Craig S. Mehrmann, BSc
The term “meditation” encompasses a broad variety of mental-training practices that vary among cultures and traditions, ranging from techniques designed to promote physical health, relaxation, and improved concentration, to exercises performed with farther-reaching goals, such as developing a heightened sense of well-being, cultivating altruistic behaviors, facilitating evolution of consciousness, and, for some, attaining enlightenment.2 Meditation can be conceptualized as complex emotional and attentional regulatory practices in which mental and somatic events are affected by specific mental-training practices.2 Meditation is typically associated with a concurrent state of heightened, vigilant awareness and reduced metabolic activity,3 allowing for improved physical health,4 psychological balance, and emotional stability.5,6
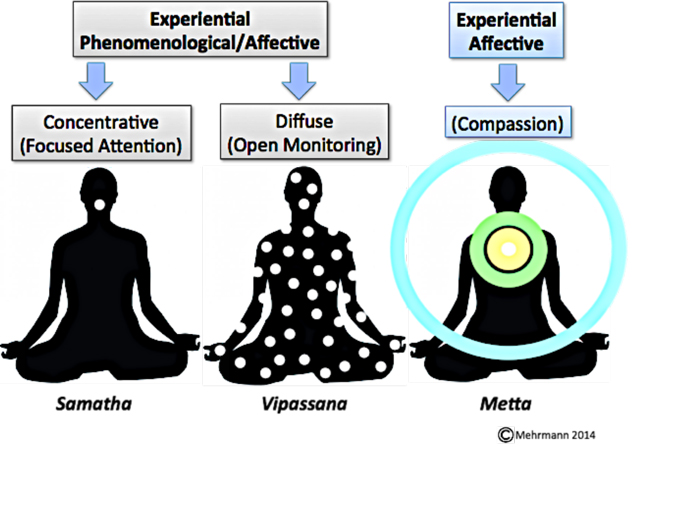
Different types of meditation can be classified based on how the practitioner’s attentional processes are regulated and directed.7 It is therefore important to be explicit about the type of meditation practice under investigation. This article focuses on the 3 most common styles of meditation derived from Buddhist traditions:
- Concentrative, or focused-attention, meditation
- Diffuse, or open-monitoring, meditation
- Compassion meditation, a form of concentration meditation widely practiced in Buddhist traditions
Concentrative and diffuse meditation practices are often combined, whether in a single session or over the course of the practitioner’s training, and are intentionally designed to train specific cognitive processes.7,8 These styles of meditation can be further classified based on whether or not their experiential mode of observation is conditional (experiential affective) or unconditional (experiential phenomenological).
Examples of the 3 most common styles of meditation derived from Buddhist traditions: 1) concentrative, or focused-attention, meditation; 2) diffuse, or open-monitoring, meditation; and 3) compassion meditation. LEFT: EP-focused attention meditation – maintaining concentration on sensations in the area of the philtrum (Pali: Samatha). CENTER: EP/EA diffuse meditation – cultivating awareness of sensations throughout the body while understanding the Three Characteristics (Pali: Vipassana). RIGHT: EP/EA concentration meditation known as “compassion meditation” – cultivating objective awareness of sensation in the area of the non-anatomical heart center, activating an unconditionally positive emotion, and allowing the heart center to act as a receiver-amplifier for that emotion, thereby filling the psychosomatic experience with the vibrations of loving-kindness (Pali: Mettā).
(EP=experiential phenomenological; EA=experiential affective)
Conditional vs Unconditional Modes of Observation
Experiential phenomenological (EP) meditation involves cultivating the ability to observe sensory phenomena impartially, ie, unconditionally, whereas experiential affective (EA) meditation involves some level of interpreting reality, or conditioning reality with the mind. EA can be further classified into 2 subcategories: 1) creating a mind-made sensory phenomenon as an object of concentration, such as a visualization or metaphysical principle (eg, “all sensations are impermanent”); or 2) cultivating awareness of sensory phenomenon, and then filling that awareness with an intention, such as loving-kindness.
EP and EA types of meditation may be practiced exclusively as EP (eg, breath sensations) or EA (eg, visualization), or practiced in combination with one another (EP/EA, eg, awareness of breath sensations while focusing on a visualization). For example, concentration meditation (Pali: samatha) involves maintaining and continually refocusing attention on a chosen object, such as a body sensation, a single point in space, color, object, visualization, sound, or affective state (such as compassion), or with any combination of these objects. Examples of EP concentration meditation include maintaining awareness of the sensations caused by breathing, or maintaining awareness of a visual object that is not created by the mind, such as a candle flame, while examples of EA concentration meditation include maintaining awareness of a visualized object created by the mind, such as a golden orb of light.
