David Brady, ND, DC, CCN, DACBN
Part two in the “Clinical Rounds” series. These clinical rounds are real case studies from my practice. It is my aim to present interesting cases to facilitate thought and discussion about novel diagnostic and therapeutic techniques for a myriad of clinical conditions that are likely to appear in your offices.
Patient Presentation and History
A 35-year-old female presented to my practice with the primary complaint of significant gastrointestinal distress. Her entire symptom/complaint list was as follows: eructation and flatulence; abdominal bloating; fatigue; generalized muscle pain; allergies; and memory and concentration difficulties.
The onset of her symptoms was approximately one year prior to presentation. I particularly remember the day this patient first came to my office. I was just finishing with another patient, running late, and on a deadline to leave my practice in order to get to a class that I was teaching at the University of Bridgeport. Of course, this is when the difficult cases seem to come in. I remember my office manager telling me that we had a difficult situation in the waiting area.
It seemed there was a new walk-in patient who was belching loudly every few minutes and the other patients waiting were obviously uncomfortable with the situation. I had her moved into a consultation room immediately. The poor woman was belching severely every few minutes. She also informed me with great embarrassment that she was having similar problems on the other end, but just less audibly apparent. Upon completing her medical history, I learned that she had just left the office of a prominent conventional gastroenterologist who practiced two doors down from my office. She had been told by him after barium swallow, barium enema and endoscopy that “nothing was obviously wrong with her.” He offered her antacid medications and told her there was nothing else he could do. She then happened to see our offices and thought she had nothing to lose by trying an alternative approach.
The more I questioned this patient, the more I realized that her gut symptoms were only the most apparent of a long laundry list of symptoms. The gut problems may have indeed been serving as the foundation of a mountain of problems in this chronically ill individual. She was experiencing significant gut bloating after meals and occasional cramping, in addition to the belching and flatulence. She was also suffering from significant fatigue and tenderness throughout her body. Mild dermatitis was present in the temporal regions and on the back of her upper arms. She complained of terrible allergy symptoms and was having a difficult time with her memory. It was actually very difficult to maintain a conversation with her due to her inability to stay focused on the conversation. Upon completion of a subjective symptom survey questionnaire, she was found to have significant issues in multiple organ systems and was manifesting a picture common in patients with high total-toxic burden.
The patient was very distressed that she had not been able to hold a job over the past year due to her condition. She was living with her mother, who was caring for her and supporting her.
Physical Examination
The patient’s vitals were normal with the exception of a slightly low oral temperature of 97.4°F. Upon gross examination, EENT was essentially normal. However, she did exhibit “allergic shiners” and moderate frontal and maxillary sinus tenderness. The thyroid palpated normal and was not enlarged. Heart evaluation revealed a normal rate and rhythm without murmur, and lung examination revealed normal breath sounds. Abdominal examination produced moderate tenderness to deep palpation in the extreme quadrants, particularly the left-lower and right-upper quadrants. Neurological examination revealed normal sensory, reflex and motor function. Cerebellar testing was negative. The patient did report pain to moderate digital pressure to the musculature throughout most regions of the body.
