Phranq D. Tamburri, NMD
Abstract:
A rare Gleason 10 prostate cancer in an 80‑year‑old veteran with a persistently low PSA challenges conventional risk models, highlights the limits of PSA‑based screening, and illustrates how active surveillance, patient personality, and immune resilience can reshape expectations about prognosis.
This case study follows an 80‑plus‑year‑old veteran with biopsy‑proven, gland‑wide Gleason 10 prostate cancer and a PSA that never exceeded 1.4 ng/mL, exploring how this extraordinary presentation exposes the limitations of PSA, refines how clinicians think about “aggressive” disease, and underscores the importance of individualized risk assessment and active surveillance in prostate cancer care.
Introduction:
After 20+ years of specializing in prostate cancer risk assessments I have seen many highly unusual cases, both of overt prostate cancer (CaP) and other cases that were CaP ‘fake-outs’ where BPH and/or prostatitis were the underlying culprits. The latter were of course ‘close-calls’ for the patient that avoided unnecessary severe conventional treatments that many patients would later regret. In even more unusual cases, an auto-immune disease, uncontrolled diabetes, or certain lifestyle choices have pushed a patient’s urologist to the brink of prostatic definitive therapy such as surgery or radiation (and numerous side effects) when in fact CaP turned out not to be the issue resulting in an extremely relieved patient (and his wife!).
The analytical tools to analyze such cases, and to keep your patient’s prostate gland (and their quality of life) from the open maws of the urological medical system, have been outlined in many prior NDNR articles over the many years of this esteemed journal.
(P.S. Congrats to NDNR for their 25th year Anniversary!).
However, one inquiry I often receive from my colleagues is, “What has been the ‘worst’ CaP case you have encountered?!”. Putting aside patients who unfortunately have already been diagnosed with stage 4 metastatic CaP, typically this question infers what had been the “most aggressive” CaP I have seen where Active Surveillance was being considered. This is profoundly important when the naturopath is diligently trying to balance the needs of their patient with the liability obligations of their medical board.
Before we get to Dwight, a tough hombre who stated he would mail me (donate) his prostate “for my fellow medical eggheads to study”, we require a quick review in order to best appreciate this case’s severity, the outcome, and ultimately the professional ‘life lessons’ I learned from Dwight’s remarkable CaP situation!
REVIEW:
Active Surveillance (AS) is technically the management of a patient with a diagnosed CaP from TRUSP biopsy without resorting to definitive treatment (surgery/radiation).1 Although please note that this term is still used, perhaps improperly, for patients who are assumed to have CaP from either a positive DRE, image, or elevated PSA but wish to track it regardless despite refusing a biopsy and hence a ‘legal’ diagnosis.
The prostatic specific antigen (PSA) lab result represents the amount of irritation affecting the prostate. Note that an elevated PSA, typically as long as it remains under 10.0ng/ml, does not specify an extreme CaP risk. In fact, a PSA between 0.00ng/ml to 2.00ng/ml is now considered low CaP risk, between 2.00ng/ml to 10.00ng/ml is intermediate risk, while over 10.0 ng/ml is considered officially overt CaP until proven otherwise.2,3 Nevertheless, the conventional medical system still will flag, often for the wrong reasons, any PSA over 4.0ng/ml.
Lastly, and most importantly, in this review are the slightly loose guideline requirements under the American Urology Association for AS. Although not ‘etched in stone’, the following AUA recommendations are strongly advised and were taught even by myself to my ND students over the years. Note that IF ANY OF THE FOLLOWING ARE ‘FAILED’ BY THE PATIENT then Active Surveillance (AS) is NO longer considered a treatment option for the conventional CaP patient.:
AS LAB REQUIREMENTS:
- PSA under 10.0 ng/ml.4,5
- %free PSA over 10%.6
- Prostatic Acid Phosphatase under 3.5 (or your local lab’s normal value).7
AS BIOPSY REQUIREMENTS:
- Less than 3 cores are allowed to be positive after a standard 12 core random biopsy.8,9
- None of the positive cores may contain more cancer (percentage) than 30% of a core. In fact, even a low aggressive CaP will often be denied AS if even ’31%’ of CaP is found in only one core!8
- ** None of the cores may be an aggressive** Gleason score.10
Besides an exceptionally elevated PSA, this last requirement is probably the most notable for a urologist. It is imperative to remember that ‘aggression’ is not a patient-centric qualitative qualifier of whether their CaP is ‘mean’ or may kill them ‘next Tuesday’. CaP aggression refers to only one metric, period,…the GLEASON SCORE. Currently Gleason Scores, that essentially reflect the mitotic division rate and growth patterns under high powered microscopy field, range from a low of the very common 6 to the highest, and rarest of all, 10.
