Andrea Gruszecki, ND
There is a growing debate in our profession about how we, as NDs, move into the 21st century. I continue to read NDNR articles by Dr. Robert Kellum that urge a return to our roots (which I support wholeheartedly), but through a specific philosophy/modality called anthrophosophy. While I do believe that a return to our roots is a necessary step if we are to survive as a profession, I do not believe and cannot support that any one person’s favorite therapy or philosophic perspective is the “one size fits all” cure that our profession requires. One of the biggest problems naturopathy faces is getting us all to agree about what it is. Since naturopathy includes many different modalities, what we really need as a profession is an underlying structure that supports all of us and clearly identifies our model of medicine to patients and other providers.
My greatest disappointment in naturopathic medical school, even as I was learning the history and philosophy of Naturopathy, was that no one was teaching me a basic model of health that explained and included all of this information and all of the modalities I was being taught. There was no model of medicine to help me discern physical from mental, emotional, spiritual or energetic root causes, and no guidance beyond my own instincts, regarding which therapies might best bring balance. I have read the Textbook of Functional Medicine (2006), and the Textbook of Natural Medicine (Pizzorno, 1999), and while they do an admirable job of teaching conventional providers how to perform a naturopathic intake, they do not discuss the therapies we have in our toolkits for assisting clients with non-physical issues. The “evidence” is slowly pushing aside our instincts and intuition, the insurance model tempts us to use symptom-based, time-limited practices, and encourages us to believe that if we focus on the physical symptoms, alone, we can achieve health and wellness for ourselves and our patients.
If any conventional physician, after a weekend seminar about supplements, diet and exercise, claims to be an “integrative physician”, it is time to get off that bandwagon. We have fallen a step behind due to our attempts to be recognized as ‘NMDs.’ It is time to realize that acting more like conventional providers is NOT naturopathy, that it is time to reclaim our true name and nature as naturopathic physicians. We promoted integration of mind and body before it was fashionable, and we have left it behind in a misguided attempt to be as “science-based” as conventional physicians.
While many conventional integrative providers give lip service to mind-body ideals, they do not incorporate them well into their symptom-driven practices. ‘Mind-body therapy’ has been handed off to conventional psychologists and therapists; the conceptual divide between mind and body that has been traditionally maintained in conventional practices persists for a great many conventional integrative practitioners. And, unfortunately for our profession, a great many NDs are taking this approach as well.
I believe this divide is the window of opportunity for naturopathy. The mind/body connection, which is unrecognized and disregarded by all conventional, symptom-based care, is the root cause of most illness. It is the need to heal on physical, mental, emotional, spiritual and energetic levels that drives patients out of conventional providers’ offices and into complementary and alternative care. Mental health professionals do not generally attend to body. Conventional medical care does not generally attend to the mind or emotions. The division between mind and body persists, and we are the only primary care providers trained to recognize and manage both. Naturopathy must either embrace its roots and begin to truly and accurately treat the underlying cause of illness, or it will be outcompeted by “integrative” MDs.
Recognition of stress and its impact on our clients’ lives is key to any shift in how we deliver care. An important set of considerations that are unacknowledged in conventional care and that, if left unresolved, can have a negative effect on treatment outcomes, involves somatization of psychological issues,1,2 hidden stressors or unresolved trauma,3,4 and current stressors.5 If we are to truly treat the cause and practice preventively, this area needs to be addressed with every single patient we see, as well as within ourselves.
