Rethinking the Problem
Phranq D. Tamburri, NMD
This year I’ve been focusing on prostates, “evil” fish oil, PCA3, tigers, and Harley Davidson motorcycles. I feel honored to contribute each year to the annual updates and changes regarding prostate cancer (CaP) screening and its treatment. This topic has seen unprecedented upheavals among the conventional medical community, in terms of how CaP is assessed and managed. The alternative medical community for years has added fuel to this debate, with regard to distrust of the Prostatic-Specific Antigen (PSA) serum test and the safety of prostate biopsies. Add to this the radical changes in the federal government’s stance on the PSA test (US Preventive Services Task Force in 2012)1 while it concomitantly undergoes an overall organizational and financial restructuring of the entire US health care system under the Patient Protection and Affordable Care Act (“ObamaCare”), and the resulting controversy this past year has become even more interesting than the prior year.
As a specialist in prostate cancer assessments, I will attempt in this article to illustrate both the objective and subjective changes noted during this past year.
PCA3 Testing has “Grown Up”
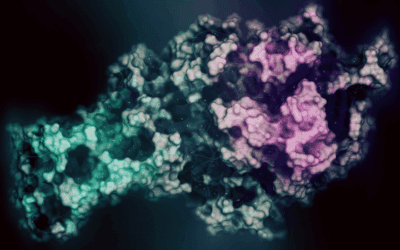
Over many prior NDNR issues, we have described the introduction of a new CaP genetic (mRNA) molecular screening lab test, the Prostate Cancer Antigen-3 (PCA3). When I first began using this test 6 years ago, it was still “underground” among urologists I worked with who specialized in Active Surveillance (“watchful waiting”). This was because it was not yet approved by the US Food and Drug Administration (FDA), improved reliability data was not yet concluded, only one urologist laboratory offered it, and the price point was $1400. Nevertheless, I had patients often flying to my office simply to have it performed, with or without a CaP diagnosis.
The PCA3 test is now mainstream. In late 2011, the test was approved by the FDA2 and subsequently offered by numerous competing non-urologist laboratories. In the summer of 2012, the US Preventive Services Task Force officially recommended against PSA as a screen for CaP (dropping it from “A” and “B” recommendation status, to a literal “D”), thereby putting increased pressure on both patients and doctors to find an alternative screening option. The price for the PCA3 test has significantly decreased to around $200 for cash payment in most cases. The sensitivity of PCA3 has ranged from 46.9% to 82.3% in various studies, usually using the traditional cutoff score of 35.3 These values are not optimal, but given the reliability of a single PSA screen, PCA3 was a welcome option. In February of 2012, the FDA approved a lower cutoff of 25 for triggering biopsy.4 However, the optimal cutoff score remains controversial; although higher cutoffs reduce the number of unnecessary biopsies (false-positives), they also result in more prostate cancers being missed (false-negatives).5 In a community-based study of 1913 men with either elevated PSA or abnormal DRE, Crawford et al4 found that a PCA3 cutoff of 10 reduced the number of false-positives by 35.4%, whereas false-negatives only increased by 5.6%. Although the PCA3 is still an uncommon test for most physicians to perform, it is now much more accessible to those integrative physicians that regularly see CaP patients. Keep in mind that this test does not diagnose a CaP, but does technically provide an estimation of the chance of finding CaP on a biopsy.
Hyperthermia: “New” Wonder Treatment, or Fad?