Gleason 6 is currently considered generally non-fatal and is not typically even conventionally treated.11 Please note that this severity downgrading of Gleason 6 CaP is not from our own naturopathic perspective but is the recent capitulation of the conventional medical establishment toward what NDs and progressive urologists have known for decades…that most men with CaP (that statistically is Gleason 6) die with CaP, not from it. In fact, since 2020, many urologists debate even the very carcinogenic etiology of this variant similar to how current astronomers currently debate whether Pluto is really still a planet or something less such as a planetoid, or a dwarf planet.
Gleason 7, in particular the more common and less aggressive (3+4) low variant (when the first number in parentheses is lower than the second), is where the battle lines are structured amongst urologists currently.12 In fact, similar to the screaming food fight challenges we see today from both sides in America discussing abortion, COVID vaccines, President Trump, or if Olympic figure ice skating is ‘really’ a sport (oi vey!), a low Gleason 7 aggressiveness is equally fraught with debate amongst urologists today.
On average a low Gleason 7 has (depending on the study) about a 1/20 chance of mortality in about 10 (or likely more) years.13 So on one hand, a 72-year-old patient with other co-morbidities such as diabetes and/or CHF could see this level of risk as a ‘gift from the Gods’ and would understandably prefer AS whereas a younger or healthier naturopathic patient may feel differently about these odds. Hence why the ND must relate to their patient’s goals and help determine their priority of quality of life vs longevity.
The typical Establishment urologist who is contracted to see 20-40 patients per day(!) statistically understands therefore that at least 1 or 2 of his daily patients will likely succumb to the Gleason 7 disease. Therefore, the solution to this admittedly relatively low risk Gleason 7 CaP, especially when the physician only has stereotypically 10 minutes with a patient to assess it, is to immediately recommend definitive treatments. This disagreement over a CaP’s pragmatic aggression can even arise from the same medical practice as some will deem a low Gleason 7 as perfectly acceptable to watch and wait (AS) while other urologists feel that any risk for mortality and potential lawsuit demands definitive treatment.
The bottom line is that the bulk of my patients with CaP (and likely yours too) arrive with a likely non-fatal Gleason 6 or low 7 hence why many in the alternative medical fields can easily fall for the trope that “CaP never really kills anyone”. The odds for a more indolent CaP are obviously on our patient’s side yet it is when a more aggressive, or really atypical, CaP shows up in my office that the much harder decisions are made. These next cancers have the ability to shorten the 10+ year CaP post diagnosis typical outcome to under this estimate.
This finally brings us to the realm of the ‘real’ prostate cancers.
Gleason high 7 (4+3) I typically see once every week. These on average increase mortality risk to a 1 out of 15 chance for survival if the patient is actively involved with his situation and being tested quarterly.
Gleason 8, about a 35% mortality in 10 years, I will see once per month.14
Gleason 9, between a 35% to 43% mortality in 10 years, I will see once or twice per year.15,16 (NOTE: President Biden was diagnosed with this form and was immediately put onto comprehensive hormone blockers that made him, like any man, tired and ‘sleepy’).
Gleason 10, 66% at 10 years post-diagnosis. I have only seen this 2-3 times in my entire career. Dwight was the first.
