Geovanni Espinosa, ND, LAc, RH, CNS
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is of significant interest in urology and other health-related fields. Currently, there are multiple approaches to the management of CP/CPPS depending on the classification of the related symptoms. Although no absolute definitive findings or laboratory tests can identify it, prostatitis leads to more than two million visits to doctors’ offices in the U.S. each year and is the most common urological problem among men younger than age 50.
In 1995, the National Institutes of Health (NIH) established an International Prostatitis Collaborative Network in order to construct a new classification of prostatitis syndromes and better define chronic prostatitis. The categories are now documented as follows:
- Category I: acute bacterial prostatitis (ABP)
- Category II: chronic bacterial prostatitis (CBP)
- Category III: CP/CPPS – IIIA, inflammatory; IIIB, non-inflammatory
- Category IV: asymptomatic inflammatory prostatitis (AIP)
Category III
CP/CPPS accounts for 90% to 95% of prostatitis diagnoses (Habermacher et al., 2006). Men with this condition present with a long history (by definition, longer than three months) of genitourinary/pelvic pain with variable obstructive and irritative voiding symptoms and, perhaps, sexual dysfunction without any association with a bacterial infection cultured using standard microbiological techniques. Older terms still loosely used for this type of prostatitis are prostatodynia and non-bacterial prostatitis.
Patients’ complaints are various, including: “golf ball” in the rectum, pain above the pubic bone, pain between the scrotum and anus, pain in and around the tail bone, low back pain, groin pain, pain and burning during urination, urinary frequency, pain or discomfort after ejaculation, anxiety about sex, general anxiety and depression.
Diagnosis
Although CP/CPPS affects up to 95% of all prostatitis patients, there are no definitive tests to identify this health problem.
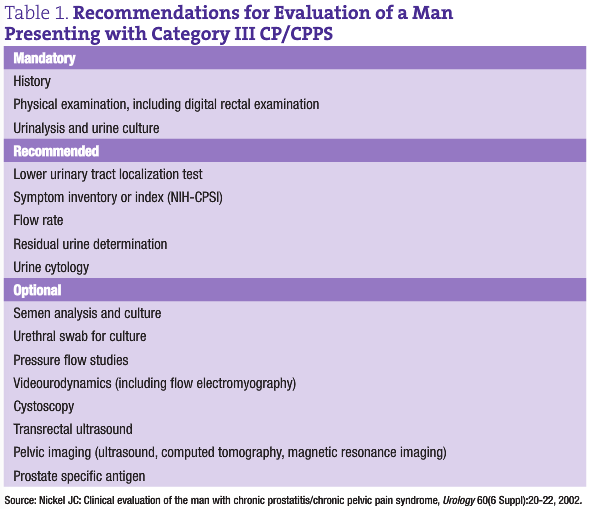
A complete history and physical examination including digital rectal examination and focused neurologic examination are mandatory. Urinalysis and urine culture are also mandatory, although they often come back negative. To rule out infection in the prostate gland (which is required to make this diagnosis), it is strongly suggested that a lower urinary tract evaluation be undertaken (at least for culture) using the Pre and Post Massage Test (PPMT) on patients with no clinical evidence of urethritis. Microscopic examination of PPMT urine sediment is of academic interest only at this time, because clinical studies have not been able to find associations between the inflammatory status of the lower urinary tract and type of prostatitis, severity of symptoms and differential response to therapy.
The PPMT is a simple, inexpensive test that may help diagnose the type of prostatitis the patient has. Prostate massage is done by milking two to three times from each side to the center sulcus and collecting urine pre and post massage. Both urine samples are then sent to the lab or studied in the office under a microscope in search of white blood cells. When microorganisms are the culprits, the most common is Escherichia coli. Other species frequently found include Klebsiella, Proteus, enterococci and Pseudomonas. On occasion, cultures grow Staphylococcus aureus, Streptococcus faecalis, Chlamydia or anaerobes such as Bacteroides species.
It is also strongly suggested that patients complete the NIH Chronic Prostatitis Symptom Index (CPSI). This symptom index, validated for symptom assessment in clinical trials, has proven invaluable in clinical practice as well (Propert et al., 2006).
This easy-to-administer questionnaire, which can be completed in five minutes by the patient, explores the three most important domains of the patient’s experience: pain (location, frequency and severity), voiding symptoms (obstructive and irritative) and, importantly, impact on quality of life. It allows the physician to follow the progress of the patient during and after therapy. The NIH-CPSI can be found in PDF format online.
Optional tests include abdominal and pelvic ultrasound, transrectal ultrasound, CT scan, urodynamics including videourodynamics, and other tests (see Table 1).