Initial Impressions
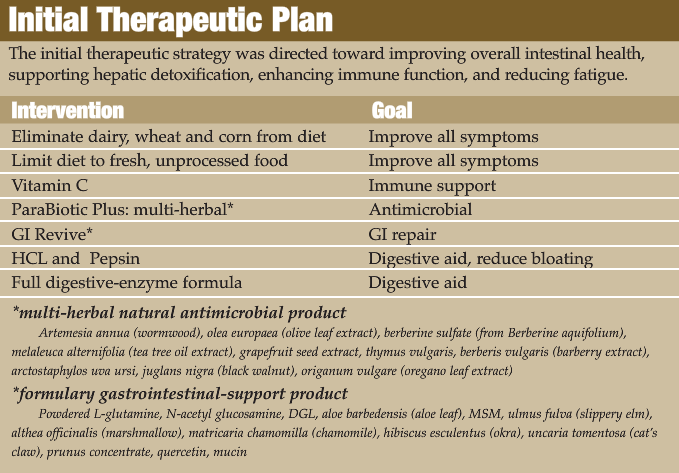
This type of patient presentation with so many symptoms always causes the functional medicine practitioner to consider a significant problem in the gut-liver axis. The prior work-up by the conventional gastroenterologist seems to have ruled out any acute and overt ulcerative or inflammatory bowel disease, making more subtle functional problems the more likely etiology. Chronic mild-to-moderate intestinal inflammation can lead to intestinal hyperpermeability (leaky gut), which can cause a dramatic increase in the antigenic and toxic load into systemic circulation. Mucosal gut disorders and hepatic detoxification insufficiency must then be considered as strong contributing factors to this patient’s declining overall health. Foundational problems such as these can lead to global symptomology such as gut problems, fatigue, metabolic distress, tenderness, cognitive dysfunction, dermatological disorders, allergies, etc. However, any significant internal disorders, which might explain her symptomology, had to be ruled out first (ie, organ failure, cancer, anemia). With this in mind, her initial diagnostic work-up was planned as follows:
 Discussion of Initial Diagnostics
Discussion of Initial Diagnostics
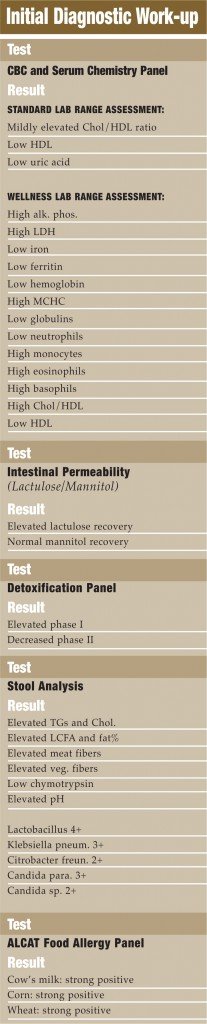
The CBC, basic blood chemistry and thyroid panel were performed on this patient due to her persistent complaints of fatigue. Basic rule-outs such as anemia, infection and serious internal disorders had to be evaluated. When the serum lab studies were evaluated from an overt pathology perspective, they were fairly unremarkable. However, if evaluated from a “wellness” perspective, many potential problems emerged. The patient did appear to be mildly anemic and seemed to show patterns of chronic immune activation (viral challenge, parasitic infection, allergy, etc.). Serum chemistries did not reveal any significant internal pathology but did suggest hepatocellular stress and an increased cardiovascular risk. Thyroid markers were normal. The intestinal permeability study showed that lactulose, a large and normally non-absorbable sugar, is passing through a “leaky” intestinal mucosa. The smaller sugar, mannitol, is not being absorbed at normal levels; suggesting some degree of malabsorption.
While this may seem counter-intuitive to have “leaky gut” and “malabsorption” simultaneously, it is actually seen quite frequently. While the large lactulose is finding its way through the gaps between damaged mucosal cells, the smaller mannitol is not being actively absorbed through the cells as it should be due to inflammatory damage of the gastrointestinal villi. This inflammatory damage results in a loss of mucosal surface area and malabsorption. The net effect is a gut that is “leaky” to large molecules (antigenic proteins and large toxins), while a malabsorption of smaller molecules (micronutrients) also exists. The hepatic detoxification panel showed increased phase I and sluggish phase II activity (“imbalanced or pathological detoxifier”).
This situation is not optimal since phase I detoxification results in toxic intermediates, which are more water-soluble and readily transported, but which must be conjugated via phase II activity in the liver in order to mitigate the oxidative stress produced by these radical compounds.
Stool analysis showed clear signs of maldigestion and malabsorption. Dysbiosis is clearly present with pathogenic microbes present in large amounts (Klebsiella and Citrobacter). An ALCAT food intolerance panel was performed which revealed strong reactions to dairy, wheat and corn. This pan-allergic picture may indeed be due primarily to the intestinal hyperpermeability more than a true, fixed allergy.