DR. TAMBURRI’S CASE STUDY OF DWIGHT:
I was only 4 years into my fledgling medical practice and my chosen specialty of assessing prostate cancer. The worst CaP I had seen up to this point was a Gleason 9 where the patient had already been properly diagnosed with a clear metastatic case with his PSA over 400.
Not soon after, in walks Dwight.
I must first point out an important (in my ‘professional’ opinion) anecdote which occurred before I even opened his chart. As I was awaiting this new patient, both of my young nurses ran into my office overly excited that my new patient “lit up a cigarette and was smoking in our lobby!”. The senior nurse was even about to call the police. I retorted, “hold the corn, there!, I wish to take a look.” Peeking into my lobby I noticed a slightly hunched 80+ year old Caucasian man. His face and hands were extremely wrinkled and he had swollen eyes…yet he had a look of weathered but fierce resolve on his face. I assessed he was a proud American veteran given his washed-out brown old leather patched bomber jacket with marine patches and a military tan cap. I suggested to my staff that this ‘old timer’ likely had never seen a doctor “since the days when physicians smoked inside hospitals!”. He told me later I was right.
Dwight presented with a confirmed diagnosis of CaP…but a case that at the time I was unprepared for.
- Firstly, his biopsy report discovered prostate cancer positive in ALL 12 cores of the 12 core random biopsy!
- Second, EVERY core was positive for CaP @ 90+% per core!!
- Thirdly, and most striking, EVERY one of the aforementioned cores was diagnosed as a Gleason 10 (5+5)!!!
Furthermore, my routine digital rectal exam (DRE) demonstrated a large, approximately 80cc gland. My prior students may recall that the maximum volume typically represented upon our DRE teaching tools was 80cc. In this case the entire gland palpated extremely hard, irregular, asymmetric, and overall exceptionally nodular… analogous to the nose of the late (awesome) famous actor Karl Malden!
I was gobsmacked with this presentation of a CaP that I had only read about in my urology texts. Like sighting Bigfoot in the woods, these variants are exceptionally rare, “exciting,” and slightly scary when observed. Clearly, as we just reviewed the Active Surveillance criteria above, this case would serve as the antithesis for any AS case as it was a variant that I was conditioned to refer immediately to the allopathic urologist. Yet here this patient sat in my office refusing to ever see another urologist and wanting only supplements and diet going forward! Yet I pressed further, “Dwight, what did your urologist say after he diagnosed you?”. “Well”, he said, “he told me I had 6 months to live.” Only, the biopsy was performed over 6 years prior!
I followed up precariously with, “So, Dwight,…why were you not scared into following your urologists’ conventional suggestions?”. He responded unflinchingly in a style channeling General George S. Patton with a retort that I will never forget. However, for the sake of the NDNR editorial staff I have highly edited it from the colorful metaphors and ‘old school’ military descriptions of America’s prior enemies (yet highly entertaining!). He said, “Sonny…” (yes he called me that), “I served under General McArther. The Japanese tried to kill me. Then ‘Charley’ tried plenty! Uncle Sam has attempted a few times too (the Bikini Island nuclear experiments and Agent Orange in Vietnam). So, this prostate cancer can go f**!#$& $&#*$ %$*# @#@*$&%^ itself!!!”
Yet there was still one more remarkable surprise awaiting for me in this case; Dwight’s PSA had never risen above 1.4!!!
What can we learn from this case?
Well, for my blossoming new prostate cancer practice, there was plenty…
1. How could such an aggressive CaP be missed up until he was 80 years old?: There were 2 reasons. First, he was a patient of the VA system and unfortunately his doctors did not conduct routine DRE’s. However, to be fair, his PSA was so low that there would have been no clinical need to consider CaP. It was detected, ironically enough, due to a medical student who was on shift that day and asked her supervisor if she could gain a coveted DRE ‘check-off. It was this DRE that apparently flagged the urologist who became alarmed and emphatically called for a biopsy and subsequent recommendation to have this gland removed ASAP. Therefore, I learned the necessity to perform a DRE regardless of the PSA.
