Robert Kachko, ND, LAc
Rollin McCraty, PhD
Tolle Totum
For naturopathic medicine to continue to prosper as healthcare evolves, it becomes exceedingly important to be precise and personalized in our approach. We’ve long known that helping patients incorporate positive emotions into their daily lives has clinical relevance. Just as diet and lifestyle counseling are crucial to successful outcomes, guiding patients to better understand the impact of their emotions on their physical well-being is paramount.
At The Heart Of It All
It’s well established in the literature that losing a significant person in your life considerably increases your risk for heart attack, but it is poorly understood why this is so. Emerging science points to a deep connection between the heart and brain and the role of the full spectrum of human emotion on health outcomes. While our naturopathic therapeutics must always be the foundation of any comprehensive care plan, gaining a better understanding of how our autonomic nervous system fosters communication between our hearts and minds is a useful tool in supporting those therapeutics. In order to do so effectively, we have an opportunity to embrace technology that will offer objective insights into previously only-subjective human experience and hard-to-quantify health goals. Heart Rate Variability (HRV) is one such technology, as it allows us to assess a unique intersection of physical and emotional well-being within our patients in real time.
A Glance At The Science Of HRV
Fluctuations in the heart rhythm result from complex, nonlinear interactions among a number of different physiological systems. In an effort to maintain homeostasis and self-regulatory capacity at all times, the afferent (via the vagus nerve) and efferent signals between the heart and brain work in harmony to regulate the heart rhythm. While too much variation or instability in these systems leads to nervous system chaos, too little variation may, in some ways, be more detrimental, correlating with a multitude of otherwise unrelated chronic diseases. As a rather crude rule of thumb, the higher the variability in time between heart beats, the less likely a patient is to suffer from some form of chronic disease (all else equal). Thus, HRV is a measure of neurocardiac function that reflects key heart-brain interactions and autonomic nervous system (ANS) dynamics.
HRV Coherence
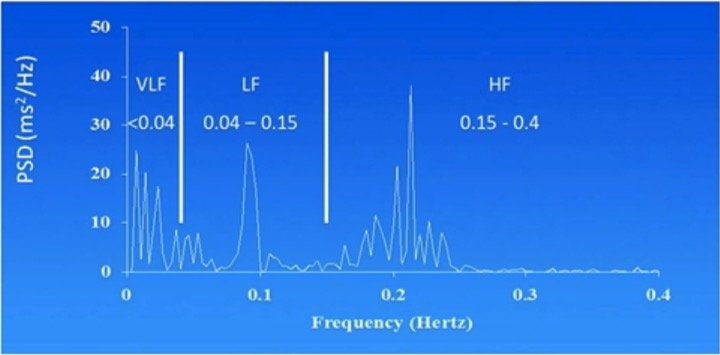
Aside from the absolute beat-to-beat variability in the heart rhythm, smooth transition between beats (coherence) indicates an appropriate complex adaptive response. Physiologically, coherence is used to describe the degree of order, harmony, and stability in the various rhythmic activities within living systems over any given time period.1 HRV coherence is a functional mode associated with positive emotional states2 and enhanced capacity to self-regulate, better performance, and health outcomes.3-9 In the power spectrum (Figure 1), HRV coherence is represented as a large increase in the low-frequency band and a decrease in power in the very-low-frequency and high-frequency bands.10 A coherent heart rhythm is defined as a relatively harmonic (sine wave-like) signal with a very narrow, high-amplitude peak in the low-frequency region (typically around 0.1 Hz) of the power spectrum, with no major peaks in the other bands.