The year 2013 saw the reemergence of a low-invasive prostate cancer treatment that has been sidelined by the FDA for decades: transurethral prostate hyperthermia.6,7 This section is not intended to promote this procedure, which at this time is only available in Germany and Canada, but only to acknowledge that this procedure has rapidly become the most talked-about and searched-for procedure among the Active Surveillance doctors and patient chatrooms. A probe is inserted through the urethra and into the prostate where short waves are pulsed, causing the cells to reach a temperature of 45-70 °C for 60 to 180 minutes, typically for 2 sessions, depending upon the prostate volume. The concept is that this directed heat will disrupt the circulation to the cancer cells so that they either die or mitosis is reduced. Unlike transurethral prostate cryotherapy that destroys the entire gland with cold (using liquid halogen gas), this procedure leaves the prostate intact, with very few lasting side effects. Technically, it is neither a surgical procedure nor a retention treatment such as brachytherapy or IMRT. As a result, the prostate is not destroyed to the point that a future radical prostatectomy is ruled out, as is typically the case using conventional options.
Although the evidence-based outcome studies to date are not yet to the satisfaction of the FDA, integrative patients who are seeking an aggressive technical procedure with low side effects are recently turning towards this option and often traveling far for it. Interestingly, I have found some naturopathic physicians who have considered this procedure in their practice, but the technology has been sequestered by the FDA for decades, it seems. Due to its recent resurgence, new safety and early-outcome studies for hyperthermia are beginning at an American hospital.
As a final note, as in many areas of medicine, new techniques are constantly investigated. And when a new procedure or device is being investigated or becomes available, it is often touted as superior to what is currently available. Initially, the “evidence-based” results often convincingly support these claims. New CaP treatments are no exception. However, physicians should be vigilant in noting that when a new (and expensive) treatment is being reviewed for approval, both the physicians promoting the technique and the manufacturers of the new device or method often have much to lose if it does not perform superior to current standard treatments. Therefore, patients chosen for these new treatments are often “cherry picked” for their lack of complicating factors. In trials examining new CaP procedures, candidates often have a lesion that is staged at T2 or less, and a “normal” prostate volume (under 80 cc in BPH). With this “new technique approval bias” acknowledged, hyperthermia is still showing interest and promise because some practitioners have performed this technique for over 10 years without stringent patient acceptance restrictions. One further protocol for hyperthermia adds on 6 months of hormone ablation therapy (eg, bicalutamide) following the procedure. On a clinical note, although I do not yet actively endorse this procedure, in a total of 3 patients whom I have assessed with laboratory (PSA kinetics, PCA3) and color doppler transrectal ultrasound post-treatment, a significant decrease in both lab values and color doppler intensity was identified, without any notable side effects to date. However, 2+ year outcomes have not yet been tracked from my office.
Fish Oil Causes Prostate Cancer? Really?
Most integrative practitioners have been informed of the July, 2013, study announced by Dr Theodore Brasky in the Journal of the National Cancer Institute (JNCI).8 This study concluded that an elevated intake of omega-3 fish oil can increase risk of prostate cancer.
So, what, exactly, is wrong with the study? Where to begin?
Most readers will likely be shocked to learn that investigators for this study did not give a monitored and controlled fish oil supplement to a cohort of men and then find some years later that the men taking fish oils were diagnosed or dying of prostate cancer more than men who did not take the oil. In fact, no fish oil supplementation was given at all! Instead, the study extrapolated leftover data from a very large 2002 study (SELECT = Selenium and Vitamin E Cancer Prevention Trial)9 that had concluded after 5 years that neither vitamin E nor selenium prevent CaP.10 Researchers of the JNCI fish oil study simply retrospectively data-mined the SELECT study for any possible correlations.
In this retrospective study, investigators analyzed miscellaneous factors that the high-CaP-incidence group might have had over those without CaP. One finding was that the increased CaP-incidence group had higher levels of DHA (docosahexaenoic acid), which is only one component of a balanced fish oil blend (ignoring EPA and ALA). So, participants who, back in the period of 2001 to 2008, for some reason, had more DHA in their blood were grouped together and analyzed for CaP incidence. This fact is critical to the controversy, but the key point, again, is that no fish oil was ever specifically administered or analyzed in a study that nonetheless made their conclusion about fish oil. Ie, this study was based upon perceived observation of data, not experimentation.
