David M. Brady, ND, DC, CCN, DACBN
This article is one in a series of Clinical Rounds, which has been appearing periodically in NDNR. Real case studies from Dr. Brady’s practice are presented. It is his aim to present interesting cases that will facilitate thought and discussion about novel diagnostic and therapeutic techniques for myriad clinical conditions likely to appear in other ND offices.
Patient Presentation and History
A 42-year-old female presented with the primary complaint of fatigue. Her symptom/complaint list was:
- Fatigue
- Exercise intolerance
- Post-prandial bloating
- Right shoulder pain
- Chronic bladder infections
- Peri-menopausal symptoms (i.e., irregular menses, heavy flow, cramping, hot flashes)
- Hypothyroid symptoms previously (i.e., fatigue, dry skin, hair falling out)
- Elevated mercury burden.
The onset of symptoms was approximately 12 years prior to presentation. Upon completing a medical history and questioning the patient, I learned that the onset of her fatigue correlated with a period of significant stress and just after her second pregnancy. She had episodes in the past of her hair thinning and falling out, as well as skin dryness. She has suffered for many years from bloating after meals, as well as from chronic cystitis. Urological workups did not reveal any strictures or anatomical problems via cystography. The patient has frequently resorted to antibiotics usage to manage this problem, though she also often uses cranberry and olive leaf as natural anti-microbial agents and for bladder infections. In the past, the patient also was frequently on antibiotics to manage a long-standing acne problem. The patient has been suffering for about six months from some right shoulder discomfort and saw an orthopedic surgeon, who confirmed that there was no significant injury or instability and referred her to a physical therapist. She discontinued physical therapy, as it exacerbated her condition. The patient has very good dietary habits, avoiding excessive carbohydrates and dairy. She is very nutrition-knowledgeable and eats plenty of fresh vegetables, fruits and lean proteins. She suffers from serious sweet and chocolate cravings, although she does not give in to them often. She has a serious allergy to walnuts, pecans and butternuts. The patient does not regularly consume coffee, tea or alcohol, nor does she smoke.
Prior Management
The patient was seen previously by several alternative health practitioners, including a prominent integrated medical physician who performed an extensive diagnostic work-up, including the following:
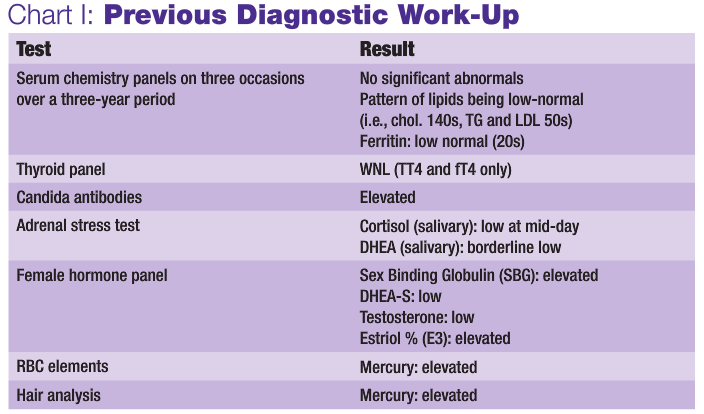
This previous physician prescribed Armour thyroid (90mg bid), based solely on subjective symptoms and low axillary temperatures, even though the limited thyroid testing performed (TT4 and fT4) was within normal limits. It would have been preferable to also have fT3 and TSH levels, at minimum. The patient also received physiological doses of Cortef (hydrocortisone) at 5mg bid (later increased to 5mg tid), DHEA at 10mg qd, pregnenalone at 30mg qd, and an unknown formulary adrenal support supplement based on her adrenal stress test results and symptoms. The patient discontinued the DHEA and pregnenalone after a three-month period and continued the Cortef for one year. She discontinued it eventually, being uncomfortable with taking cortisone long term. She was also given testosterone at 2mg qd, based on the results of her female hormone panel and menstrual symptoms. She took this for a three-month period and discontinued it, not noticing any improvement and being uncomfortable with using testosterone medication.
The patient was given a short course of Diflucan at 200mg qd, probiotics, olive leaf extract and D-mannose for the yeast infection and cystitis. Follow-up testing showed a reduction in yeast antibodies, and the patient’s symptoms improved markedly. She continued to use olive leaf as a preventive measure.
No therapy was directed at the elevated mercury burden. The patient had no silver fillings or known exposures. However, she is a graphics artist and had been exposed to solvents and unknown chemicals during training in college. Repeat hair analysis six months after the first did not show an elevated mercury level. The only intervention the patient can think of was taking olive leaf extract.