Figure 1. HRV Coherence
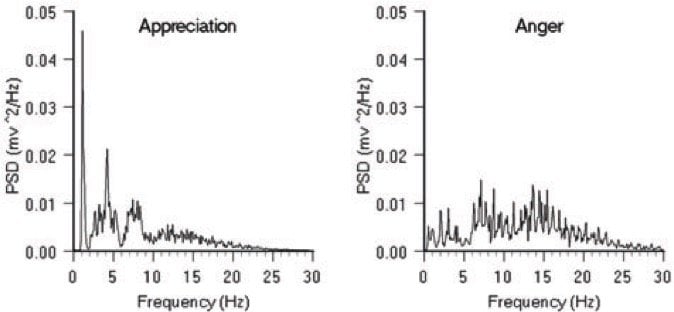
As can be seen in Figures 2 and 3, the HRV rhythm as a function of time is very state-specific, with higher variability and coherence occurring during the activation of positive emotional states such as gratitude, and the opposite patterns occurring during predominantly negative states such as anger or fear. Interestingly, the state-to-state changes that occur are predominantly a function of parasympathetic nervous system activity, via the vagus nerve. (While most physiology textbooks fail to highlight this fact, there are actually more afferent nerve fibers traveling from heart to brain through the vagus nerve than efferent fibers. Of similar intrigue, the heart is able to exert wide-ranging neurohormonal effects via the release of atrial natriuretic peptide,11-13 oxytocin,14 and the catecholamines.15
Figure 2. Heart Rhythm Patterns
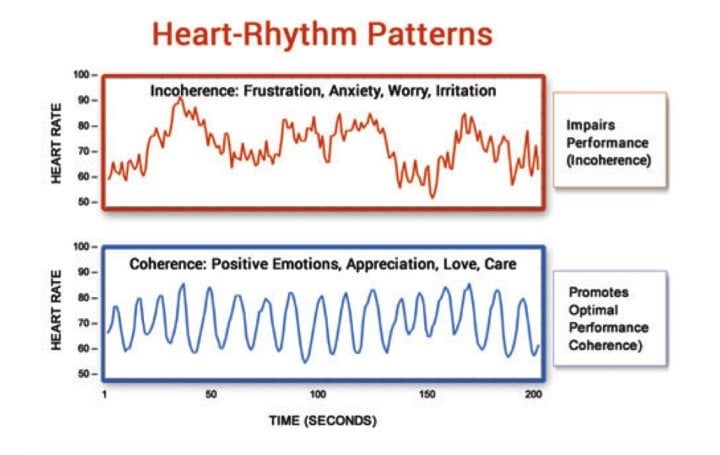
Figure 3. HRV: Appreciation vs Anger
Influencing & Activating HRV Improvements
In daily practice, we often encounter patients who understand that stress is a key determinant of health outcomes, and that techniques such as mindful breathing or meditation can serve a central role in mitigating the effects of stress. Almost as often, though, we may hear that our patients are not able to sustain meditation for long periods of time for a multitude of reasons: their mind wanders, they don’t feel like they’re doing it “right,” or they simply cannot find the time.
Biofeedback technology allows us to offer insights to our patients that can often help them overcome these hurdles. There are many approaches to biofeedback, which provides an opportunity for patients to discover how their bodies are functioning in real time, with the intention of correcting detrimental physiologic states through a better understanding of the totality of those states. While expanding upon all of the medical uses of biofeedback is beyond the scope of this article, HRV biofeedback is one useful approach to incorporate into practice, as it provides a real-time objective understanding of the nexus between emotional states and ANS activity. Just as importantly, patients learn that they are in fact very much in control of their adaptive response to any given situation and that they have the ability to influence the state of their nervous system function.
