Cheryl Burdette, ND
There is an abundance of research that demonstrates the benefits of healthy fats. Omega-3 fatty acids are routinely touted for their ability to help areas of the body that contain fat, such as the brain, myelin sheath, and cell membranes. Much research suggests the importance of fats in cardiovascular disease, but also in other conditions, such as attention deficit disorder. Successful treatment of hyperactivity disorder and other neurologic conditions is also dependent on the health of fats, and on keeping them in a reduced state. Reactive oxygen species are highly damaging to fats and will inhibit their ability to be incorporated appropriately into the places they are needed, such as the central nervous system (CNS) and the peripheral nervous system (PNS).
The Importance of Milieu
Despite the strong body of research, we may give an omega-3 fatty acid or a balance of omega-3s, 6s, and 9s, but not see the desired clinical response. In naturopathic medicine, we are, of course, never merely using a pill for a symptom. We work to change diet and lifestyle habits, and assuming the patient has been compliant in making these shifts, it can be disappointing to add a therapy that seems so well supported by the research, but not see the desired effect in the patient.
Like much of what we see, it is not merely the compound that is important; it is also the environment that the compound – in this case a fatty acid – is in. Even arachidonic acid (AA), usually thought of as an inflammatory fat, can produce symptoms when its concentration is too low. The environment around AA will also dictate how inflammatory it is. AA can become more hazardous to the body when surrounded by free radicals or reactive oxygen species that oxidize it. This inflammation of fats can increase our risk of heart disease and impact the health of the CNS and PNS, which are both dependent on the health of fats.1 From inflammatory fats to healthy fats, if fatty acids are put into an inflamed body, they will predictably become more damaging and be unable to facilitate the clinical improvement often noted in the literature. Evaluating the endogenous environment of our fats has wide-reaching clinical implications for clinical direction and treatment.
F2-Isoprostane
By assessing a fat’s environment with F2-Isoprostane, a marker of oxidative stress, we can better estimate AA’s magnitude of harm or understand why our omega-3 fatty acids are not giving us the benefit we had expected. F2-Isoprostane is a lipid peroxide, similar to TBARS/MDA (thiobarbituric acid reactive substances/malondialdehyde). However, TBARS are a byproduct of lipid peroxidation. The most commonly measured byproduct is MDA, which is only one of many byproducts of lipid peroxidation; MDA is calculated in the lab as an extrapolation of the degree of oxidative stress occurring endogenously. MDA cannot be measured in the blood directly, because we do not create this end-product internally. In contrast, F2-Isoprostane is formed endogenously (Figure 1).
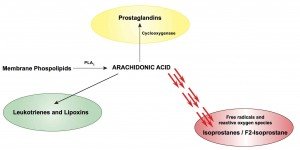
Figure 1.F2-Isoprostane & Oxidative Stress
Another advantage of measuring F2-isoprostane, compared to other markers of lipid peroxidation, is its in-vivo and in-vitro stability. Isoprostanes are detectable in a variety of human tissues and biological fluids, including plasma, urine, lavage fluid, RBCs, and cerebrospinal fluid, with good correlation between tissue and urine.2 However, quantitation of F2-isoprostanes in a random urine specimen is considered to be the most accurate and robust measurement of these circulating compounds.3
Biological Effects of F2-Isoprostane
F2-Isoprostane is thought to be the gold standard for assessing lipid peroxidation, and for many reasons. F2-isoprostanes are produced in abundance in vivo and have demonstrated potency as vasoconstrictors within the vasculature of the heart, brain, lung, and kidneys.4 Generation of F2-Isoprostane induces downstream effects, including proliferation of vascular smooth muscle cells and release of endothelin.5 Additional evidence suggests that F2-isoprostanes may promote aspirin resistance with respect to platelet aggregation.6
F2-Isoprostane can be a useful marker of cardiovascular health. Serum F2-Isoprostane was found to be higher in patients with acute coronary syndrome, and to be an excellent predictor of 30-day increased risk of acute coronary syndrome.7 High urinary F2-Isoprostane indicates increased risk of CHF.8 Lower isoprostanes are favorably associated with an improved ejection fraction, as well as more efficient superoxide dismutase activity.8 F2-Isoprostanes can oxidize LDL lipids, increasing their atherosclerotic capacity. Studies show that those eating a Mediterranean diet – high in antioxidants from olive oil, fruits and vegetables – have lower levels of F2-isoprostane. This may help explain the diminished risk of heart disease associated with this diet.9