The levels of DHA in the blood that were labeled “elevated” were not the typical levels seen when patients taking fish oil are specifically monitored. If fish oil supplements had been taken, then EPA (eicosapentaenoic acid) would also be expected to be elevated in this cohort. Furthermore, omega-3 values have been shown to be affected by genetics and metabolism, yet this was never accounted for. Finally, the researchers, themselves, stated that the patients were not, for the most part, supposed to be taking other natural supplements (including fish oil), since the study was trying to isolate the effects of vitamin E and selenium on CaP.
An ancillary but not publicly reported finding from the JNCI study is that trans fats were highest in the group of men having the least amount of CaP! Flippantly speaking, the conclusion should now suggest that to prevent prostate cancer, one must stop eating fish but consume French fries. (?!)
Studies that are critical of natural treatments are often automatically dismissed or faulted by a reactionary (but often correct) integrative medical community. However, the JNCI finding has not only elicited explosive reactions and controversy among integrative practitioners, but in the conventional community as well.11 Most mainstream CaP awareness organizations have decried the finding as simply a misconstruing of the results. These include the American Cancer Society and the Prostate Cancer Research Institute, among others. Despite the years of evidenced-based, peer-reviewed conclusions that inflammation is linked to cancer and that fish oil can reduce inflammation (among other benefits), the JNCI study drew an opposite conclusion, without even using fish oil in their study.
Correlation is NOT Causation
The JNCI study, and the furor it produced in the preventive medicine community, highlights an extremely critical point in analyzing study outcomes: correlation is NOT causation. This is particularly relevant with regard to CaP causation studies, given the evolving view of this pathology. For most patients, the diagnosis of CaP is discovered upon a biopsy, performed because of an elevated PSA. Men are routinely checked for PSA levels. Those with elevated levels are biopsied. Since random biopsies often reveal “random” indolent CaP (detailed below), these patients will very likely be diagnosed with at least a few cancer cells; technically, they “have” CaP. Therefore, an increase in routine prostate biopsies based on PSA values will identify an increase in CaP incidence. An elevated PSA will consequently be correlated with a higher incidence of CaP. Of course, in most cases PSA values are elevated for non-cancerous reasons, with prostatitis and benign prostatic hyperplasia (BPH) being the most common (in that order). Therefore, increases in PSA do not necessarily indicate increased risk of CaP, though these other factors are typically discounted and trumped by a controversial and potentially litigious cancer diagnosis. The common interpretation has been that men with elevated PSAs have a high risk of CaP.
Do Harley Davidson Motorcycles Cause CaP?
Imagine returning years later to the original 2002 study (like the JNCI study did) and then retroactively identifying those test subjects who happened to have ridden Harley Davidson motorcycles. Most likely, the rider cohort will have slightly elevated PSA levels, since prostatitis is more common with motorcycle riding. With higher PSA levels, this group will more likely have been biopsied. Again, this increase in routine biopsy based on PSA would identify an increase in CaP incidence. Therefore, the net finding and headline could be: “Men who ride motorcycles have higher incidence of prostate cancer.” Of course, this is not true and simply reflects the mistaken assumption that correlation equals causation.
A true case study I had was of a man with a PSA of 15 ng/mL, who was then biopsied and diagnosed with CaP. Radical prostatectomy was immediately scheduled and was imminent. After visiting my office and taking a thorough history, a radically different story emerged. It turned out that his PSA was taken in an emergency room following a catheter insertion due to a seized and spastic prostate gland during a cross-country tour on his new Harley Davidson motorcycle. His PSA 2 weeks before the trip was 2.1 ng/mL. His CaP diagnosis was actually a Gleason 6 (lowest grade), and in less than 1% of only 1 core out of 12 (the most benign “positive” reading possible). Two months of prostatitis treatments reduced the PSA back to 1.4 ng/mL, and all other test parameters were eventually negative for CaP. Surgery was avoided in this case. This case study suggests that this patient’s CaP was indolent (ie, non-lethal, low “aggression”) and was probably always present without any known sign or symptom to the patient. The elevated PSA was a “red-herring,” based on the false assumption that his PSA value was linked to the “CaP.”