Research shows that the most useful techniques to improve HRV and coherence include paced, heart-centered breathing (at 6 breaths per minute) coupled with the activation of positive emotion, such as gratitude. Importantly, in order to impact long-lasting change and sustainably improve HRV, patients must actually activate the positive emotional state and “feel” its effects throughout the body. If the effort is purely mental, little progress is made.16,17
HRV As An Indicator Of Health Outcomes
Measuring, tracking, and working to improve HRV outcomes seem to indicate a higher likelihood of recovery from debilitating illness. Much of the research has focused on cardiovascular outcomes, especially related to recovery from myocardial infarction (MI). In one study, the relative risk of mortality after MI was 5.3 times higher in the group with HR variability of less than 50 ms, as compared to the group with HR variability of more than 100 ms.18 Similarly, a 1-SD increase in HRV – determined from a 20-minute ECG resting-state recording – was associated with a 52-59% reduction in the 10-year risk of developing coronary heart disease, as well as an inverse correlation with Framingham Risk Score.19
Low HRV also correlates with higher likelihood of major depressive disorder,20 anxiety,21 inflammatory diseases such as Crohn’s disease,22,23 adrenal insufficiency,24 and type 2 diabetes.25 Teaching patients to use HRV-based biofeedback devices that help them to change their breathing and activate positive emotion has been shown to be an effective strategy in a wide variety of populations. These types of interventions have been demonstrated to help improve metabolic disorders (sustained changes in lipid markers, blood pressure, and glucose have been achieved among highly stressed correctional officers26), increase self-regulation and memory in those with post-traumatic stress disorder,27 improve functional capacity in congestive heart failure,28 and reduce blood pressure, at times better than standard-of-care medication.29 While not a panacea, helping patients to understand the impact of their emotional state on their physical well-being is an important tool in the naturopathic toolkit.
HRV & Whole-Person Naturopathic Care
As a profession, one of our greatest strengths is the personalized, eclectic nature of our practices. Beyond a necessary baseline standard of care, it is often said that 10 naturopathic doctors might use 10 different approaches to a particular case; much of the time the patient in question will get better. Our capacity to impact meaningful change lies most often not in the tools we use, but rather in the reasons we use them. Measuring HRV provides an interesting insight into the whole-body impact of our therapies. Likewise, it offers an opportunity to objectively track patient outcomes and provide positive reinforcement that improves compliance.
Many of the therapies we use to prevent or treat chronic disease lead to simultaneous improvements in HRV markers. For example, there is a strong positive correlation to HRV among individuals who never smoke cigarettes, consume a healthy diet, perform moderate (150 min/wk) or vigorous (75 min/wk) physical activity, have a body mass index (BMI) <25 kg/m2, have a total cholesterol <200 mg/dL, have a glycated hemoglobin A1c <5.7%, and maintain blood pressure <120 mm Hg (systolic) and <80 mm Hg (diastolic).30 For every 1-unit increase in the Mediterranean diet score, there is a 3.5% improvement in HRV measures; similarly, green, leafy vegetable intake, as well as a higher intake of omega-3 fatty acids, correlates with higher HRV, in particular.31,32 In a study of 549 elderly men, T allele carriers of the 677CT MTHFR gene (CT/TT genotypes) had HRV measures that were 17.1% lower than in subjects with the MTHFR CC genotype; however, these effects are abrogated in subjects with higher intakes (above median levels) of vitamin B6, B12, or methionine.33 In a large review of 18 667 individuals, HRV measures were decreased after an elevation in exposure to particulate air pollution (PM <2.5).32 Similarly, HRV is highest during the non-smoking hours of a 24-hour cycle in regular smokers.33 Cognitive behavioral therapy,34 laugh therapy,35 yoga,36 meditation,37 hypnotherapy,38 green “nature bathing” walks at lunchtime,39 and acupuncture40 have all been shown to improve HRV parameters as well.
Parting Thoughts
Throughout the history of naturopathic medicine, we’ve effectively demonstrated the very definition of the frontier, perpetually years ahead of others in “novel” discoveries that have always been at the heart of what we do. Ever at the cutting edge while staying grounded in the roots of our medicine, we’re coming upon some truly important decisions as individual providers and as a profession.