Cause
The cause and pathogenesis of CP/CPPS is not well understood, which leads to much frustration for patients as well as practitioners. This prevalent clinical condition appears with multiple manifestations of pain, urinary symptoms and sexual dysfunction but lacks any biomarkers, radiological imaging and reliable characteristics or consistent physical findings, making the disorder difficult for any targeted therapy.
The final result of the pathogenic process in chronic patients appears to be a neuropathic pain state involving central and peripheral neural and neuromuscular mechanisms. The initiator of this process could be any one of a number of things: infection in the lower urinary tract (including the prostate gland), dysfunctional voiding with resulting dyssynergia of the pelvic floor, reflux of sterile urine into the prostatic ducts and acini secondary to an anatomic variant, or something as simple as repetitive perineal or pelvic trauma (such as from a bicycle seat).
Once triggered, the process either stimulates inflammation or causes neuromuscular damage. Inflammation can promote secondary neurologic damage, while nerve injury can promote inflammation. Despite a common pathway for the pathogenesis of this condition, each patient presents with a slightly different constellation and severity of symptoms, and significantly different levels of aggravation. This finding appears to be regulated by coping mechanisms (adaptive and maladaptive), stress, anxiety and depression.
Treatment – Conventional Approach
Most well-intentioned urologists I have worked with dread seeing this type of patient population due to the low efficacy rate of conventional treatments. Once the tricks in their bag run out, physicians become as frustrated as their patients.
Traditionally, the therapy for nonbacterial chronic prostatitis syndromes has included antibiotics, anti-inflammatories, hormone therapy, antianxiolytic agents, muscle relaxants and, more recently, alpha-blockers. Results from prospective randomized data from clinical trials are not as favorable as we would like.
Antimicrobials are the main agents used for this “nonbacterial” condition on the premise that our culture techniques may not be picking up offending organisms, as well as on anecdotal experience that many patients actually do respond to antibiotics. However, most studies failed to show any significant benefit of these antimicrobials when compared with placebo.
A note on fluoroquinolones: This class of broad-spectrum antibiotics includes ciprofloxacin and levofloxacin, which can have debilitating side effects that include peripheral neuropathies and tendon damage. Just recently the FDA requested the manufacturers of these drugs to include a black-box warning label concerning the increased risk of tendinitis and tendon rupture. I have had CP/CPPS patients come in my office with major, debilitating peripheral neuropathies and severe extremity pain and have found myself treating these symptoms more than the prostatitis.
Treatment – Naturopathic Approach
Second to prostate cancer, the most common disease I see in my office is prostatitis. The typical naturopathic treatments that I find useful with these types of patients are:
- eradicating yeast/candida
- detoxing heavy metals
- elimination/challenge diet
- healing the gut
I would say about 40% of CP/CPPS patients I see have IBS or some other gastrointestinal issue. Also, many of these patients have been treated previously with multiple sessions of antibiotics, which often wipe out beneficial bacteria.
“When in doubt, treat the gut” is the traditional naturopathic saying that we all have grown to appreciate.
Anecdotal evidence suggests that food allergies and intolerances may play a role in exacerbating CP/CPPS, perhaps through mast cell mediated mechanisms. Specifically, patients with gluten intolerance or celiac disease report severe symptom flares after sustained gluten ingestion. Therefore, patients may find an exclusion diet helpful in lessening symptoms by identifying problem foods. Studies are lacking in this area.
Phytotherapy: As many as 30% to 60% of patients with chronic prostatitis treat themselves with herbal therapy or supplements. Many of these therapies do have significant in vitro anti-inflammatory activities, and several trials have indicated that they may be beneficial.
A small single-center pilot study evaluating quercetin showed significant benefit compared with placebo in patients with CP/CPPS (Shoskes et al., 1999).
A multicenter study testing the lipido-sterolic extract of Serenoa repens analyzed the response of S repens therapy in 61 patients with Category III-B prostatitis. While 65% of the S repens group reported improvement based on the Subjective Global Assessment (SGA); the total NIH-CPSI; and the pain, voiding and quality of life/impact domains of the NIH-CPSI; statistical significance was not reported (Reissigl et al., 2004). Since S repens is used primarily with patients with BPH, not too many other reliable studies are found with its use for prostatitis.
One available study testing pollen extract reported a 78% favorable response of men with chronic prostatitis taking a proprietary rye pollen extract at a dosage of 1 tablet TID for six months (Rugendorff et al., 1993). While this study reported favorable results, it was published in 1993 and similar subsequent larger-phase clinical trials are not evident to further elucidate the possible utility of pollen extract in men with CP/CPPS.