Compassion meditation (Pali: mettā) is a form of EP/EA concentration meditation that involves cultivating objective awareness of sensation in the area of the non-anatomical heart center, activating an unconditionally positive emotion, and allowing the heart center to act as a receiver-amplifier for that emotion, thereby filling the psychosomatic experience with the vibrations of loving-kindness. For the purpose of this paper, compassion meditation is considered separately because of its simple practical application, significant derived healing benefit from its practice, and its widespread and distinct emphasis across Buddhist traditions. [A thorough review of the principles, effects, and scientific exploration of compassion meditation as a healing modality is beyond the scope of this paper, but will be covered in depth in a separate article.]
Open-monitoring meditation is an experiential phenomenological form of meditation that involves developing a present-centered and unattached/neutral mode of observation toward all sensory phenomena, including thoughts. Insight meditation (Pali: vipassana) is a form of EP/EA open-monitoring meditation that involves maintaining awareness of certain modes of perception, or metaphysical characteristics, that support the practitioner’s ability to observe sensory phenomena impartially. In Buddhism, significant emphasis is placed on understanding sensory phenomena through the “Three Marks (or Characteristics) of Existence”: 1) impermanence (Pali: anicca), or perpetual transience of all phenomena; 2) no-self (Pali: anatta), or the illusion of a separate and permanent self, or ego; and 3) suffering (Pali: dukkha), or the understanding that one will never ultimately be satisfied by sense objects – hence the term insight meditation, which refers to a form of EP/EA diffuse meditation that is practiced with the continual awareness or experience of these philosophical principles, and with an emphasis on experiencing impermanence, or change (ie, the continual arising and passing of distinct sensory phenomena from moment to moment).6
Mindfulness-based therapeutic programs are all derivatives of traditional Buddhist meditation. The theory and practice of concentrative and diffuse (insight meditation) are at the core of these programs, making these meditation practices the basis for most applications in the clinical and psychiatric settings.1,9,10 Mindfulness-based therapeutic programs have become a popular form of therapeutic intervention: they are efficacious; their principles are universal; they are cost-effective; and they are highly adaptable for diverse populations with different cognitive abilities.8,11 Moreover, these programs have made training in concentration and diffuse meditation more accessible by offering what one may consider a nonreligious alternative for individuals who may be unwilling to adopt Buddhist terminology.6,8
The theory and practice of meditation are not grounded in mysticism or in religious dogma, rites, rituals, or ceremonies, and may rather be accurately described as composing a detailed and precisely descriptive scientific technique. Meditation is universal in nature; meditation methodologies are equally applicable to individuals of any religious, cultural, or spiritual background, and the practice of meditation does not require any form of conversion or identification with a religious tradition. Many Westerners, however, are unfamiliar with the cultural context in which the terminology of Buddhist meditation has developed. This ignorance has, in some cases, resulted in misinterpretations of meditation practices as well as in unwarranted religious or dogmatic stigma being attached to them. To help bridge this cultural boundary, we can consider an introduction to the principles and clinical applications of concentrative and diffuse forms of meditation. We can also review relevant scientific studies to-date on concentrative and diffuse meditation and discuss the clinical implications of these findings. This article describes the philosophical basis and neurophysiological underpinnings of these practices and how they apply to modern healthcare and naturopathic medicine, in particular. Further discussion of scientific research is available for review.6
Concentrative and Diffuse Meditation
Concentrative Meditation
Concentrative meditation is often practiced in preparation for practicing diffuse meditation, and, as noted earlier, entails voluntarily focusing attention on a chosen object in a sustained fashion, such as a visual object, visualized image, sound, breath sensations, or affective state (eg, compassion).7 To sustain this focus, practitioners must constantly monitor and regulate their quality of attention, thereby naturally developing 3 regulatory skills1,6,7:
- monitoring and remaining vigilant to distractions, thereby enabling practitioners to recognize when and to what degree their attention has wandered from the object of focus
- releasing distractions from the attentional field without further involvement
- restoring attention promptly to the chosen object of focus
Concentrative meditation develops the 3 regulative skills to the point that advanced practitioners have an especially acute ability to notice when the mind has wandered, resulting in an automatic and instantaneous restoration of attention on the chosen object of focus.7,12 Eventually, attention rests more readily and stably on the chosen object. As concentration continues to develop, the regulative skills are invoked less and less frequently, and soon the ability to sustain focus becomes “effortless,” a state commonly known as “access concentration.”1,13 The achievement of access concentration is often considered the appropriate time to begin practicing diffuse meditation; however, this relatively high degree of concentration is not absolutely necessary for the beginning stages of diffuse meditation.6
