Clinical Rounds in Functional and Nutritional Medicine- Part Three: Hypertension and Adrenal Disorders
David M. Brady, ND, DC, CCN, DACBN
This is the third in a series of Clinical Rounds, which will be appearing as a part of ND News & Review. In these Clinical Rounds real case studies from my practice will be presented. It is my aim to present interesting cases, which will facilitate thought and discussion about novel diagnostic and therapeutic techniques for a myriad of clinical conditions that are likely to appear in your offices.
Patient Presentation and History:
The patient is a 50 year-old man who has been suffering from chronic essential hypertension for approximately seven years. His blood pressure has fluctuated between being significantly elevated and normal. His average reading has been approximately 150/102 even though he is on two anti-hypertensive medications (Toprol-XL 200 mg qd and Norvasc 5 mg qd) and potassium chloride. He had previously taken Diazide 75/50 mg qd. His past history also includes three episodes of kidney stones and a relative intolerance/allergy to cured pork. The patient is 6’0″ and weighs 190 lbs. He has been a teacher at a professional school for the past six years and is a trained surveyor by trade. The patient is a very active individual and is a permanent non-smoker. He consumes very little alcohol, usually less than a quarter of a drink each week on average. He apparently has a personality that is easy to anger. He does not have a significant family history for hypertension. The patient has had complications in taking his medications stating “the diuretics are raising havoc with my system.” The patient expressed a desire to more adequately manage his hypertensive condition with the addition of alternative and complementary therapies. His current problem list consist of:
- Hypertension
- Kidney Stones
- Pork Sensitivity
Prior Work-Up:
Results of two serum potassium studies (1/04/00 and 2/08/00) revealed low-normal levels. Alkaline phosphatase and AST/SGOT were normal when measured on 10/26/99, suggesting an absence of hepatocellular destruction, although no functional liver studies were performed. A urinalysis performed on 9/28/99 revealed some epithelial cells and some mucus. He had a history of a previous finding of hypokalemia while having a right ankle open reduction fixation surgery for a fracture five years prior.
Initial Impressions:
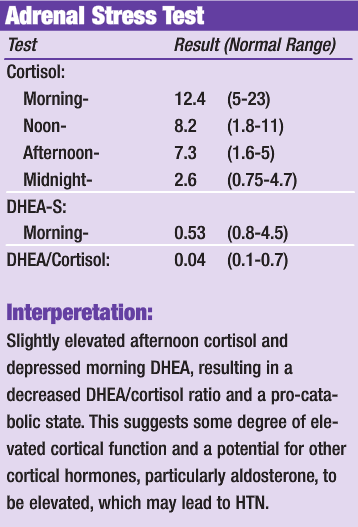
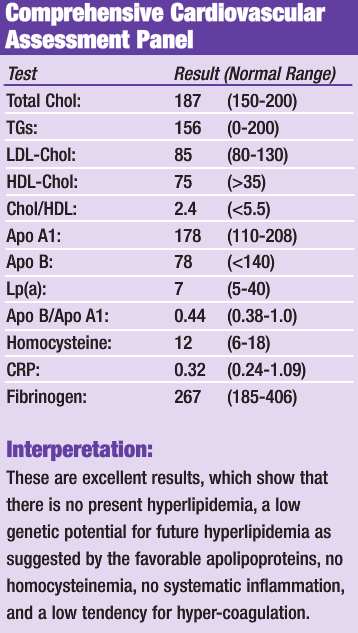
In the presence of this type of significant hypertension it is wise to assess this patient’s adrenal cortical function to determine if that may be contributing to his hypertension, particularly with his history of easily being stressed. This can be done by performing a salivary cortisol/DHEA-S level at several periods throughout the day with the Adrenal Stress Test from American Medical Testing Labs or Great Smokies Diagnostic Labs. I would also recommend that a comprehensive cardiovascular risk assessment be performed on him (ie: NMR Cardivascular Panel with lipid sub-class analysis by LipoScience, Inc. or the Cardiovascular Risk Profile by GSDL), which are much more comprehensive than a standard cholesterol, triglycerides, HDL and LDL panel. These tests, combined with a serum magnesium performed by any commercial lab, will go a long way toward determining this patient’s overall cardiovascular disease risk, and may help significantly in the choice of an appropriate therapeutic intervention.