Acupuncture
Acupuncture is one of the main modalities I use to treat CP/CPPS, with moderate results. Although there were a small number of participants, several pilot studies have shown that acupuncture can be an effective treatment, bringing relief to patients including a decrease in pain, positive impact on quality of life and potentially inflammation modulation.
In one study, acupuncture was performed on the bilateral BL-33 points and rotated manually for ten minutes. The treatment was repeated every week for five weeks without other therapeutic maneuvers. Improvement overall was significant (Honjo et al., 2004).
A more recent randomized trial by Shaun Wen Huey Lee et al. (2008) used sham needles. Acupuncture proved to be almost twice as effective as sham acupuncture at easing symptoms of CP/CPPS. Sham acupuncture included the same number, duration and frequency of sessions as the acupuncture group at non-acupoints (superficial and 15mm to the left of each corresponding acupoint).
The points selected in this trial included CV-1, CV-4, SP-6 and SP-9. Treatment consisted of twice-weekly, 30-minute sessions for ten weeks without needle stimulation.
Proteolytic Enzymes
Although I could not find any studies on the use of proteolytic enzymes for CP/CPPS, some sufferers (not patients of mine) have reported to me via phone or e-mail symptom-free results using proteolytic enzymes that include: bromelain, chymotrypsin, trypsin and papain on an empty stomach TID, three to ten tablets at a time.
Stanford Protocol for Prostatitis
A new treatment for prostatitis called the Stanford Protocol has been developed at the Stanford University Urology Department by Rodney Anderson, MD, professor of urology at Stanford Medical School and David Wise, PhD, former research scholar at Stanford Urology Department. This new treatment is described in the book A Headache in the Pelvis.
This Stanford researcher team does not treat prostatitis as a disease of the prostate gland. Instead, the Stanford Protocol relies on research that shows that the prostate gland is normal in the large majority of men carrying symptoms of prostatitis. The Stanford treatment focuses on relaxing chronic tension and releasing spasm in the pelvic muscles.
There are two parts to the Stanford protocol: myofascial/trigger point release and paradoxical relaxation:
- Myofascial trigger point release is a self-administered physical therapy performed inside and outside the pelvic floor. It identifies more than 60 trigger points inside and outside the pelvis that can refer pelvic pain and symptoms. This method aims to free the muscles in and around the pelvis of active trigger points and to restore the muscles of the pelvic floor to a flexible and lengthened state.
- The purpose of paradoxical relaxation is to teach a patient to profoundly relax the tensed and shortened muscles within the pelvic floor basin associated with certain kinds of pelvic pain. Paradoxical relaxation has two components: a breathing technique used at the beginning of relaxation, and instructions given for the remainder of the relaxation session directing patients to focus attention on the effortless letting go of tension in a specified area of the body and accepting residual tension that does not easily release. In addition, patients are asked to listen to approximately one hour of recorded relaxation instruction daily focusing on individual predetermined anatomical sites including the jaw, neck, shoulders, arms, etc. Relaxation instruction guides the patient to rest attention in sensation and to redirect attention away from discursive thinking and daydreaming.
Reviewing all the complex details of this approach is beyond the scope of this article but can be found in the aforementioned book.
Prostate Massage
It has been said that one of Dr. Bastyr’s treatments for prostatitis was prostate massage. Before antimicrobial agents were available for chronic prostatitis, “prostate milking” was the mainstay of therapy.
Although prostate massage is a commonly used treatment along with the use of mainstream agents like antibiotics or herbal therapies in countries like the Philippines (Nickel et al., 1999) and China (Yang et al., 2008), it is not a common treatment in the U.S. One U.S. study published in Urology showed no significant benefit with prostate massage compared to antibiotics alone (Ateya et al., 2005).
Prostate massage is not a risk-free treatment and should not be performed on patients with acute prostatitis. Some documented consequences are life-threatening periprostatic hemorrhage (Buse et al., 2003), cellulitis, Fournier’s gangrene (Sengoku, 1990) and septicemia. Some theoretical possible adverse events include disturbance and metastasis of prostate cancer, and hemorrhoidal flareup.
Summary: Treating CP/CPPS Patients
- Be compassionate and understanding: These patients’ social and sexual quality of life is significantly altered by their symptoms. The impact of their symptoms have been compared to those of patients with Crohn’s disease.
- Natural anti-inflammatory diet: Three main foods that I have these patients eliminate are simple sugars, gluten and dairy. Other foods may be culprits as well, but I have found these to be the main ones. An elimination/challenge diet can be helpful in the determination of offending foods.