Follow-up: Four and Eight Weeks
The patient had a dramatic reduction of her symptoms following the above program for a four-week period. In fact, on her follow-up appointment she was given new-patient paperwork by my front-office staff because they did not recognize. She was no longer presenting with the disheveled, depressed, dull appearance of the chronically ill. She was wearing a red dress, had a different hairstyle, and was bright-eyed, perky and eager to engage in conversation. In other words, her real personality was back. She had landed a new sales job and had firm plans to move out from her mother’s house. This was one of the most dramatic changes I had ever seen in a patient. She was instructed to continue her dietary changes, engage in stress reducing recreational activities, and to continue her multivitamin-mineral and vitamin C.
Follow-up: Eight Months
I continued to see this patient on a monthly basis for manipulation and physical medicine. She progressed very well over this time period. About eight months after her initial visit, she started complaining of some of her original symptoms again such as belching, flatulence and cramping. She also had a mild return of her skin problems. Overall, these symptoms were mild as compared to previously. However, she was very concerned about returning to her original condition. One possible explanation for the re-emergence was the fact that she had recently changed to a more stressful on-the-road sales job. She had high quotas and did not like her new boss. She was also eating on-the-run again, meaning some fast food. In other words, she was not maintaining the lifestyle and dietary changes that had served her so well, and her body was letting her know that.
We decided to aggressively treat the return of her symptoms. Since the patient had significant findings on her original stool analysis, I chose to retest the patient’s stool.
Discussion of Follow-up Diagnostics
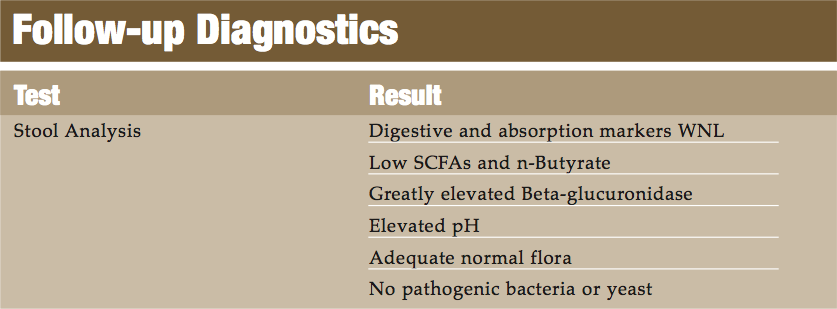
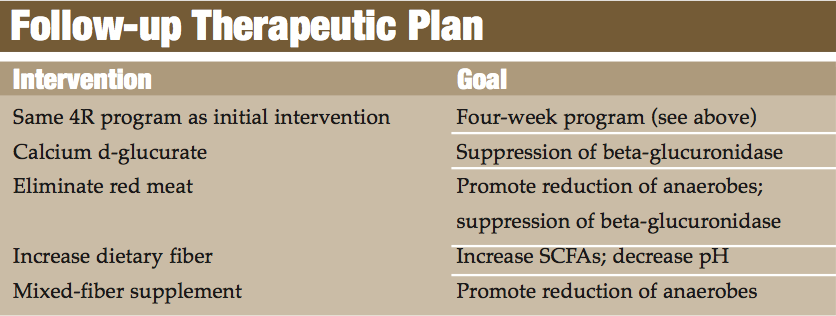
The follow-up stool analysis clearly displayed that the patient’s digestion and absorption improved dramatically. The pathogenic organisms originally detected were no longer present. However, an imbalance in the patient still existed. A lack of adequate levels of SCFAs always suggests that either there is not enough normal flora or an inadequate amount of dietary soluble fiber (SCFAs are mainly produced by the microbial fermentation of soluble fiber and starches). Since this patient clearly has adequate normal flora, lack of fiber was suspected as the cause.
The lack of SCFAs also resulted in an elevated stool pH. An elevated pH can create an environment favorable to various pathogens, particularly anaerobes such as bacteroides and clostridia. Standard stool analyses from the major American functional medicine laboratories do not measure anaerobic species, although they represent the predominant species in the gut and can cause significant clinical symptoms. These organisms can also result in larger amounts of various substances being produced such as beta-glucuronidase. In fact, this patient had a beta-glucuronidase level of 2348 IU/gm (70-1000 IU/gm). This bacterially derived enzyme will result in deconjugation of toxins that have been sent through the hepatic glucuronidation pathway that are attempting to be eliminated from the body via biliary excretion. The deconjugated toxin can now be reabsorbed into systemic circulation.