2. PSA is not always reliable: Of course most physicians currently are aware of the notable unreliability for a PSA and the numerous false positives it can yield.17 However this case represents the ‘definition’ of a PSA INDEPENDENT variant CaP. These are rare variants that may produce PSA from typical prostate cells or even BPH and prostatitis, but the transformation into CaP disables the PSA pathway making these variants essentially camouflaged through typical CaP screening. This would also include the %free PSA.18
Furthermore, not only is this CaP detection on lab work near impossible, but so too would be your PSA tracking following their designated treatments! After all, regardless of your CaP treatment chosen, how would you even know if they were efficacious if the PSA is already ‘normal’? Although my practice is specialized with other tools such as color Doppler TRUSP imaging and molecular testing for such ‘beasties’, this limitation for the typical PCP or even urologist understandably makes AS a nonstarter.
3. The Gleason Score’s conventional medical prognosis is not fait accompli: Being that there are over 1000 (and counting) CaP variations, the Gleason Score is quickly becoming an older overly generalized classification system.19 First off, despite Dwight’s own urologist declaring his prostate cancer specific mortality (PCSM) at 6 months, the true mortality is much more forgiving. As was stated earlier, based on large-scale population studies, the average PCSM for men with newly diagnosed Gleason 10 prostate cancer is approximately 66% at 10 years post-diagnosis. This estimate comes from a 2023 nationwide Swedish cohort study (Prostate Cancer data Base Sweden, covering 2000–2020) although these ranges are never exact depending on the yearly study you choose.
In fact, between you and me dear reader, of the only 3 Gleason 10 cases I have ever encountered, not one of them ever eventually passed from the disease. Now admittedly when I fondly taught my urology class for 23 years I would always make clear that the severity of this variant demanded an immediate referral if the ND or the patient was not perfectly clear over the official lethality risk and how it differs from the typical Gleason 6 that they have likely read about. However, for a patient who is clear about this risk, AS can still be a reasonable option. With proper informed consent and caution, such a case can be undertaken in your practice.
4. ‘Aggressive’ is a medically legal and technical description…it’s not necessarily a pragmatic one: This point is perhaps more involved than this section can allow here however it is worth briefly addressing it. Recall that ‘aggression’ only describes a CaP’s Gleason Score. This score generally breaks down to ‘how many CaP cells are undergoing mitotic division under high powered field’ and is reflected in the 2 different numbers within parentheses whose sum makes up the total Gleason Score. However, this score does not necessarily reflect the chance of mortality. Higher Gleason, mostly seen in patients with a strong familial or carcinogen/radiation history, also suggest a CaP that is more atypical and random than lower Gleason Scores. For instance, it is the higher Gleason’s that show variants with unique traits such as being androgen independent, being located in very rare locations such as the apex over the more common base, and, as seen with Dwight, the infamous PSA independent variant.20,21 Note that none of these traits by themselves dictate higher mortality but, in my professional opinion, atypical cancer behavior compels the practitioner to incorporate this into their patient’s risk assessment. For example, a PSA independent variant does not mean it is not trackable nor treatable. However if the physician is not even aware that this variant exists in his patient then of course mortality risk does notably increase.
5. Surprisingly, a pervasive CaP 12/12 positive core CaP can be LESS of a mortality risk than a newly diagnosed 1/12 positive core!: How? Because a gland wide pervasive CaP often suggests that it has been around for a long time.22 I suspect in Dwight’s case that the CaP had begun during his much younger years, like after he left the military, suggesting it had existed for decades. A CaP this old has had years to move, grow, and explore every ‘nook and cranny’ of the gland including transversing the capsular edge. Yet, like a homebody, the Gleason 10 nevertheless refused to leave the gland! Contrast this to a newly diagnosed much smaller and localized CaP at only one sole location. This second scenario makes me more uncertain about the metastatic risk since I have no idea what ‘personality’ this variant may have nor whether it may bolt ‘out the door’ of the capsule like a captured animal. Recall that a Gleason 10, even a small one, has a mortality of 65% in 10 years. Yet Dwight’s at age 83 had likely been there for many decades…even as a lifelong Camel unfiltered smoker!