Physical Examination
The patient was of normal body composition and looked adequately nourished and hydrated. Thyroid palpation did not reveal any fullness, masses, nodules or tracheal deviation. Standard EENT examination was normal. Heart evaluation revealed a normal rate and rhythm. An apical murmur was present, which previously had never been detected. Lung examination revealed normal and clear breath sounds. Her seated brachial blood pressure was 116/78mm Hg. Remaining vital signs were as follows: pulse 80bpm, respiration 12rpm and oral temperature 96.8 degrees. Abdominal examination was essentially normal, with a previous appendectomy scar in the RLQ. Musculoskeletal and neurological examination revealed multiple myofascial trigger points (TrPs) in the right lower cervical and right shoulder musculature. Normal cervical ROM was noted, with multiple areas of segmental dysfunction in the lower right neck. Right rotator cuff and shoulder girdle muscles were all +5/5, with the exception of the teres minor and latissimus dorsi, which were weak to sustained resistive testing. Standard orthopedic testing of the right shoulder did not produce significant pain or instability. George’s battery of tests was negative and no bruits or thrills were present over the cervical vessels.
Initial Impressions
The presence of this many overlapping symptoms should always cause the practitioner to consider a multi-faceted problem. It seems clear that the patient has a hypothyroid condition, based on her symptoms, temperature and response to thyroid HRT. However, with the peri-menopausal symptoms, sweet cravings, low cortisol and fatigue, there seem to be a much bigger picture involving the endocrine system. The initial treating clinician correctly directed therapy toward the thyroid and adrenals via Armour thyroid and hydrocortisone medications, DHEA and adrenal support supplement. However, the patient still did not feel entirely well and did not like the idea of staying on the medications – particularly the cortisone – long term if not absolutely necessary. It was determined that a more detailed evaluation of the patient’s cellular energy production and mitochondrial function was in order, utilizing an organic acid panel due to long-standing fatigue.
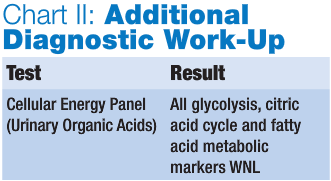
Discussion of Diagnostic Test Results
Organic acid analysis (Cellular Energy Panel by GSDL or Organix by Metametrix Labs) is an excellent way to objectively evaluate mitochondrial function and cellular energy production in an individual. It can aid in identification of a functional metabolic block or lesion, which can result in a lack of ATP production and fatigue, global tissue tenderness, cognitive dysfunction and more. When a block is present, it is usually apparent in that a substance (such as a Kreb’s cycle intermediate) that immediately precedes a metabolic reaction is elevated, while the substance that is immediately downstream to the reaction is low. In such cases, this reflects an inability to bio-transform one substance into the other. This may be the result of a genetic enzyme deficiency, production of a warped enzyme due to oxidative stress to the mitochondrial DNA or, most commonly, a functional deficiency in the nutrient required to catalyze the reaction in question. For example, if pyruvic acid and lactic acid were elevated, while citric acid and other initial Kreb’s cycle intermediates were low, this would suggest a slowing of mitochondrial aerobic metabolism and a backing up into the cytosolic anaerobic metabolism of glycolysis. This situation would obviously yield much less ATP and produce tissue-irritating acidic metabolic waste products, resulting in symptoms such as fatigue, malaise, myalgia, muscle weakness, headache, etc. This patient did not show any specific abnormal pattern that suggested a need for therapeutic repletion of any particular nutrient catalyst, nor the need for any specific amino acid therapy to provide re-filling of the Kreb’s cycle at any intermediate point.
Initial Therapeutic Plan
It was determined that we would direct the therapeutic effort into restoring proper global endocrine balance by stabilizing the patient’s blood sugar, supporting the hypothalamic-pituitary-adrenal (HPA) axis and optimizing peripheral thyroid conversion. Shoulder ROM exercises, myofascial therapy and correction of the cervical segmental dysfunction by spinal manipulation was planned to balance shoulder function. The patient was also referred for a cardiology evaluation to accurately evaluate the apical murmur, since valvular pathologies can certainly result in fatigue, particularly on exertion.
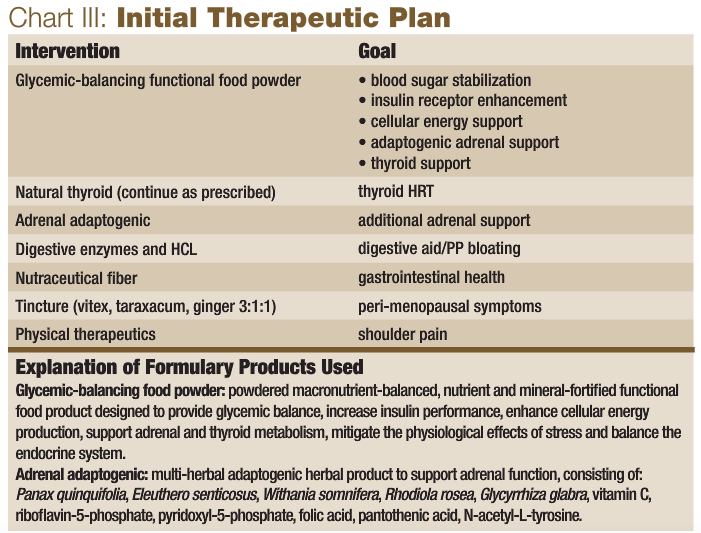
Physical Medicine Protocol
The patient was treated with Active Release Technique (ART), post-isometric stretching and mild ischemic compression to the located TrPs in the cervical and right shoulder girdle musculature. Cervical and thoracic manipulation and mobilization techniques were used in addition to the myofascial techniques.
