Martin Milner, ND
The management of atrial fibrillation requires a multi-factorial approach. To begin, the patient’s blood must be optimally thinned to avoid significant comorbidities, such as pulmonary embolism, stroke and myocardial infarct. In addition, the patient’s ventricular response rate must be slowed to 80-100bpm, and the rhythm converted to a normal sinus rhythm to avoid atrial cardiomyopathy and congestive heart failure.
NDs are well armed to accomplish both of these goals in atrial fibrillation patients.
Clot Prevention
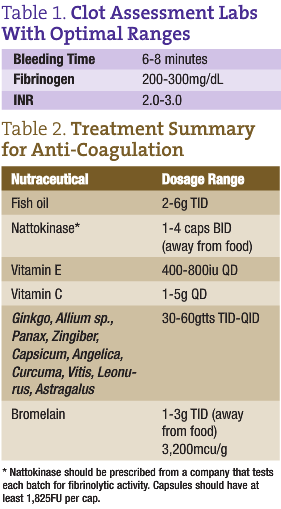
When a patient is in atrial fibrillation for greater than 48 hours, his or her risk of stroke greatly increases, and it becomes necessary to thin their blood. Many patients with atrial fibrillation will consult with NDs to avoid, decrease or discontinue warfarin. This can be accomplished over time, but must be carefully managed. The patient’s warfarin dose should be automatically reduced after weekly international normalized ratios (INRs) as naturopathic protocols gradually take over the role of thinning the blood and preventing clot formation. Patients should be followed as they are transitioned off of warfarin to optimize bleeding time (measured by placing a blood pressure cuff at 40mm/Hg with a standardized Surgicutt lancet to the forearm followed by timing the duration of clot formation) and fibrinogen levels (ideal target 250-300; see Table 1). Patients must be diligent and compliant with naturopathic treatments during this process to ensure proper blood viscosity.
Fish Oil
Fish oil consistently has been shown to increase fibrinolytic activity and decrease blood viscosity, and is often the first agent we will employ to reduce clot risk (al-Awadhi and Dunn, 2000). It is important to ensure that the prescribed fish oil has been tested for rancidity, levels of DHA and EPA, and heavy metals as the environmental burden increases. We begin dosing at 2g TID with meals for 100-lb individuals and increase by 3g daily for every 100lbs. This starting dose is reassessed with monthly bleeding times and fibrinogen levels (see Table 1). If the target is not reached, the dose is increased to a maximum of 6g TID. This dose is maintained on an ongoing basis. If dose elevations have not significantly altered target ranges, the dose will be lowered to 2g TID with meals, and nattokinase or other blood thinning agents will be added to the protocol.
Nattokinase
Nattokinase is a fibrinolytic enzyme derived from natto, a constituent of fermented vegetable products common in Japan. Many in vitro and in vivo studies have consistently demonstrated the potent pro-fibrinolytic effect of the enzyme, and researchers are now demonstrating that nattokinase has significant power to decrease both RBC aggregation and blood viscosity (Pais et al., 2006; Sumi et al., 1987). When prescribing nattokinase, be aware that there is a broad range of quality in the fibrinolytic activity, measured in fibrinolytic units (FU), and some products may contain vitamin K, which should be avoided. A soft gel in an oil base is well absorbed and more effective in reaching target lab levels than the dry capsule.
The starting protocol begins with 1 soft gel (with 2000FU) twice daily on an empty stomach an hour away from meals for a 100lb individual. We will increase this dose based on body weight 2-4 BID until targeted blood levels of bleeding time and fibrinogen levels are achieved after 30 days of medication. Remember, these patients are already taking 6-12g or more EFAs, and we are adding nattokinase to further inhibit their chronic coagulation mechanisms.