What is needed is a model of medicine, a model of health, that is supported by the available science in physical, mental, emotional, spiritual and energetic arenas. The model must be flexible enough to admit new evidence for each aspect as it becomes available, inclusive enough to support every modality in use, and simple enough for patients and conventional providers to comprehend. I offer the bare bones of such a model here:
The Model: The Five-Part Harmony Model of Health
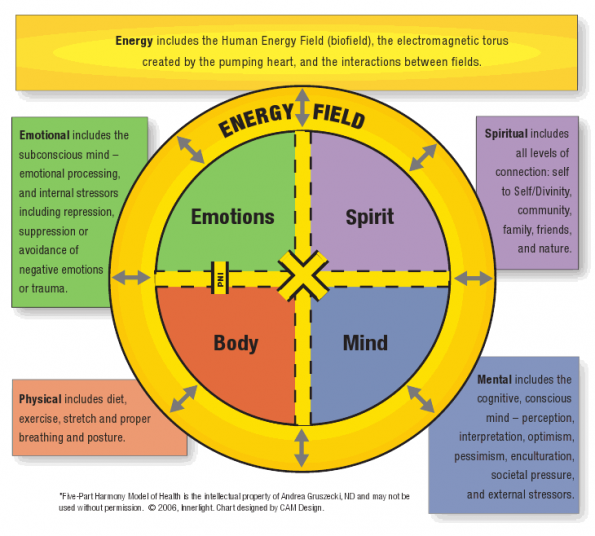
The Five-Part Harmony Model recognizes five main aspects of health, any one of which may become imbalanced and present as a physical symptom. The five aspects are physical, mental (conscious mind), emotional (subconscious mind), spiritual and energy.
The Five-Part Harmony Model of Health6
Physical includes the body and its biochemistry, metabolic functions and genetics, as affected by diet, exercise, stretch and proper breathing and posture.
Mental includes the cognitive, conscious mind – perception, interpretation, optimism, pessimism, enculturation, societal pressure, external environmental stressors.
Emotional includes the subconscious mind – emotional processing, and internal stressors including repression, suppression or avoidance of negative emotions, memories or trauma.
Spiritual includes all levels of connection: self to Self/Divinity, community, family, friends, nature (the Vis).
Energy includes the energy inputs from the environment and the human energy field,7 the electromagnetic torus around the body created by the pumping heart,8 and the interactions between these electromagnetic fields.8
The Science Support
One of the most common problems in mental/emotional/spiritual/energetic therapies is describing how a modality creates changes in the human system. Most conventional providers insist on “evidence-based” complementary modalities, despite the growing evidence that multiple types of evidence exist, which may be appropriate for different levels of review and decision-making.9 As described by Jonas (2001), the “evidence house” model provides room for different types of testing and information gathering. The term “science supported” may be more useful. Adding to the confusion, most complementary /alternative practitioners are quick to insist that their respective modalities cover multiple areas within the Five-Part Harmony model – and they are right – based on current information from the field of psychoneuroimmunology10,11 and the studies of neurocardiology and psychophysiological coherence at the Institute of HeartMath.12 The physical body is impacted by (and may impact) the emotional, mental and energy aspects of the human system. Despite the overlap, all therapies will have a recognizable “entry point” into the model (for example a mindfulness technique will enter the model through the conscious mind, a trauma resolution technique that provides emotional releases enters the model through the emotional subconscious mind, a flower essence will enter the model through energy/vibration).
According to the Merriam-Webster Dictionary,13 psychoneuroimmunology is the study of the interactions between psychological factors, the central nervous system (CNS), and immune function as modulated by the neuroendocrine system. These “molecules of emotion”14 have an impact on the body’s physical systems, including the inflammatory process and immune function. Studies have shown that perceived stress creates neuropeptides in the limbic areas of the brain that are released into the bloodstream, and that these neuropeptides are immune-suppressive and pro-inflammatory.15 This new understanding of the mind-body interaction explains why relaxation, meditation, and stress management demonstrate measurable changes in the physiology of the human system.
An even newer field of research, neurogastroenterology, is offering compelling evidence of the “gut brain” and its effects on the central nervous system. Ninety percent of the fibers in the vagus nerve travel from the gut to the CNS. Ninety-five percent of the tryptophan in the body is found in the tissues of the GI tract. The microbiota are affected by mood, stress and trauma, and, in turn, create effects of their own by secreting neurologically-active peptides and other substances into the bloodstream.4
Research from the Institute of HeartMath further demonstrates that the physical heart’s afferent neural input to the brain has an effect on perception and mood.8 They have further demonstrated that the same electrical information measured in an electrocardiogram creates an electromagnetic field around the body, and that this field is capable of interacting with other human electromagnetic fields.