Because fats are ubiquitous in the body, oxidation of fats, as reflected by higher F2-Isoprostane, can be associated with symptoms and pathology in many other areas of the body as well. For example, higher levels of F2-Isoprostane in the CSF have been associated with depression and Alzheimer’s disease,10 and higher plasma F2-Isoprostane has been noted in Parkinson’s disease.11 F2-Isoprostane has also been found elevated in the plasma of patients with lupus.12 Higher F2-Isoprostane was associated with greater disease severity, fatigue, and depression, suggesting an oxidative mechanism behind multiple symptoms of lupus. F2-Isoprostane has also been found to be higher in obesity, suggesting an inflammatory component of weight management.13 Other studies have suggested F2-Isoprostane as a risk factor for various cancers, including prostate and breast.14,15 Patients with prostate cancer, who were matched based on Gleason scores, had a higher rate of progression when urinary F2-Isoprostane was elevated.14 As F2-Isoprostane levels increase, so does the risk of breast cancer.15
Using F2-Isoprostane to Guide Treatment
F2-Isoprostane as a marker can help direct many of our therapies, from the use of healthy fats, to hormonal therapies. A decrease in the F2-Isoprostane level indicates a decrease in oxidative stress. As mentioned above, a Mediterranean-type diet can reduce levels of F2-Isoprostane. Compounds from broccoli sprouts and seeds have been shown to effectively decrease F2-Isoprostane; lower levels also track with decreasing deleterious oxidative end-products of estrogen, ie, semiquinones.16 Other antioxidants shown to lower F2-Isoprostane include vitamins C, E and alpha-lipoic acid,17 carotenoids,18 and hydroxyltyrosol in olive oil.19
Summary
F2-Isoprostane is a reliable, affordable, and minimally-invasive biomarker of oxidative stress. This marker correlates with the increased oxidative stress that occurs in cardiovascular disease, depression, autoimmune conditions, and even cancer. Essential fatty acids are critical to the health of many areas of the body, from the brain and myelin sheath, to mitochondrial membranes and the membrane of every cell in the body. They are also essential to hormonal health. When F2-Isoprostane is high, our fats are in an environment of distress, or oxidative stress. By improving levels of antioxidants and decreasing reactive oxygen species, we can improve the environment surrounding our fats, which in turn will improve the function of fats. While F2-Isoprostane is not diagnostic of any singular condition, it is indicative of oxidative stress that contributes too many pathologies and their ability to progress. F2-Isoprostane also gives us a reliable benchmark for improving dosing and outcomes, allowing us to tailor a level of antioxidant to the level functional impact in the body.
 Cheryl Burdette, ND, graduated from Bastyr University in 2001, and completed her residency at Cancer Treatment Centers of America. She practices in Atlanta, GA, at Progressive Medical Center, the largest integrative medicine clinic in the Southeast. Cheryl serves on an IRB, reviewing integrative study designs. She authored a chapter in the book, Laboratory Evaluations in Molecular Medicine, and has published in many journals. Cheryl teaches Clinical Oncology and Nutrition at George Washington University, in a PhD program in Integrative Medicine. As Education Director and owner of Dunwoody Labs, her marriage between clinical practice and laboratory oversight provides her a unique perspective in evidence-based natural therapies.
Cheryl Burdette, ND, graduated from Bastyr University in 2001, and completed her residency at Cancer Treatment Centers of America. She practices in Atlanta, GA, at Progressive Medical Center, the largest integrative medicine clinic in the Southeast. Cheryl serves on an IRB, reviewing integrative study designs. She authored a chapter in the book, Laboratory Evaluations in Molecular Medicine, and has published in many journals. Cheryl teaches Clinical Oncology and Nutrition at George Washington University, in a PhD program in Integrative Medicine. As Education Director and owner of Dunwoody Labs, her marriage between clinical practice and laboratory oversight provides her a unique perspective in evidence-based natural therapies.