Other Nutraceuticals
 Many other nutraceuticals can affect platelet aggregation as well as blood viscosity, and can be used therapeutically in atrial fibrillation in combination with or independently of nattokinase. Note that fish oil or other stable forms of omega-3s should always be used in the treatment of atrial fibrillation. All supplements must be taken regularly, daily and consistently. With consistency, one can easily monitor the effect of these other nutrients on warfarin clotting times and INR as well as platelet aggregation bleeding times and fibrin stranding with fibrinogen levels. Many conventional warfarin labs provide a list of nutraceuticals considered to be direct contraindications simply because they may interact with warfarin and may require lowering of the necessary dose of warfarin. Ginkgo biloba, Allium sativa, Allium cepa, Panax ginseng, Capsicum species, Angelica sinensis, Curcuma longa, Vitis vinifera, Leonurus cardiaca, Astragalus membranosus and Zingiber officinalis can be used to help prevent clot formation.
Many other nutraceuticals can affect platelet aggregation as well as blood viscosity, and can be used therapeutically in atrial fibrillation in combination with or independently of nattokinase. Note that fish oil or other stable forms of omega-3s should always be used in the treatment of atrial fibrillation. All supplements must be taken regularly, daily and consistently. With consistency, one can easily monitor the effect of these other nutrients on warfarin clotting times and INR as well as platelet aggregation bleeding times and fibrin stranding with fibrinogen levels. Many conventional warfarin labs provide a list of nutraceuticals considered to be direct contraindications simply because they may interact with warfarin and may require lowering of the necessary dose of warfarin. Ginkgo biloba, Allium sativa, Allium cepa, Panax ginseng, Capsicum species, Angelica sinensis, Curcuma longa, Vitis vinifera, Leonurus cardiaca, Astragalus membranosus and Zingiber officinalis can be used to help prevent clot formation.
Bromelain may be dosed in lieu of nattokinase at fairly high doses. Start at 1g TID up to 3g TID away from food. A bromelain product should be selected with at least 3,200mcu/g (milk clotting units, a measure of bromelain activity).
Vitamin E acts as a platelet aggregation inhibitor and can be dosed at 400-800iu QD. Vitamin C can also be administered at doses of 1-5g QD, but should not be discontinued abruptly to avoid inducing scurvy symptoms. See Table 2 for a summary of treatments that prevent clot formation.
Slowing Ventricular Response and Converting to Normal Sinus Rhythm
Omega-3 fatty acids have a marked effect on coagulation. It is now coming to light that they also strongly affect conduction in the heart. According to a recent article, lab-based research studies and large clinical trials have found that omega-3 fatty acids have an anti-arrhythmic efficacy. It has been found that omega-3 alters ionic channels in the heart that regulate transmembrane action potentials, reduce incidence of sudden death in survivors of MI, and benefit atrial fibrillation, ventricular ectopy and ventricular tachyarrhythmias (Lombardi and Terranova, 2007; Reiffel and McDonald, 2006). A large population-based study evaluated fish intake and electrocardiographic parameters, and found that subjects who consumed fish had slower AV conduction and a lower heart rate, and were less likely to have arrhythmias (Mozaffarian et al., 2006). Clearly, omega-3 fatty acids must be used in the treatment of atrial fibrillation.
Magnesium may also be of benefit to slow conduction, convert to normal sinus and prevent atrial fibrillation from occurring. Iseri (1990) states that magnesium treatment is a viable therapeutic option when other antiarrhythmic agents fail to suppress ventricular tachycardia, ventricular fibrillation, multifocal atrial tachycardia, atrial fibrillation and supraventricular tachycardia. Begin dosing at 500-1000mg of oral chelated magnesium for the prevention and treatment of atrial fibrillation in patients who are not currently in active atrial fib. In patients who are in active atrial fibrillation, we administer 1g intravenously with calcium.