Put together, this information explains why most of the available research into holistic modalities demonstrates similar positive results in a few basic areas, as listed below, due to mind-body interactions16:
- Relaxation (stress management)
- Improved immune function
- Decreased inflammatory process (asthma)
- Decreased anxiety or depression
- Pain relief
- Reduced fatigue
- Reduction of blood pressure
- Improvements in coronary heart disease or its rehabilitation
- Reduction of salivary cortisol levels
- Improved quality of life
- Reduction in number and severity of headaches
- Changes in gene expression
- Improved type II diabetes or metabolic syndrome
- Relief of medical symptoms17
The improvements are easily explained through the mind-heart-body feedback loops of psychoneuroimmunology and neurocardiology. The overall pattern seems to indicate that most of the positive benefits of holistic care involve mind-body interactions, the notable exceptions being physical-level complementary interventions involving diet, herbs, nutritional supplements, manipulation or exercise (although, even in these arenas, the positive regard and personal attention of the provider may produce mind-body benefits.18 While the energy medicines have not been completely elucidated by science as yet, the available evidence may be reviewed in Energy Medicine the Scientific Basis by James L. Oschman,19 Vibrational Medicine by Richard Gerber, MD,20 The Field by Lynn McTaggart,21 and The Energy Healing Experiments by Schwartz and Simon.22 Information from studies conducted at the HeartMath Institute are available online at: http://www.heartmath.org/faqs/research/research-faqs.html.
Why This Matters in Practice
We must return to our roots and incorporate a model of health for one simple reason: our philosophy of care demands it! If we ignore the mind-body aspect of naturopathic medicine, we fail to treat the cause, we fail to support the Vis, we fail to remove the obstacles to cure, we fail to truly practice wellness and preventative care. We ignore the accumulating evidence at our profession’s peril:
- Women who have been abused are 6 time more prone to substance abuse, 5 times more likely to have family or social problems, 2 times as likely to use tobacco, and are overall more likely to be diagnosed with illnesses ranging from chest pain, depression, anxiety, urinary tract infections, sexually transmitted diseases and GERD, as well as the actual injuries from the abuse.3
- The Child Molestation Research and Prevention Institute estimates that 2/10 girls and 1/10 boys have been sexually abused by the end their 13th year.23
- The Centers for Disease Control and Prevention reports that among people who reported experiencing at least 6 of 8 separate bad childhood experiences – from frequent verbal abuse to living with a mentally ill person – the average age at death was about 61 years, compared to 79 years for people who suffered none of these experiences as children.24
- A national survey reveals that 1 in 10 US children has an alcoholic parent.25 Studies have systematically documented that patients who habitually repress their emotions simultaneously suppress their immune responses; conversely, those who are encouraged to experience and express their feelings demonstrate improvements in immune function, physical condition, and psychological well-being.26
- Research suggests that teaching pre-op patients relaxation, hypnosis, and guided imagery for “shunting blood” during surgery results in 50% less blood loss during spinal surgeries.27 (Blue Cross of CA now covers this type of presurgical psychoeducational training.)