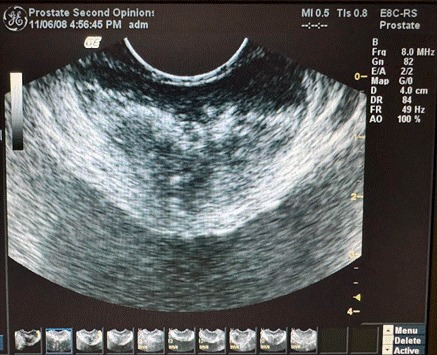
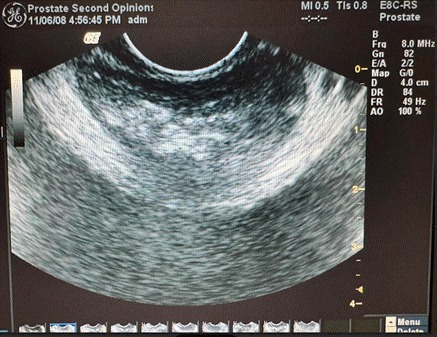
6. CaP and the patient’s immune system can forge a balance or ‘détente’: Even this patient’s trans rectal ultrasound (TRUSP) was informative in that one can see (attached TRUSP image) this gland consumed by both pronounced swaths of hypoechoic (very dark) suspect CaP tissue at the bilateral posterior prostate (the black upper half) that sits in stark contrast to the anterior half which appears completely hyperechoic (the blatant white half) that is likely calcium ‘rock’ often seen as inert scar tissue. Although I do not have a peer review study to confirm this statement, my long experience has observed this dichotomy presentation in numerous ‘pit bull’ patients who have weathered many years (knowingly or not) of a confirmed CaP that remained contained. My sense is that the calcification is an artifact from the battle of the immune system ‘walling off’ or transitioning the active CaP, like Medusa, into literally ‘stone’.
7. I require a pit bull patient to take on a pit bull CaP!: Although this rule is not steadfast it still remains one that helps a good naturopath combine both the personality and aggression of the CaP in equal importance to the personality and aggression of your patient. The reason I spent time in this essay describing the human side of Dwight is because it hopefully illustrates this last rule, the most important one that I learned. In fact assessing these ‘personalities’ is almost 50% of my risk weighting as it helps me assess the viability of CaP cases. You mustn’t approach this however as judgment over your patient but instead from a professional yet compassionate humanist perspective. A patient, after proper education and informed consent, should not be too anxious about learning to live with cancer, a required trait for successful AS. Understandably this may not apply to a patient who had traumatically watched a loved-one suffer from a metastasis, prior successes with the conventional system, or especially if they still have young children at home. Financial ‘aggression’, or how much money they are able to throw at their disease is also a strong factor. Keeping in mind that I typically refer my patients out for aggressive integrative treatments, a man on Medicare could take on a ‘poodle’ CaP with diet and a few supplements such as Serenoa repens. Yet a ‘pit bull’ CaP may require weekly IVs at $220 each for months alone! The patient should understand up front what size ‘mountain’ they are about to climb…and its likely cost. Furthermore, although far from absolute, I also see more confidence in undertaking the AS journey from patients who are extraordinarily religious as they typically do not fear death as more secular patients may. I have often seen this dichotomy over the years. Witnessing how countless patients confront ‘the news’ of their potential mortality instantly while sitting in the couch across from me does play a factor in my assessment but personally has moved me greatly. Interestingly, over 90% of my patients (I ask every one) had never opted for the COVID vaccine which is much higher than the 15% national average. It seems consistent that if a patient refused to take an establishment-endorsed untested drug for a potentially life-threatening virus then they might balk at similar conventional treatments for a cancer.