Initial Diagnostic Work-Up:
Discussion of Diagnostics:
While the results of the adrenal stress test show some level of adrenal dysfunction, the results do not adequately determine if the adrenals are significantly contributing to the patient’s high blood pressure or if he is just suffering from common essential hypertension. More specific adrenal testing, such as aldosterone levels, would be required to fully determine the level of adrenal involvement. The adrenal results, combined with the very clean cardiovascular testing results, are supportive of a simple trial of natural therapeutics to support adrenal function, adaptation to stress, and to reduce essential hypertension. Prophylactic therapy for kidney stones will also be included. If positive results are not achieved, as evidenced by a reduction of the blood pressure, within a reasonable time frame, more advanced diagnostics will be performed.
Initial Therapeutic Plan:
- Adrenotone Plus* – adrenal support
- Hawthorne Berry (Cratagus oxycanthus) – HTN
- Magnesium – HTN
- Calcium – HTN
- CoQ10 – enhanced cardiac function
- Taurine – enhanced cardiac function
- Multi-vitamin & mineral – general support
- EPA-DHA (Omega-3 fatty acids) – blood thinning/lipids/inflam
- Limit sodium intake (processed foods, etc.) – HTN
- 2 qrts. water per day with the juice of 3 lemons – kidney stone prevention
- Stress reduction counseling – adrenal support
- Light aerobic exercise – stress reduction/wellness
- Macronutrient-balanced elimination diet – general/allergy
- low simple carbs
- moderate lean protein and complex carbs
- monounstaurated fats
*Adrenotone Plus is an adaptogenic herbal and nutritional product containing: Panax quinquefolius (American giseng), Eleutherosenticosus (Siberian ginseng), Withania somnifera (ashwagandha), Rhodiola rosea, Glycyrrhiza glabra (licorice), vitamins C, B2 (R5P), B6 (P5P), pantothenic acid, folate, and N-acetyl-tyrosine.
Adjunctive Therapy:
- Stress reduction and sleep counseling for adrenal health
- Deep breathing exercises
- Guided imagery instruction
- Instructions on proper and predictable sleep (in bed by 10PM, up by 7AM)
- Sun / light exposure first thing in morning with light activity
The above protocols were to be applied for at least 8-12 weeks in order to assess potential changes in blood pressure. Medication dosages have to be monitored in situations such as this and may have to be adjusted with the help of the primary-care physician if the program is successful. The diet and exercise program should be a long-term goal for the patient. This program was implemented with the full realization that if it did not yield significant results in the 8-12-week trial period, then further evaluation into causes of secondary hypertension, such as hyperaldosteronism, renal artery stenosis, hyperreninemia, and pheochromocytoma must be done. However, the lack of palpitations and flushing tends to rule against pheochromocytoma. If these further investigations, if necessary, should not produce an adequate explanation, then a consultation with a chelating physician would be in order to determine if chelation therapy would be appropriate. This is particularly true in cases of persistently elevated systolic pressures with relatively normal diastolic pressures, suggestive on non-compliance of the vessels. Given this patient’s extremely favorable cardiovascular health profile, this scenario of vessel non-compliance or significant atherosclerotic disease, is extremely unlikely.