- Low social class in early life has been shown to promote glucocorticoid resistance and upregulated inflammatory responses in the 5th and 6th decades of life.28
- There is an elevated risk of inflammatory disease in individuals who experience chronically high levels of subjective social isolation.29
- Traumatized rat pups show permanent, detrimental changes in their gut microbiomes, and increased GI sensitivity to stress as adult rats.4
- Probiotic treatment of traumatized rat pups normalizes cortisol levels and restores normal GI function in the pups; this is also demonstrated in re-stressed adult trauma survivors.4
- Animal models indicate that stress (sympathetic nervous system activation) encourages bone metastasis in cancer.30
We know that stress and trauma impact health and wellness, but what do we actually do about it? Do we “farm it out” like conventional providers? Or, do we ask the tough questions as we look for signs and symptoms that might be stress or trauma-related, and docere – educate our patients about how such symptoms arise, and teach them how to make the fundamental mental, emotional, Spiritual and energetic changes necessary to live vibrant, healthy lives on all levels? Have we “walked the talk” and made these explorations in ourselves? How do we bring about our patients’ balance if we do not know how to balance ourselves? Focusing 100% of our effort on the physical 20% of the whole person is not the answer. It does not work for conventional providers and it will not work for naturopathic physicians.
We get to choose what kind of profession and what types of providers we wish to be in the 21st century. Let us choose wisely.
Andrea  Gruszecki, ND, a graduate of SCNM (2000), specializes in bringing balance to her patients by supporting their bodies while empowering health on all levels – physical, mental, emotional, Spiritual and energetic. Experiences in conventional medicine as an Army medic and radiographer, combined with her naturopathic training, served her patients well for 12 years. She now enjoys assisting other practitioners working in the Science Support department at Doctor’s Data, Inc.
Gruszecki, ND, a graduate of SCNM (2000), specializes in bringing balance to her patients by supporting their bodies while empowering health on all levels – physical, mental, emotional, Spiritual and energetic. Experiences in conventional medicine as an Army medic and radiographer, combined with her naturopathic training, served her patients well for 12 years. She now enjoys assisting other practitioners working in the Science Support department at Doctor’s Data, Inc.
Anyone wishing more information on how to recognize the symptoms of stress or emotional imbalance is referred to the following websites:
http://www.helpguide.org/mental/mental_emotional_health.htm
http://www.helpguide.org/mental/stress_signs.htm
References
- Feder A. Chapter 3532- Somatization. General Medicine Clinics. http://www.medicineclinic.org/AmbulatorySyllabus4/NEW%20somatization.htm. Accessed March 24, 2012.
- McClendon PD. Trauma-related symptoms/illnesses. Pat McClendon’s Clinical Social Work, 1995. http://www.clinicalsocialwork.com/trauma.html. Accessed March 25, 2012.
- Harding A. Reuters. Abused women suffer more mental, physical ills. October 12, 2009. http://www.reuters.com/article/2009/10/12/us-abused-women-ills-idUSTRE59B4YW20091012. Accessed June 18, 2012.
- Gareau MG, Jury J, MacQueen G, et al. Probiotic treatment of rat pups normalises corticosterone release and ameliorates colonic dysfunction induced by maternal separation. Gut. 2007:56(11):1522-1528. http://www.ncbi.nlm.nih.gov/pubmed/17339238. Accessed November 29, 2012.
- Mayo Clinic. Conversion disorder. February 3, 2011. http://www.mayoclinic.com/print/conversion-disorder/ds00877/dsection=all&method=print. Accessed March 24, 2012.
- Gruszecki AN. Five-Part Harmony, a model of Health for the 21st Century. Lecture series; July, 2011: Fredericksburg, VA.
- Feinstein D. Energy Psychology: A Review of the Preliminary Evidence. Psychotherapy: Theory, Research, Practice, Training. 2008;45(2):199-213. Accessed March 24, 2012.
- McCraty RP. The Energetic Heart, Bioelectricmagnetic Interactions Within and Between People. Institute of HeartMath; 2003:11-12.
- Jonas WB. The evidence house: how to build and inclusive base for complementary medicine. West J Med. 2011;175(2):79-80. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1071485/. Accessed March 30, 2012.
- Azar B. A New Take on Psychoneuroimmunology. American Psychological Association. 2001;32(11):34. http://www.apa.org/monitor/dec01/anewtake.aspx. Accessed March 24, 2012.
- American Psychological Association. (2006, February 23). Stress Weakens the Immune System; February 23, 2006. http://www.apa.org/research/action/immune.aspx. Accessed March 24, 2012.