This phenomena is not totally abnormal or deleterious though. A certain amount of this enzyme needs to be present to facilitate enterohepatic recirculation of hormones such as estrogens. However, an imbalance in intestinal flora which results in elevated levels of this enzyme can ultimately increase toxic burden and tissue-hormone levels. In the case of estrogen, this can increase a woman’s risk for breast tissue proliferation and breast cancer. This situation was not detected on the original stool analysis since the beta-glucuronidase marker was not available when the original analysis was performed.
 Long-Term Management
Long-Term Management
This patient had an almost immediate resolution to her returning symptoms following the above program for a four-week period. She was able to maintain her improvement by reducing stress; eating a clean, non-processed food diet; rotation and limited consumption of corn, wheat, and dairy; and continued use of a quality multivitamin-mineral. I also decided to re-introduce a small dose of HCL and pancreatic enzymes with meals in an attempt to more adequately digest proteins into less antigenic forms. She was more than willing to follow this dietary and supplement program in order to avoid her previous condition.
Conclusion
This patient was chosen to illustrate the importance of the accurate detection and management of complex multi-symptom problems in patients with chronic health problems. Intestinal health, digestive function, detoxification, immune function and often adrenal/thyroid health all need to be evaluated and addressed in order to comprehensively treat these types of cases. If this is not done by the functional medicine practitioner, these patients are likely to be mismanaged and given “catch-all” diagnoses like fibromyalgia or chronic fatigue syndrome, when in reality they have very specific metabolic problems that can be accurately detected and adequately treated.
I would also like to point out the fact that this patient initially came to my practice without a job and without health insurance. Through the education she received from my office, she was able to come to terms with making her health a priority and making an investment in it. This meant actually using money from her savings account and borrowing from her family. She realized this was the only way to get well.
Her total expenditures, for her entire nine-month case, was approximately $2,000 to $2,500. She spent almost that much in one day for the gastroenterologist to tell her that “nothing was wrong with her.” She was more than happy with her investment. After all, what is it worth to re-enter society again, maintain a job, feel better, and to not live at home with your mother at 35 years of age?
 David M. Brady, ND, DC, CCN, DACBN is a licensed Naturopathic Physician and Clinical Nutritionist, He is the vice provost of the Division of Health Sciences, director of the Human Nutrition Institute, and associate professor of clinical sciences at the University of Bridgeport in Connecticut. He is also chief medical officer for Designs for Health, Inc., and maintains a private practice, Whole Body Medicine, in Trumbull, CT. Dr. Brady has been a featured presenter at many of the most prestigious conferences in integrative medicine, including IFM, ACAM, A4M, IHS, IAACN, AANP, and many more. He is a contributing author for Integrative Gastroenterology, the first integrative medical textbook on gastroenterology by Johns Hopkins physician Gerard Mullin, MD, and is also a contributing author for Laboratory Evaluations for Integrative and Functional Medicine, by Lord and Bralley, and Advancing Medicine with Food and Nutrients, Second Edition, by Ingrid Kohlstadt, MD.
David M. Brady, ND, DC, CCN, DACBN is a licensed Naturopathic Physician and Clinical Nutritionist, He is the vice provost of the Division of Health Sciences, director of the Human Nutrition Institute, and associate professor of clinical sciences at the University of Bridgeport in Connecticut. He is also chief medical officer for Designs for Health, Inc., and maintains a private practice, Whole Body Medicine, in Trumbull, CT. Dr. Brady has been a featured presenter at many of the most prestigious conferences in integrative medicine, including IFM, ACAM, A4M, IHS, IAACN, AANP, and many more. He is a contributing author for Integrative Gastroenterology, the first integrative medical textbook on gastroenterology by Johns Hopkins physician Gerard Mullin, MD, and is also a contributing author for Laboratory Evaluations for Integrative and Functional Medicine, by Lord and Bralley, and Advancing Medicine with Food and Nutrients, Second Edition, by Ingrid Kohlstadt, MD.