Is Most CaP “Indolent”?
Of course, the case study above provocatively asks men a very “modern” question in understanding oncology: “Might we all have CaP in us all the time?” This is a controversial concept that is challenging to prove. However, there is a growing body of evidence, both direct and indirect, to support this.
From an evidence-based perspective, this question is being confronted head-on through investigation into the incidence of CaP. The National Cancer Institute’s SEER data (Surveillance Epidemiology and End Results) demonstrate that CaP has been detected in exceedingly more patients after the PSA blood test was introduced in 1985 than prior to it.12,13 At the same time, however, the incidence of mortality from CaP did NOT increase accordingly (see Figure 1) and, in fact, declined.14 Unless a coincidental mysterious CaP “contagion” entered America’s drinking water in 1985, this data suggests that a significant amount of cancer always existed. It further suggests that all those men with CaP prior to 1985 likely never even knew they had it and had died of some other cause. Put another way, CaP likely existed in higher numbers of men than it killed (indolent CaP). This situation has persisted for an unknown number of years prior to 1985, simply due to the lack of any form of early detection for these indolent cancers.
Is Cancer “Normal”?
Consider the fact that indolent prostate cancers only now “exist,” due to decades of reflexive biopsies, often for the wrong reasons. Can we not then further argue that if this is true for CaP, then why not for other forms of cancer, in other organs, for which we do not yet have an early warning detection test? For example, do we have a “PSA” test for kidney cancer that could lead to countless reflex biopsies? No. Do we have a way to palpate other organs, like we do with the prostate? What if we could somehow conduct a “DRE” of the pancreas, as we do the prostate? Think of all the undetectable yet indolent cancers that might exist in the typical human being, within each of these organs. This concept may be difficult to prove empirically; however, the lessons learned from the overdiagnosis of CaP may illustrate new ways to consider cancer. Medical experience and biological wisdom are illuminating cancer much differently than it was previously pigeonholed – as the biological “boogeyman.”
Is CaP a “Weaker” or “Better” Form of Cancer to Get (Since It Does Not Kill Most Men)?
This question is commonly answered in the affirmative by patients and even some practitioners, but reflects the lack of understanding of the uniqueness of the CaP diagnosis. I believe this notion is false, that CaP, as a whole, is not significantly different than other cancers, in terms of mortality risk. As hinted above, humans likely have indolent cancer within most, if not all, of our body organs at some point. Although some of these cancers may eventually become active (for whatever reason), most may remain indolent. What sets CaP apart, however, is that only CaP currently has 2 unique “early-detection” tests, ie, both a palpation (digital rectal exam) and a serum blood test. Renal cancer, for example, has neither. Nor does pancreatic or bladder cancer. Therefore, most cancers are only detected when they enter an active stage, and most likely at that point (when physical symptoms are realized) are already metastatic. As a result, these other cancers are often mistaken as more aggressive than CaP. Actually, I believe that all cancers are relatively equal in potential activity and mortality; that is, every cancer may have an indolent form that, in the minority of cases, is followed by an “aggressive” and lethal form. The false sense of security by many that CaP is inherently “weak” is, I believe, the current result of excessive detection of the indolent form of CaP. It is my professional opinion that if physicians began to biopsy everyone’s pancreas at the same excessive rate that they biopsy the prostate, the pancreas might mistakenly join the prostate as a perceived “weaker” cancer.
Can Cancer Be “Good”?
After a patient has been diagnosed with CaP on biopsy but chooses to follow Active Surveillance, there is typically an understandable discussion with him about his risk tolerance for continuing to follow and track the potential progression of the disease. A stable comfort level and consent must be obtained with these patients so that they can handle the anxiety in knowing that a cancer resides in them. At my office, I further explain how they can both visualize and ultimately accept living with an indolent CaP, if they choose.