Many botanicals have antiarrhythmic qualities. Digitalis purpurea, either in tincture form or in homeopathic dilutions of 3x-12x, can be helpful to convert patients out of atrial fibrillation and/or slow the ventricular response. For dosing, 15 drops can be used as a loading dose followed by 5 drops QD. Digitalis 3x can be administered every 15 minutes during acute atrial fib and is a safer alternative to the tincture. If using the whole plant, it is necessary to monitor blood Digitalis levels and maintain patients in a steady state. Labs should be drawn six hours after their last dose.
Other antiarrhythmic herbs include:
- Selenicereus grandiflora
- Strophanthus hispidus
- Convallaria majalis (similar to Digitalis but less toxic)
- Leonurus cardiaca
- Crataegus species
- Cytisus scoparius
- Gelsemium sempervirens in drop dosages
- Rauwolfia serpentina
- Lycopus virginica
- Ginkgo biloba.
Whether your practice focuses on botanical medicine, homeopathy or neutraceuticals, many options exist to help prevent atrial fibrillation from creating severe morbidity in patients. The goals for treating atrial fibrillation are to prevent clots, slow the ventricular response during the arrhythmia, convert to normal sinus and fundamentally prevent atrial fibrillation from returning. Nevertheless, the ultimate goal, as NDs, is to always address and treat the underlying cause for each patient.
 Martin Milner, ND received his naturopathic degree in 1983 from NCNM in 1983, and serves at NCNM as professor of cardiovascular and pulmonary medicine. Dr. Milner is also the CEO and medical director of the Center for Holistic Medicine (1983-1991) and Center for Natural Medicine (CNM) (1991-present). Dr. Milner has treated more than 20,000 patients with heart disease alone over the course of his 23 years of practice as a physician. Dr. Milner is well published with texts, medical journal articles and studies in endocrinology, cardiology, pulmonology, oncology and environmental medicine. He is currently lecturing around the U.S., guiding physicians and compounding pharmacists in the management of hypothyroidism using his protocol of slow released compounded thyroid replacement.
Martin Milner, ND received his naturopathic degree in 1983 from NCNM in 1983, and serves at NCNM as professor of cardiovascular and pulmonary medicine. Dr. Milner is also the CEO and medical director of the Center for Holistic Medicine (1983-1991) and Center for Natural Medicine (CNM) (1991-present). Dr. Milner has treated more than 20,000 patients with heart disease alone over the course of his 23 years of practice as a physician. Dr. Milner is well published with texts, medical journal articles and studies in endocrinology, cardiology, pulmonology, oncology and environmental medicine. He is currently lecturing around the U.S., guiding physicians and compounding pharmacists in the management of hypothyroidism using his protocol of slow released compounded thyroid replacement.
References
al-Awadhi AM, Dunn CD. Effects of fish-oil constituents and plasma lipids on fibrinolysis in vitro, Br J Biomed Sci 57(4):273-80, 2000.
Pais E et al: Effects of nattokinase, a pro-fibrinolytic enzyme, on red blood cell aggregation and whole blood viscosity, Clin Hemorheol Microcirc 35(1-2):139-42, 2006.
Sumi H et al: A novel fibrinolytic enzyme (nattokinase) in the vegetable cheese Natto; a typical and popular soybean food in the Japanese diet, Experientia Oct 15;43(10):1110-1, 1987.
Lombardi F, Terranova P: Anti-arrhythmic properties of N-3 poly-unsaturated fatty acids (n-3 PUFA), Curr Med Chem 14(19):2070-80, 2007.
Reiffel JA, McDonald A: Antiarrhythmic effects of omega-3 fatty acids, Am J Cardiol Aug 21;98(4A):50i-60i, 2006.
Mozaffarian D et al: Dietary fish and n-3 fatty acid intake and cardiac electrocardiographic parameters in humans, J Am Coll Cardiol Aug 1;48(3):478-84, 2006.
Iseri LT: Role of magnesium in cardiac tachyarrhythmias, Am J Cardiol Jun 19;65(23):47K-50K, 1990.