Six-Week Follow-Up
The patient reported that she felt a significant improvement in her energy levels. She did not like taking the Armour thyroid HRT. However, after some discussion, she came to terms with the probability that a purely nutritional, glandular and/or herbal approach to up-regulate thyroid function to adequate levels had failed on multiple attempts and is unlikely to yield satisfactory results in the future. The patient reported still having painful menstrual periods, with heavy flow and cramping. She had not used the herbal product prescribed for her menstrual difficulties, due to an aversion to the taste of tinctures. She agreed to try an encapsulated alternative. The shoulder problem had not caused any discomfort since the previous visit, and repeat examination did not reveal any pain or muscle weakness. She saw a cardiologist, who performed an echocardiogram and stress test. The cardiologist reported her heart to be strong and confirmed the mitral valve prolapse. The physician did not think the murmur was severe enough to be causing the patient’s fatigue and suggested exercise and stress management.
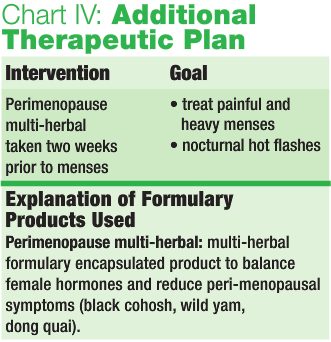
12-Week Follow-Up
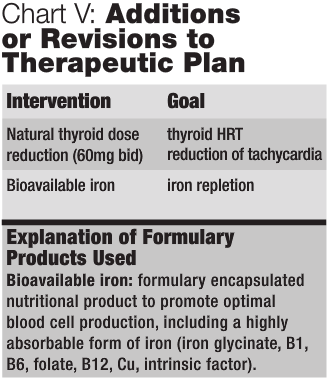
The patient reported that she was feeling very well: “I am feeling better than I have in years.” She reported fewer food cravings and felt much more consistent energy since starting the Metabol-X shake product. She felt her blood sugar was much more stable and she was not having the urge to eat as much. She had also lost weight and looked thinner. She had experienced bad cramping and back pain during her first period after starting the BioFem-HRT product, so she discontinued it. She also had a minor acne outbreak coinciding with her menses. The patient also reported feeling some intermittent “jitters, shakiness and racing pulse rate.” She was advised to contact her prescribing physician regarding reducing her dosage of Armour thyroid to see if that may be a contributing factor. A new blood chemistry, TT4, fT4, ferritin and CBC was performed by her medical physician, which revealed the same pattern as seen previously, including low-normal lipids, normal thyroid markers and a sub-optimal ferritin of 26. The dosage of Armour thyroid was reduced from 90mg bid to 60mg bid, and the patient was advised to take iron supplements due to her ferritin levels, heavy periods and history of anemia. The patient has not reported the elevated pulse rate or “shakiness” since lowering the Armour thyroid dosage.
 Future Diagnostic and Therapeutic Considerations
Future Diagnostic and Therapeutic Considerations
- Heavy metal burden testing (DMSA-provoked urine study) to re-evaluate mercury burden
- Possible oral chelation program (based on test results)
Meta-Tox (Bio-Logics): DMSA
Toxi-HMF (Biogenesis): (NAC, DL-methionine, bentonite, sodium alginate, pectin, C, bioflav, alpha lipoic acid)
Homeopathic: nosode heavy metal detoxifier formulation
- FemGuard + Balance: (Designs for Health): multi-herbal and nutrient encapsulated formulary product for PMS symptoms and female hormonal balance and cancer prevention. (Cimicifuga racemosa, Vitex agnus castus, Curcuma longa, Rosmarinus officinalis, Polygonum cuspidatum, Vitis vinifera, Camelia senensis, BioResponse DIM, chrysin, calcium-D-glucarate, Mg-malate, Ca-malate, B6, B12 and folic acid)
Discussion
This patient’s case is a prime example of how endocrine imbalance can cause myriad symptoms and problems in an individual, particularly in female patients. As discussed previously, altered production of cortisol due to stress or other factors can imbalance blood sugar and all hormonal products of the cholesterol-synthesis pathways, such as androgens and estrogens. This may result in dysglycemia, fatigue, PMS, menstrual irregularity, difficult menopause and a host of female-related problems. Cortisol perturbations can also result in improper thyroid hormone conversion and low thyroid function. Therefore, a comprehensive functional approach to balancing the endocrine system is essential in the management of this patient and others like her.

Brady is a licensed naturopathic physician, board-certified clinical nutritionist and doctor of chiropractic. He is the chief medical officer of Designs for Health and serves as a technical consultant to Metametrix Clinical Laboratory. He presently is director of the Human Nutrition Institute at the University of Bridgeport, and an associate professor of clinical sciences at the University of Bridgeport, Colleges of Naturopathic Medicine and Chiropractic in Bridgeport, Conn. Brady also maintains a private practice at The Center for the Healing Arts in Orange, Conn., where he specializes in functional and metabolic medicine.