In conclusion, I hope that one has gleaned from this case study that CaP is not always the ‘Boogey man’ that we were led to believe from the academics. Dwight ended up living another 8 years to a ripe age of 91, passing away in his sleep I was told. Of course, cancer must be taken profoundly seriously for the health and longevity of your patient (and ourselves!). Yet I have learned, as many who work in the world of oncology, to respect cancer…ALL cancer, almost as a separate and unique life form. It mutates, there are unlimited variations / ‘personalities’ of them, and they often develop metabolic ‘super-powers’ to succeed in their combative environment. This perspective has truly changed my approach to what the DIS-ease of cancer may really be about. Yet I will always remember that this first glimpse from ‘textbook’ oncology into the ‘real world’ was myself first gleaned from my meeting with a very special patient, Dwight.

Phranq D. Tamburri, NMD
Dr. Tamburri graduated from SCNM in 2001, Chief Resident until 2023, then taught Clinical Urology at his Alma Mater for for 23 years. He is especially honored to have been asked to regularly contribute to the annual NDNR Men’s Health issues over the past 15 years. Dr. Tamburri has an international practice that specializes in the assessment of prostate cancer (or the risk from elevated PSA) and related disorders.
References:
1) Shill DK, Roobol MJ, Ehdaie B, Vickers AJ, Carlsson SV. Active surveillance for prostate cancer. Transl Androl Urol. 2021 Jun;10(6):2809-2819. doi: 10.21037/tau-20-1370. https://pubmed.ncbi.nlm.nih.gov/34295763/
2) Umbehr MH, Gurel B, Murtola TJ, et al. Intraprostatic inflammation is positively associated with serum PSA in men with PSA <4 ng ml(-1), normal DRE and negative for prostate cancer. Prostate Cancer Prostatic Dis. 2015 Sep;18(3):264-9. doi: 10.1038/pcan.2015.19. https://pmc.ncbi.nlm.nih.gov/articles/PMC4537352/
3) David MK, Leslie SW. Prostate-Specific Antigen. [Updated 2024 Sep 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557495/
4) Chung MS, Lee SH. Current status of active surveillance in prostate cancer. Investig Clin Urol. 2016 Jan;57(1):14-20. doi: 10.4111/icu.2016.57.1.14. https://pmc.ncbi.nlm.nih.gov/articles/PMC4778755/
5) Garisto JD, Klotz L. Active Surveillance for Prostate Cancer: How to Do It Right. Oncology (Williston Park). 2017 May 15;31(5):333-40, 345. https://pubmed.ncbi.nlm.nih.gov/28512731/
6) Loeb S, Bruinsma SM, Nicholson J, et al. Active surveillance for prostate cancer: a systematic review of clinicopathologic variables and biomarkers for risk stratification. Eur Urol. 2015 Apr;67(4):619-26. doi: 10.1016/j.eururo.2014.10.010. https://pmc.ncbi.nlm.nih.gov/articles/PMC4483277/
7) Taira A, Merrick G, Wallner K, Dattoli M. Reviving the acid phosphatase test for prostate cancer. Oncology (Williston Park). 2007 Jul;21(8):1003-10. https://pubmed.ncbi.nlm.nih.gov/17715699/
8) Jones C, Fam MM, Davies BJ. Expanded criteria for active surveillance in prostate cancer: a review of the current data. Transl Androl Urol. 2018 Apr;7(2):221-227. doi: 10.21037/tau.2017.08.23. https://pmc.ncbi.nlm.nih.gov/articles/PMC5911537/
9) Romero-Otero J, García-Gómez B, Duarte-Ojeda JM, Rodríguez-Antolín A, Vilaseca A, Carlsson SV, Touijer KA. Active surveillance for prostate cancer. Int J Urol. 2016 Mar;23(3):211-8. doi: 10.1111/iju.13016. https://pmc.ncbi.nlm.nih.gov/articles/PMC4966658/
