relationship between gut microbiota and myasthenia gravis: A bidirectional Mendelian randomization study. Cell & Bioscience, 13(1), 204. https://doi.org/10.1186/s13578-023-01187-1
- Deng, X., Gong, X., Zhou, D., & Hong, Z. (2025). Perturbations in gut microbiota composition in patients with autoimmune neurological diseases: A systematic review and meta-analysis. Frontiers in Immunology, 16, 1513599. https://doi.org/10.3389/fimmu.2025.1513599
- He, L., Zhong, Z., Wen, S., Li, P., Jiang, Q., & Liu, F. (2024). Gut microbiota-derived butyrate restores impaired regulatory T cells in patients with AChR myasthenia gravis via mTOR-mediated autophagy. Cell Communication and Signaling, 22(1), 215. https://doi.org/10.1186/s12964-024-01215-7
- Murphy, B. (2024, June). Butyrate from gut microbiota may have therapeutic effects in AChR MG. Rare Disease Advisor. https://www.rarediseaseadvisor.com/news/butyrategut-microbiota-potential-therapeutic-effects-mg/
- Sun, J., Chen, J., Xie, Q., Chen, Y., Zeng, H., & Wu, S. (2023). Sodium butyrate alleviates R97-116 peptide-induced myasthenia gravis in mice by improving the gut microbiota and modulating immune response. Journal of Inflammation, 20(1), 37. https://doi.org/10.1186/s12950-023-00377-9
- Singh, V., Lee, G., Son, H., Koh, H., Park, S., Shin, J., … Suk, K. (2023). Butyrate producers, “the sentinel of gut”: Their intestinal significance with and beyond butyrate, and prospective use as microbial therapeutics. Frontiers in Microbiology, 13, 1103836. https://doi.org/10.3389/fmicb.2022.1103836
- Baxter, N. T., Schmidt, A. W., Venkataraman, A., Kim, K. S., Waldron, C., & Schmidt, T. M. (2019). Dynamics of human gut microbiota and short-chain fatty acids in response to dietary interventions with three fermentable fibers. mBio, 10(1), e02566-18. https://doi.org/10.1128/mBio.02566-18
- Sun, C., Zhao, C., Guven, C., … (2020). Dietary polyphenols as antidiabetic agents: Advances and opportunities. Food Frontiers, 1(1), 18–44. https://doi.org/10.1002/fft2.15
- Wang, S., Li, H., Zhang, M., Ma, X., & Huang, H. (2016). Curcumin ameliorates experimental autoimmune myasthenia gravis by diverse immune cells. Neuroscience Letters, 626, 25–34. https://doi.org/10.1016/j.neulet.2016.05.007
- Sun, J., Xie, Q., Sun, M., … (2024). Curcumin protects mice with myasthenia gravis by regulating the gut microbiota, short-chain fatty acids, and the Th17/Treg balance. Heliyon, 10(4), e26030. https://doi.org/10.1016/j.heliyon.2024.e26030
- Riwes, M. M., Golob, J. L., Magenau, J., Hanauer, D., Lee, C. J., & Alousi, A. (2023). Feasibility of a dietary intervention to modify gut microbial metabolism in patients with hematopoietic stem cell transplantation. Nature Medicine, 29(11), 2805–2813. https://doi.org/10.1038/s41591-023-02577-3
- Fletcher, K., Machaalani, M., El Hajj Chehade, R., … (2025). Immune checkpoint inhibitors for patients with preexisting autoimmune neurologic disorders. JAMA Network Open, 8(6), e2513727. https://doi.org/10.1001/jamanetworkopen.2025.13727
- Cazzaniga, M., Cardinali, M., Di Pierro, F., Baldassarre, F., & Fazio, M. (2024). The role of short-chain fatty acids, particularly butyrate, in oncological immunotherapy with checkpoint inhibitors: The effectiveness of complementary treatment with Clostridium butyricum 588. Microorganisms, 12(6), 1235. https://doi.org/10.3390/microorganisms12061235
- Keynes, G. (1961). The history of myasthenia gravis. Medical History, 5(4), 313–326. https://doi.org/10.1017/S0025727300027278