For instance, I have them consider America 100 years ago. As an example, my Italian-immigrant grandparents lived in tight row homes in Philadelphia. If a neighbor was sick with an “infection,” the house was roped off and quarantined. Neighbors would walk on opposite sides of the street and children were often not even allowed outside. “Infection” and its associated bacteria were not well understood, but simply feared. Later, when antibiotics were introduced, they were enthusiastically used immediately and redundantly, to the point that bacterial resistance and side effects eventually occurred. After clinicians had years to better study and learn about bacteria and the adverse results of overtreating, the realization emerged that “we naturally always have bacteria in us!” This concept was later labeled for lay audiences as “good bacteria.” Subsequently, a cottage industry developed, such as yogurt companies promoting how much bacteria they were selling you! I ponder what my grandparents would have thought of the concept of paying for bacteria?!
Our understanding of cancer, being led by the debate over prostate cancer incidence versus mortality, is likely following a similar pattern. Currently, a patient who is diagnosed with cancer will often associate this diagnosis with an incurable metastatic form, along with the stereotypical chemotherapy, subsequent hair loss, muscle weakness, pain, and eventual death. Yet this stereotype may, in reality, be the minority situation, as indolent CaP assessments are currently demonstrating. I see the medical community becoming more comfortable with recognizing the likely dominance of indolent cancer variants. Better screening tests will be developed for all cancers, and physicians will become more comfortable with an Active Surveillance approach, where reactionary cancer removal or destruction is limited. I see a pattern for cancer acceptance and understanding that is similar to the learning curve regarding bacteria. Of course, a very fair question I am asked is, “Well, then, is there such a thing as “good” cancer?” Although it is too early to tell, I believe a rethinking will be eventually realized. Consider that cancers in some organs have been shown to develop enzymatic skillsets that resemble an almost intelligent purpose. For instance, some breast cancers “suddenly” construct organ-specific enzymes that specifically attack the defenses of the surrounding breast tissue. This begs the question of whether cancer is not necessarily some “berserk zombie” mutation, but instead is a unique “life.” If this is true, then medical science has much to learn in reestablishing our relationship with these “beings.” Even the National Cancer Institute has slowly changed its mantra of “The War on Cancer” to “Living with Cancer.” Indolent cancers like CaP suggestively demonstrate that a significant amount of cancer is coexisting with us, rather than opposing us. What this purpose is will likely be reserved for the future medical community to discover.
The year 2012 turns out to have been an intriguing and significant one, with regard to CaP assessment and its treatment considerations. Although new evidence-based assessment tools and treatment options have been introduced and debated, it is profoundly the larger, conceptual re-thinking of CaP that has trumped it all. And most exciting is that, due to the unfortunate decades of unnecessary biopsies, and the brave patients who read the new research on mortality incidence and chose the more harrowing option to live with cancer, physicians such as myself are learning a new language set and comfort level when dealing with CaP. For example, seeing a large tiger growling in your back yard would reflexively cause you to immediately shoot it out of fear (immediate prostate surgery). However, if you spent months on a safari observing tigers in their natural habitat, after awhile you would learn that a growl might just mean a yawn or playing. You canヘt learn to live with a tiger (or cancer!) until you know its ells,rt level for doctors that slowly develops from it, will likely, and excitingly, become the vanguard for the future re-thinking of cancer.
 Phranq D. Tamburri, NMD is medical director for Prostate Second Opinions (PSO). As a 3-office international practice, PSO is a specialty service dedicated to assessing prostate cancer treatment options from Active Surveillance, to surgical, and natural. Dr Tamburri is a graduate from the Southwest College of Naturopathic and Health Sciences (SCNM), 2001. He was resident and chief resident, and eventually the first naturopathic physician to conduct rounds with Mayo Clinic urologists. Prior schooling was at Penn State, Temple University (masters degree), and eventually Kansai Gaidai, Japan. Outside of medicine, he lectures on Austrian Economic vs Keynesian theory and, as an INTJ, the Myers-Briggs Personality Type Indicator.