Patient Follow-up:
Upon serial periodic follow-up examination it was determined that the patient’s blood pressure was not adequately being reduced or controlled via the medications alone, nor by the suggested natural protocol and his medications in combination. The patient was sent to his conventional medical physician for further diagnostic work-up. The following studies were suggested and performed on the patient:
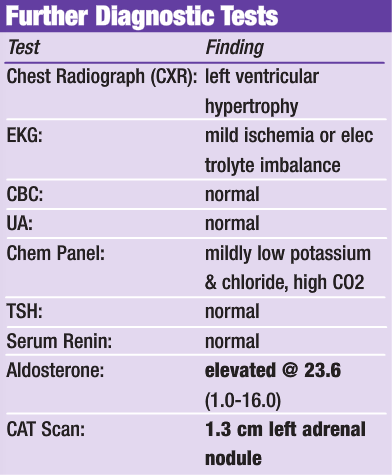
Discussion of Findings:
Based on the above findings, the patient was diagnosed with hypertension secondary to hyperaldosteronism. It was unclear whether the adrenal mass was cystic or if it represented an adrenal adenoma. The patient was put on Aldactone (100 mg bid). Aldactone contains spironolactone, an aldosterone antagonist, acting primarily through competitive binding of receptors at the aldosterone-dependent sodium-potassium exchange site in the distal convoluted tubule of the kidneys. Aldactone causes increased amounts of sodium and water to be excreted, while potassium is retained. Aldactone acts both as a diuretic and as an anti-hypertensive drug by this mechanism. The patient’s blood pressure and potassium levels were well controlled once this medication was prescribed. However, even though the patient was stable on this medication, he expressed a preference to have the functional adrenal mass removed to potentially cure his primary hyperaldosteronism and eliminate the necessity of remaining on long-term drug therapy. It was explained to the patient that the adrenal mass may not be functional, and even if it was, removal may not totally cure the hypertension. After contemplation, his decision was to go ahead and have the mass removed.
Surgical Intervention:
The patient underwent laparoscopic left-sided adrenalectomy. According to the surgeon, on gross examination there was an approximately 1 to 1.5 cm hard nodule present in the inferior aspect of the left adrenal gland with the remaining portion of the adrenal gland appearing grossly normal. The entire gland was successfully removed and the lesion was sectioned and sent for pathological assessment, which confirmed an adrenal cortical adenoma.
Post-Surgical Follow-Up:
Serial follow-up over the several months post-surgery revealed that the patient was essentially cured by virtue of the adrenalectomy. His blood pressures averaged in the 110s/70s in the months immediately after surgery and it was determined that he no longer needed any medications to manage his condition.
Conclusion:
This case perfectly illustrates that even though we may often be very successful in our nutritional and functional medicine interventions, we must always be diligent and aggressively reassess our patients in order to determine how successful we truly are in each and every individual case. In this particular situation, the patient was not responsive to his initial medical management with anti-hypertensive drugs alone. It was rational to try and add other integrated therapeutics to the patient’s treatment protocol, however, follow-up assessment revealed that this approach was also not providing satisfactory results.
Unfortunately, it is all too common that patients are given a treatment protocol and sent away, never to be seen again. In this patient’s case, that could have resulted in early morbidity and mortality. It would also be tempting to take the attitude that he had failed before with conventional medical management so why send him back? This too would have been a mistake. Careful contemplation of the physiology of blood pressure control lead to rational investigations into the potential causes of secondary hypertension and an eventual answer to this patient’s problem. While essential or primary hypertension accounts for well over 95% of cases of hypertension, it is advisable at times to consider the most probable reasons for secondary hypertension, particularly when the patient is refractive to normal hypertension therapy.
 Dr. Brady is a naturopathic physician, a board certified clinical nutritionist, and a doctor of chiropractic. Dr. Brady is the Chief Medical Officer of Designs for Health, Inc. and serves as a technical consultant to Metametrix Clinical Laboratory. He is also presently the Director of the Human Nutrition Institute at the University of Bridgeport, and an Associate Professor of Clinical Sciences at the University of Bridgeport, Colleges of Naturopathic Medicine and Chiropractic in Bridgeport, Connecticut. Dr. Brady also maintains a private practice at The Center for the Healing Arts in Orange, CT, where he specializes in “Functional and Metabolic Medicine”.
Dr. Brady is a naturopathic physician, a board certified clinical nutritionist, and a doctor of chiropractic. Dr. Brady is the Chief Medical Officer of Designs for Health, Inc. and serves as a technical consultant to Metametrix Clinical Laboratory. He is also presently the Director of the Human Nutrition Institute at the University of Bridgeport, and an Associate Professor of Clinical Sciences at the University of Bridgeport, Colleges of Naturopathic Medicine and Chiropractic in Bridgeport, Connecticut. Dr. Brady also maintains a private practice at The Center for the Healing Arts in Orange, CT, where he specializes in “Functional and Metabolic Medicine”.