The primary care clinic of the future will offer every kind of “-omics” imaginable (if you’re not quite sure about what that means, a deep Google dive may be in order), coupled with deep learning and predictive diagnostics powered by artificial intelligence that will redefine the doctor-patient relationship. While technology will no doubt save lives, it will also contribute to the further dehumanization of the standard medical experience. How do we define ourselves as medicine evolves to be more high-tech and low-touch? How do we stay unique and necessary among the rising tide of integrative medicine? As a profession, we have a golden opportunity to be a voice of reason while also embracing these coming advances in “precision” medicine. Incorporating an approach like HRV technology, within the context of whole-person naturopathic care, may just be a reasonable way to dip our toes into the fast-moving current of advancements in medicine.
Refs:
- McCraty R, Atkinson M, Tomasino D, Bradley RT. The Coherent Heart: Heart‐Brain Interactions, Psychophysiological Coherence, and the Emergence of System‐Wide Order. Integral Review. 2009;5(2):10‐ Available at: http://integral-review.org/documents/McCraty%20et%20al,,%20Coherent%20Heart,%20Vol.%205%20No.%202.pdf. Accessed July 15, 2017.
- McCraty R, Atkinson M, Tiller WA, et al. The effects of emotions on short‐term power spectrum analysis of heart rate variability. Am J Cardiol. 1995;76(14):1089‐
- McCraty R, Barrios‐Choplin B, Rozman D, et al. The impact of a new emotional self‐management program on stress, emotions, heart rate variability, DHEA and cortisol. Integr Physiol Behav Sci. 1998;33(2):151‐
- Luskin F, Reitz M, Newell K, et al. A controlled pilot study of stress management training of elderly patients with congestive heart failure. Prev Cardiol. 2002;5(4):168-172.
- McCraty R, Atkinson M, Tomasino D. Impact of a workplace stress reduction program on blood pressure and emotional health in hypertensive employees. J Altern Complement Med. 2003;9(3):355‐
- Lehrer P, Vaschillo E, Lu SE, et al. Heart rate variability biofeedback: effects of age on heart rate variability, baroreflex gain, and asthma. Chest. 2006;129(2):278‐
- Hassett AL, Radvanski DC, Vaschillo EG, et al. A pilot study of the efficacy of heart rate variability (HRV) biofeedback in patients with fibromyalgia. Appl Psychophysiol Biofeedback. 2007;32(1):1‐
- McCraty R, Atkinson M. Resilence Training Program Reduces Physiological and Psychological Stress in Police Officers. Glob Adv Health Med. 2012;1(5):44‐
- Berry ME, Chapple IT, Ginsberg JP, et al. Non-pharmacological Intervention for Chronic Pain in Veterans: A Pilot Study of Heart Rate Variability Biofeedback. Glob Adv Health Med. 2014;3(2):28‐
- Ströhle A, Kellner M, Holsboer F, Wiedemann K. Atrial natriuretic hormone decreases endocrine response to a combined dexamethasone-corticotropin-releasing hormone test. Biol Psychiatry. 1998;43(5):371-375.
- Butler GC, Senn BL, Floras JS. Influence of atrial natriuretic factor on heart rate variability in normal men. Am J Physiol. 1994;267(2 Pt 2):H500-H505.
- Vollmar AM, Lang RE, Hänze J, Schulz R. A possible linkage of atrial natriuretic peptide to the immune system. Am J Hypertens. 1990;3(5 Pt 1):408-411.
- Gutkowska J, Jankowski M, Mukaddam-Daher S, McCann SM. Oxytocin is a cardiovascular hormone. Braz J Med Biol Res. 2000;33(6):625-633.
- Huang MH, Friend DS, Sunday ME, et al. Identification of novel catecholamine-containing cells not associated with sympathetic neurons in cardiac muscle. Circulation. 1995;92(8 Suppl):I-59.
- Rein G, Atkinson M, McCraty R. The Physiological and Psychological Effects of Compassion and Anger. Journal of Advancement in Medicine. 1995;8(2):87-105. Available at: http://www.heartmathbenelux.com/doc/compassion-and-anger.pdf. Accessed July 15, 2017.