Phranq D. Tamburri, NMD is medical director for Prostate Second Opinions (PSO). As a 3-office international practice, PSO is a specialty service dedicated to assessing prostate cancer treatment options from Active Surveillance, to surgical, and natural. Dr Tamburri is a graduate from the Southwest College of Naturopathic and Health Sciences (SCNM), 2001. He was resident and chief resident, and eventually the first naturopathic physician to conduct rounds with Mayo Clinic urologists. Prior schooling was at Penn State, Temple University (masters degree), and eventually Kansai Gaidai, Japan. Outside of medicine, he lectures on Austrian Economic vs Keynesian theory and, as an INTJ, the Myers-Briggs Personality Type Indicator.
References
- U.S. Preventive Services Task Force. Screening for Prostate Cancer: U.S. Preventive Services Task Force Recommendation Statement. May, 2012. http://www.uspreventiveservicestaskforce.org/prostatecancerscreening/prostatefinalrs.htm. Accessed July 15, 2013.
- U.S. Food and Drug Administration. Progensa PCA3 Assay. February 13, 2012. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm294907.htm. Accessed July 15, 2013.
- Filella X, Foj L, Milà M, et al. PCA3 in the detection and management of early prostate cancer. Tumour Biol. 2013;34(3):1337-1347.
- Crawford ED, Rove KO, Trabulsi EJ, et al. Diagnostic performance of PCA3 to detect prostate cancer in men with increased prostate specific antigen: a prospective study of 1,962 cases. J Urol. 2012;188(5):1726-1731.
- Barbera M, Pepe P, Paola Q, Aragona F. PCA3 score accuracy in diagnosing prostate cancer at repeat biopsy: our experience in 177 patients. Arch Ital Urol Androl. 2012;84(4):227-229.
- Gould D. Hyperthermia and Electrochemical Therapy at St. Georg Hospital, Germany: Friedrich Douwes, MD’s Innovative, Intergrative Cancer Care. Alternative & Complementary Therapies. 2001;7(5):291-295.
- Douwes FR, Lieberman S. Radiofrequency Transurethral Hyperthermia and Complete Androgen Blockade: A Nonsurgical Approach to Treating Prostate Cancer. Alternative & Complementary Therapies. 2002;8(3):149-156.
- Brasky TM, Darke AK, Song X, et al. Plasma Phospholipid Fatty Acids and Prostate Cancer Risk in the SELECT Trial. J Natl Cancer Inst. 2013;105(15):1132-1141.
- Southwest Oncology Group. Selenium and Vitamin E in Preventing Prostate Cancer (SELECT). ClinicalTrials.gov identifier: NCT00006392. Last updated October 12, 2012. http://clinicaltrials.gov/show/NCT00006392. Accessed September 6, 2013.
- Lippman SM, Klein EA, Goodman PJ, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA. 2009;301(1):39-51.
- Bowden J. Media Madness: Fish Oil Supplements Cause Prostate Cancer! July 17, 2013. Huffington Post Web site. http://www.huffingtonpost.com/dr-jonny-bowden/fish-oil-prostate-cancer_b_3601906.html. Accessed August 15, 2013.
- Surveillance Epidemiology and End Results. Prostate Specific Antigen Testing. National Cancer Institute Web site. http://seer.cancer.gov/studies/surveillance/study6.html. Accessed August 15, 2013.
- Potosky AL, Miller BA, Albertsen PC, Kramer BS. The role of increasing detection in the rising incidence of prostate cancer. JAMA. 1995;273(7):548-552.
- Bartsch G, Horninger W, Klocker H, et al: Prostate cancer mortality after introduction of prostate-specific antigen mass screening in the Federal State of Tyrol, Austria. Urology. 2001;58(3):417-424.