- Acupuncture: The main points I have used with moderate success (significant relief or resolution of symptoms as measured by the NIH-CPSI) include: BL-23, BL-25, CV-2, CV-4, SP-6, SP-9, LV-2 or LV-3, KI-3, KI-10, LV-4. I would choose the appropriate points and pattern for each treatment depending on the symptoms and the TCM diagnosis. Each treatment lasts about 30 minutes, with some stimulation after 15 minutes.
- Supplements: formulas that include proteolytic enzymes, curcumin, quercetin and Boswellia. Other agents include: Fish oil (4-5g/day), probiotics and magnesium.
- Deep breathing exercise: Many of these patients live a stressful life – partially due to their lifestyle and partially due to their symptoms. I ask them to “go to timeout” (I have two young kids, the father in me comes out sometimes) three times a day and take ten deep breaths, consciously relaxing the pelvic muscles as follows: They should inhale through their nose for a four count, expanding their belly outward (not their chest), hold their breath for a two count, and then exhale out through their mouth for a four count, flattening the belly. In my experience, many prostatitis patients do not breathe correctly, which may propagate the problem.
- Ba zheng san (Eight Righteous herbs) – this TCM formula consists of: Mu Tong (caulis mutong), Hua Shi (talcum), Che Qian Zi (semen plantaginis), Qu Mai (herba dianthi) Bian Xu (herba polygoni avicularis), Zhi Zi (fructus gardeniae jasminoidis), Zhi Da Huang (treated radix and rhizoma rhei), Deng Xin Cao (medulla junci effusi), Gan Cao (radix glycyrrhizae uralensis). This formula is sometimes modified depending on symptoms and TCM pattern. For example, when a CP/CPPS patient presents with significant pain, I add 15-30g of Yan Hu Suo (Corydalis cava rhizome; a major TCM herb for pain). I find TCM decoctions to be more effective than pills or granules. Many practitioners assume that patients will not drink these strong, bitter decoctions; however, I have found that CP/CPPS patients are willing to do anything that will help them resolve their life-altering prostatitis symptoms.
 Geovanni Espinosa, ND, LAc, RH, CNS is director of clinical trials and co-investigator at the Center for Holistic Urology, Department of Urology – Columbia University Medical Center (CUMC). He earned his naturopathic medical degree and masters degree in acupuncture from the University of Bridgeport. Upon graduation, Dr. Espinosa did his residency in urology at Washington Heights Urology (an affiliate of CUMC) and continued it at CUMC under Dr. Aaron Katz. His research and practice is exclusive to urology and men’s health.
Geovanni Espinosa, ND, LAc, RH, CNS is director of clinical trials and co-investigator at the Center for Holistic Urology, Department of Urology – Columbia University Medical Center (CUMC). He earned his naturopathic medical degree and masters degree in acupuncture from the University of Bridgeport. Upon graduation, Dr. Espinosa did his residency in urology at Washington Heights Urology (an affiliate of CUMC) and continued it at CUMC under Dr. Aaron Katz. His research and practice is exclusive to urology and men’s health.
References
Habermacher GM et al: Prostatitis/chronic pelvic pain syndrome, Annu Rev Med 57:195-206, 2006.
Propert KJ et al: Responsiveness of the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), Qual Life Res 15(2):299-305, 2006.
Shoskes DA et al: Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial, Urology 54:960-963, 1999.
Reissigl A et al: Multicenter Austrian trial on safety and efficacy of phytotherapy in the treatment of chronic prostatitis/chronic pelvic pain syndrome, AUA 98th Annual Meeting: Abstract 103937. Presented April 26, 2003.
Rugendorff EW et al: Results of treatment with pollen extract (Cernilton N) in chronic prostatitis and prostatodynia, Br J Urol 71(4):433-438, 1993.
Honjo H et al: Effects of acupuncture for chronic pelvic pain syndrome with intrapelvic venous congestion: preliminary results, Int J Urol 11(8):607-612, 2004.
Lee SW et al: Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain, Am J Med Jan;121(1):79.e1-7, 2008.
Nickel JC et al: Repetitive prostatic massage therapy for chronic refractory prostatitis: the Philippine experience, Tech Urol Sep;5(3):146-151, 1999.
Yang J et al: Chinese urologists’ practice patterns of diagnosing and treating chronic prostatitis: a questionnaire survey, Urology Jul 1, 2008. [Epub ahead of print].
Ateya A et al: Evaluation of prostatic massage in treatment of chronic prostatitis, Urology Apr;67(4):674-678, 2006.uiyhb
Buse S et al: Prostate massage with unwanted consequences. Case report [translated], Urologe A Jan;42(1):78-79, 2003.
Sengoku A et al: A case of Fournier’s gangrene: was it triggered by prostatic massage? [in Japanese], Hinyokika Kiyo 36(9):1097-1100, 1990.