- Kleiger RE, Miller JP, Bigger JT Jr, Moss AJ. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol.1987;59(4):256-262.
- Yoo CS, Lee K, Yi SH, et al. Association of Heart Rate Variability with the Framingham Risk Score in Healthy Adults. Korean J Fam Med. 2011;32(6):334-340.
- Kemp AH, Quintana DS, Gray MA, et al. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry. 2010;67(11):1067-1074.
- Kemp AH, Quintana DS, Felmingham KL, et al. Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: implications for cardiovascular risk. PLoS One. 2012;7(2):e30777.
- Aeschbacher S, Schoen T, Dörig L, et al. Heart rate, heart rate variability and inflammatory biomarkers among young and healthy adults. Ann Med. 2017;49(1):32-41.
- Engel T, Ben-Horin S, Beer-Gabel M. Autonomic Dysfunction Correlates with Clinical and Inflammatory Activity in Patients with Crohn’s Disease. Inflamm Bowel Dis.2015;21(10):2320-2326.
- Morris JA Jr, Norris PR, Waitman LR, et al. Adrenal insufficiency, heart rate variability, and complex biologic systems: a study of 1,871 critically ill trauma patients. J Am Coll Surg.2007;204(5):885-892.
- Tiftikcioglu BI, Bilgin S, Duksal T, et al. Autonomic Neuropathy and Endothelial Dysfunction in Patients With Impaired Glucose Tolerance or Type 2 Diabetes Mellitus. Medicine (Baltimore). 2016;95(14):e3340.
- McCraty R, Atkinson M, Lipsenthal L, Arguelles L. New hope for correctional officers: an innovative program for reducing stress and health risks. Appl Psychophysiol Biofeedback. 2009;34(4):251‐
- Ginsberg JP, Berry ME, Powell DA. Cardiac coherence and posttraumatic stress disorder in combat veterans. Altern Ther Health Med. 2010;16(4):52‐
- Luskin F, Newell K, Haskell W. A pilot study on the effects of stress management training of elderly patients with congestive heart failure. Prev Cardiol. 1999;2(3):101-104.
- Alabdulgader AA. Coherence: a novel nonpharmacological modality for lowering blood pressure in hypertensive patients. Glob Adv Health Med. 2012;1(2):54‐
- Aeschbacher S, Bossard M, Ruperti Repilado FJ, et al. Healthy lifestyle and heart rate variability in young adults. Eur J Prev Cardiol. 2016;23(10):1037-1044.
- Mozaffarian D, Stein PK, Prineas RJ, Siscovick DS. Dietary fish and omega-3 fatty acid consumption and heart rate variability in US adults. Circulation. 2008;117(9):1130-1137.
- Dai J, Lampert R, Wilson PW, et al. Mediterranean dietary pattern is associated with improved cardiac autonomic function among middle-aged men: a twin study. Circ Cardiovasc Qual Outcomes. 2010;3(4):366-373.
- Baccarelli A, Cassano PA, Litonjua A, et al. Cardiac autonomic dysfunction: effects from particulate air pollution and protection by dietary methyl nutrients and metabolic polymorphisms. Circulation. 2008;117(14):1802-1809.
- Pieters N, Plusquin M, Cox B, et al. An epidemiological appraisal of the association between heart rate variability and particulate air pollution: a meta-analysis. Heart. 2012;98(15):1127-1135.
- Minami J, Ishimitsu T, Matsuoka H. Effects of smoking cessation on blood pressure and heart rate variability in habitual smokers. Hypertension. 1999;33(1 Pt 2):586-590.
- Carney RR, Freedland KE, Stein PK, et al. Change in heart rate and heart rate variability during treatment for depression in patients with coronary heart disease. Psychosom Med. 2000;62(5):639-647.