References:
1. Montuschi P, Barnes PJ, Roberts LJ 2nd. Isoprostanes: markers and mediators of oxidative stress. FASEB J. 2004;18(15):1791-1800.
2. Milatovic D, Aschner M. Measurement of isoprostanes as markers of oxidative stress in neuronal tissue. Curr Protoc Toxicol. 2009;Chapter 12:Unit12.14.
3. Yin H, Porter NA, Morrow JD. Separation and identification of F2-isoprostane regioisomers and diastereomers by novel liquid chromatographic/mass spectrometric methods. J Chromatogr B Analyt Technol Biomed Life Sci. 2005;827(1):157-164.
4. Montuschi P, Barnes PJ, Roberts LJ 2nd. Isoprostanes: markers and mediators of oxidative stress. FASEB J. 2004;18(15):1791-1800.
5. Strobel NA, Fassett RG, Marsh SA, Coombes JS. Oxidative stress biomarkers as predictors of cardiovascular disease. Int J Cardiol. 2011;147(2):191-201.
6. Davies SS, Roberts LJ. F2-isoprostanes as an indicator and risk factor for coronary heart disease. Free Radic Biol Med. 2011;50(5):559-566.
7. LeLeiko RM, Vaccari CS, Sola S, et al. Usefulness of elevations in serum choline and free F2)-isoprostane to predict 30-day cardiovascular outcomes in patients with acute coronary syndrome. Am J Cardiol. 2009;104(5):638-643.
8. Polidori MC, Praticó D, Savino K, et al. Increased F2 isoprostane plasma levels in patients with congestive heart failure are correlated with antioxidant status and disease severity. J Card Fail. 2004;10(4):334-338.
9. Salami M, Galli C, De Angelis L, Visioli F. Formation of F2-isoprostanes in oxidized low density lipoprotein: inhibitory effect of hydroxytyrosol. Pharmacol Res. 1995;31(5):275-279.
10. Pomara N, Bruno D, Sarreal AS, et al. Lower CSF amyloid beta peptides and higher F2-isoprostanes in cognitively intact elderly individuals with major depressive disorder. Am J Psychiatry. 2012;169(5):523-530.
11. Seet RC, Lee CY, Lim EC, et al. Oxidative damage in Parkinson disease: Measurement using accurate biomarkers. Free Radic Biol Med. 2010;48(4):560-566.
12. Segal BM, Thomas W, Zhu X, et al. Oxidative stress and fatigue in systemic lupus erythematosus. Lupus. 2012;21(9):984-992.
13. Il’yasova D, Wang F, Spasojevic I, et al. Urinary F2-isoprostanes, obesity, and weight gain in the IRAS cohort. Obesity (Silver Spring). 2012;20(9):1915-1921.
14. Barocas DA, Motley S, Cookson MS, et al. Oxidative stress measured by urine F2-isoprostane level is associated with prostate cancer. J Urol. 2011;185(6):2102-2107.
15. Qi Dai, Ziangzhu Zhu N. F2-isoprostanes and Metabolite, and Breast Cancer Risk. Am J Med Sci. 2009;2(3):106-108.
16. Fowke JH, Morrow JD, Motley S, et al. Brassica vegetable consumption reduces urinary F2-isoprostane levels independent of micronutrient intake. Carcinogenesis. 2006;27(10):2096-2102.
17. Dietrich M, Block G, Hudes M, et.al., Antioxidant supplementation decreases lipid peroxidation biomarker F(2)-isoprostanes in plasma of smokers. Cancer Epidemiol Biomarkers Prev. 2002;11(1):7-13.
18. Mayne ST, Walter M, Cartmel B, et al. Supplemental beta-carotene, smoking, and urinary F2-isoprostane excretion in patients with prior early stage head and neck cancer. Nutr Cancer. 2004;49(1):1-6.
19. Visioli F, Caruso D, Galli C, et al. Olive oils rich in natural catecholic phenols decrease isoprostane excretion in humans. Biochem Biophys Res Commun. 2000;278(3):797-799.