- McCraty RP. The Appreciative Heart, the Psychophysiology of Positive Emotions and Optimal Functioning. Institute of HeartMath; 2002.
- Merriam-Webster. Psychoneuroimmunology. http://www.merriam-webster.com/dictionary/psychoneuroimmunology. Accessed March 24, 2012.
- Pert C. Molecules of Emotion: The Science Behind Mind-Body Medicine. New York, NY: Simon & Schuster; 1999.
- Lorentz MM. Stress and Psychoneuroimmunology Revisited:Using mind-body interventions to reduce stress. Alt J of Nursing. July, 2006;11. http://www.altjn.com/perspectives/stress.pdf. Accessed March 23, 2012.
- Varvgoli L, Darviri C. Stress Management Techniques: Evidence-based Procedures that Reduce Stress and Promote Health. Health Science Journal. 2011;5(2). http://www.hsj.gr/volume5/issue2/521.pdf. Accessed March 23, 2012.
- Pan CX, Morrison RS, Ness J, et al. Complementary and Alternative Medicine in the Management of Pain, Dsypnea and Nausea and Vomiting Near the End of Life: A Systematic Review. J Pain Symptom Manage: 2000;20(5):374-387. http://www.jpsmjournal.com/article/S0885-3924(00)00190-1/abstract. Accessed March 23, 2012.
- Kaptchuk TJ. The Placebo Effect in Alternative Medicine: Can the Performance of a Healing Ritual Have Clinical Significance? Ann Intern Med. 2002;136(11). http://annals.org/article.aspx?articleid=715317. Accessed March 23, 2012.
- Oschman JL. Energy Medicine: The Scientific Basis. London, England: Churchill Livingstone; 2000.
- Gerber RM. Vibrational Medicine the #1 Handbook of Subtle-Energy Therapies. 3rd ed. Canada: Bear & Company; 2001.
- McTaggart L. The Field: The Quest for the Secret Force of the Universe. New York, NY: Harper Collins; 2008.
- Schwartz GE. The Energy Healing Experiments. New York, NY: Simon & Schuster; 2007.
- Child Molestation Research and Prevention Institute. Early Diagnosis and Effective Treatment. http://www.childmolestationprevention.org/. Accessed December 22, 2012.
- Harding A. Reuters. Stressful childhood may mean earlier death. October 9, 2009. http://www.reuters.com/article/2009/10/09/us-stressful-childhood-idUSTRE5985FV20091009. Accessed December 15, 2102.
- Kelleher JB. One in 10 U.S. kids have alcoholic parent: study. February 16, 2012. www.reuters.com: http://www.reuters.com/article/2012/02/16/us-usa-drinking-study-idUSTRE81F0CB20120216#undefined. Accessed December 15, 2012.
- Selva D. Emotional processing in the treatment of psychosomatic disorders. J Clin Psychol. 2006;62:539-550.
- American Psychological Association. Want Better Health? Use Your Head! December 15, 2003. http://www.apa.org/research/action/head.aspx. Accessed June 18, 2012.
- Miller GE, Chen E, Fok AK, et al. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proc Natl Acad Sci U S A. 2009;106(34):14716-14721. http://www.ncbi.nlm.nih.gov/pubmed/19617551. Accessed December 30, 2012.
- Cole SW, Hawkley LC, Arevalo JM, et al. Social regulation of gene expression in human leukocytes. Genome Biol. 2007;8(9):R189. http://www.ncbi.nlm.nih.gov/pubmed/17854483. Accessed December 30, 2012.
- Campbell JP, Karolak MR, Ma Y, et al. Stimulation of Host Bone Marrow Stromal Cells by Sympathetic Nerves Promotes Breast Cancer Bone Metastasis in Mice. PLoS Biol. 2012;10(7):e1001363. http://www.plosbiology.org/article/info%3Adoi%2F10.1371%2Fjournal.pbio.1001363. Accessed August 12, 2012.