- Dolgoff-Kaspar R, Baldwin A, Johnson MS, et al. Effect of laughter yoga on mood and heart rate variability in patients awaiting organ transplantation: a pilot study. Altern Ther Health Med. 2012;18(5):61-66.
- Tyagi A, Cohen M. Yoga and heart rate variability: A comprehensive review of the literature. Int J Yoga. 2016;9(2):97-113.
- Nijjar PS, Puppala VK, Dickinson O, et al. Modulation of the autonomic nervous system assessed through heart rate variability by a mindfulness based stress reduction program. Int J Cardiol. 2014;177(2):557-559.
- Yüksel R, Ozcan O, Dane S. The effects of hypnosis on heart rate variability. Int J Clin Exp Hypn. 2013;61(2):162-171.
- Gladwell VF, Kuoppa P, Tarvainen MP, Rogerson M. A Lunchtime Walk in Nature Enhances Restoration of Autonomic Control during Night-Time Sleep: Results from a Preliminary Study. Int J Environ Res Public Health. 2016;13(3):280.
- Huang ST, Chen GY, Lo HM. et al. Increase in the vagal modulation by acupuncture at neiguan point in the healthy subjects. Am J Chin Med. 2005;33(1):157-164.
Image Copyright: <a href=’https://www.123rf.com/profile_dolgachov’>dolgachov / 123RF Stock Photo</a>
 Robert Kachko, ND, LAc, graduated from the U of Bridgeport College of Naturopathic Medicine and Acupuncture Institute with degrees in both naturopathic medicine and acupuncture. Dr Kachko is co-founder and CEO of TribeRx, a medical technology company helping physicians to address social isolation among their patients. He also maintains a private practice at InnerSource Health in NYC. Dr Kachko serves on the Board of Directors of the AANP and the NYANP, and as Chair of Public Education and Media Affairs for the AANP. He also serves on the Advisory Board for Sharp Again Naturally (a non-profit committed to natural approaches to dementia), and serves as a clinical research consultant to the Alzheimer’s Prevention Clinic at Weill Cornell Medical.
Robert Kachko, ND, LAc, graduated from the U of Bridgeport College of Naturopathic Medicine and Acupuncture Institute with degrees in both naturopathic medicine and acupuncture. Dr Kachko is co-founder and CEO of TribeRx, a medical technology company helping physicians to address social isolation among their patients. He also maintains a private practice at InnerSource Health in NYC. Dr Kachko serves on the Board of Directors of the AANP and the NYANP, and as Chair of Public Education and Media Affairs for the AANP. He also serves on the Advisory Board for Sharp Again Naturally (a non-profit committed to natural approaches to dementia), and serves as a clinical research consultant to the Alzheimer’s Prevention Clinic at Weill Cornell Medical.
 Rollin McCraty, PhD, is Director of Research of the HeartMath Research Center at the Institute of HeartMath. He is also a professor at Florida Atlantic University. A psychophysiologist, Dr McCraty’s research on the mechanisms by which emotions influence cognitive processes, behavior, and health have been applied to the development of simple, user-friendly mental and emotional self-regulation tools and techniques. Dr McCraty has acted as Principal Investigator in numerous and varied laboratory research studies and field studies examining the effects of emotions on heart–brain interactions and on autonomic, cardiovascular, hormonal, and immune system function.
Rollin McCraty, PhD, is Director of Research of the HeartMath Research Center at the Institute of HeartMath. He is also a professor at Florida Atlantic University. A psychophysiologist, Dr McCraty’s research on the mechanisms by which emotions influence cognitive processes, behavior, and health have been applied to the development of simple, user-friendly mental and emotional self-regulation tools and techniques. Dr McCraty has acted as Principal Investigator in numerous and varied laboratory research studies and field studies examining the effects of emotions on heart–brain interactions and on autonomic, cardiovascular, hormonal, and immune system function.