10) Van der Poel HG, van den Bergh RC. Difference of opinion – Active surveillance in intermediate risk prostate cancer: is it safe? Opinion: Yes. Int Braz J Urol. 2016 May-Jun;42(3):413-7. doi: 10.1590/S1677-5538.IBJU.2016.03.03. https://pmc.ncbi.nlm.nih.gov/articles/PMC4920555/
11) Carter HB, Partin AW, et al. Gleason score 6 adenocarcinoma: should it be labeled as cancer? J Clin Oncol. 2012 Dec 10;30(35):4294-6. doi: 10.1200/JCO.2012.44.0586. https://pmc.ncbi.nlm.nih.gov/articles/PMC3515766/
12) Bernardino R, Sayyid RK, Leão R, Zlotta AR, et al. Using active surveillance for Gleason 7 (3+4) prostate cancer: A narrative review. Can Urol Assoc J. 2024 Apr;18(4):135-144. doi: 10.5489/cuaj.8539. https://pmc.ncbi.nlm.nih.gov/articles/PMC11034964/
13) Richard PO, Timilshina N, Komisarenko M, et al. The long-term outcomes of Gleason grade groups 2 and 3 prostate cancer managed by active surveillance: Results from a large, population-based cohort. Can Urol Assoc J. 2020 Jun;14(6):174-181. doi: 10.5489/cuaj.6328. https://pmc.ncbi.nlm.nih.gov/articles/PMC7654679/
14) Wright JL, Salinas CA, et al. Prostate cancer specific mortality and Gleason 7 disease differences in prostate cancer outcomes between cases with Gleason 4 + 3 and Gleason 3 + 4 tumors in a population based cohort. J Urol. 2009 Dec;182(6):2702-7. doi: 10.1016/j.juro.2009.08.026. https://pmc.ncbi.nlm.nih.gov/articles/PMC2828768/
15) Zhou Y, Lin C, Hu Z, Yang C, Zhang R, Ding Y, Wang Z, Tao S, Qin Y. Differences in survival of prostate cancer Gleason 8-10 disease and the establishment of a new Gleason survival grading system. Cancer Med. 2021 Jan;10(1):87-97. doi: 10.1002/cam4.3571. https://pmc.ncbi.nlm.nih.gov/articles/PMC7826472/
16) Ham WS, Chalfin HJ, Feng Z, Trock BJ, Epstein JI, Cheung C, Humphreys E, Partin AW, Han M. New Prostate Cancer Grading System Predicts Long-term Survival Following Surgery for Gleason Score 8-10 Prostate Cancer. Eur Urol. 2017 Jun;71(6):907-912. doi: 10.1016/j.eururo.2016.11.006. https://pubmed.ncbi.nlm.nih.gov/27876305/
17) Tidd-Johnson A, Sebastian SA, et al. Prostate cancer screening: Continued controversies and novel biomarker advancements. Curr Urol. 2022 Dec;16(4):197-206. doi: 10.1097/CU9.0000000000000145. https://pmc.ncbi.nlm.nih.gov/articles/PMC9875204/
18) David MK, Leslie SW. Prostate-Specific Antigen. [Updated 2024 Sep 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557495/
19) Li J, Wang Z. The pathology of unusual subtypes of prostate cancer. Chin J Cancer Res. 2016 Feb;28(1):130-43. doi: 10.3978/j.issn.1000-9604.2016.01.06. https://pmc.ncbi.nlm.nih.gov/articles/PMC4779761/
20) Sazuka T, Imamoto T, Namekawa T, et al. Analysis of preoperative detection for apex prostate cancer by transrectal biopsy. Prostate Cancer. 2013;2013:705865. doi: 10.1155/2013/705865. https://pmc.ncbi.nlm.nih.gov/articles/PMC3595663/
21) Zhang Q, Han Y, Zhang Y, Liu D, Ming J, Huang B, Qiu X. Treatment-Emergent Neuroendocrine Prostate Cancer: A Clinicopathological and Immunohistochemical Analysis of 94 Cases. Front Oncol. 2021 Feb 1;10:571308. doi: 10.3389/fonc.2020.571308. https://pubmed.ncbi.nlm.nih.gov/33598420/
22) Ahmed HU, Arya M, Freeman A, Emberton M. Do low-grade and low-volume prostate cancers bear the hallmarks of malignancy? Lancet Oncol. 2012 Nov;13(11):e509-17. doi: 10.1016/S1470-2045(12)70388-1. https://pubmed.ncbi.nlm.nih.gov/23117005/