Practitioners continue to practice concentrative or diffuse techniques in everyday life, which enables them to maintain a wholesome lifestyle and contributes to their degree of readily accessible concentrative absorption during formal meditation. The degree of concentrative absorption refers to the depth or strength of concentration on a single-pointed focus and, during formal meditation, correlates directly with how well the continuity of awareness has been maintained since the previous meditation session. For example, practitioners may strive to maintain a continuous awareness of breath sensations or of an affective state such as compassion, or try to maintain a continuous superficial “body-scan” throughout the day. Advanced practitioners report a sense of physical lightness and increased mental and physical vitality as a result of maintaining a concentrated mind.13 This perception may be explained in part by a possible correlation between increased concentration with decreased emotional reactivity, accounting for a more efficient use of energy both during meditation and in everyday life.6,14,15
Diffuse Meditation
Open-monitoring meditation is done with the aim of becoming more objectively aware of sensate experience, which occurs through the development of one’s ability to be psychologically present and equanimous with all forms of sensory phenomena. This state involves the nonreactive monitoring of the ongoing stream of experience from moment to moment, without focusing on any explicit object for a prolonged period of time.16 Practitioners aim to familiarize themselves with reality at the pure sensate level, without interpretation of, or identification with, sensory phenomena. In the context of meditation, sensate refers to anything that can be mentally observed, including thoughts.6
The prelude to diffuse meditation typically involves concentrative meditation to calm and focus the mind, reduce distractions, and enhance one’s equanimity toward sensory phenomena. For example, the practitioner may use concentrative meditation focusing on breath sensations at the area of the philtrum (the indentation below the nostrils and above the upper lip). Continually monitoring breath sensations in the chosen area develops equanimity (or non-reactivity) toward body sensations and enables the practitioner to disengage from, quiet, and eventually stop, the internal dialogue of the mind. From here, the practitioner may shift to diffuse meditation, even if access concentration has not yet been established, so long as the awareness of breath sensations is maintained with relative continuity. The practitioner would then work at continually disengaging from body-mind sensations as quickly as possible until a continual stream of awareness, or access concentration, has been established. Otherwise, as previously described, practitioners would practice concentrative meditation on breath sensations until access concentration has been established, and then redirect their focus from breath sensations to begin practicing diffuse meditation. Usually, practitioners direct their attention to the most subtle (or least perceptible) features of experience possible.6
Open-monitoring meditation enhances one’s faculty of present-centered, nonjudgmental awareness of psychosomatic phenomena, thereby enhancing cognitive flexibility and reappraisal.1 This state is accomplished through nonreactive, metacognitive monitoring of body-mind sensations, which gradually increases awareness of “automatic cognitive and emotional interpretations of sensory, perceptual, and endogenous stimuli.”1,16-18 With consistent practice, the practitioner becomes progressively more aware of subtle body-mind sensations, lending access to rich features of subtle sensational experience, such as emotional tone, active cognitive schema, awareness of sensation all over the body (inside and out), degree of phenomenal intensity, and bodily vibrational frequency (ie, the literal, physical experience of the body and mind as “vibrations,” or rapidly-oscillating particular sensory phenomena whose strength [amplitude] and speed [frequency] fluctuate over time).
The process of cultivating awareness of the psychosomatic experience, while remaining equanimous toward sensory phenomena, disintegrates the gross sensory experience (ie, head, hand, foot, narrative thought, memories) toward progressively more subtle phenomena (subtle flowing vibrations, and eventually space and light); this is often referred to by practitioners as “opening up the body.” This process entails living a lifestyle that supports becoming gradually more aware of the body matrix (ie, more sensitive) in order to disintegrate even very deeply-conditioned interpretative patterns of reality. This lifestyle can be described as living in line with the messages of the body and the world on very subtle levels. The subtlety of the practitioners’ experience is in direct accordance with their concentrative capacity (the degree of effort exerted to observe the subtlest sensations possible while remaining continuously aware of, and equanimous toward, the internal sensory experience).6
Physiological and Neurobiological Studies of Meditation
It is important to acknowledge that the mind and the brain are not the same thing. However, in order to more clearly understand the mechanisms of meditation, it is helpful to understand the physiological and neurobiological analogues of its effects. Buddhist meditation induces what one may consider a low-entropy state of equanimous, vigilant awareness,3 bringing the body to a “hypometabolic state of parasympathetic dominance” that serves to rejuvenate the organism’s capacity for resilience and adaptability.9 Long-term Buddhist meditation has been correlated with reduced stress response and lower cortisol levels overall,4,6 possibly contributing to reduced chronic stress and a restored healthy response to acute stress,4 longevity,6 reduced stress-induced craving, and increased craving tolerance.9 Developed meditators also have the ability to access “highly reinforced” (ie, deep) meditative states,5,7,15 which may contribute to cognitive resilience and adaptation in the face of even highly-agitating stressors.8 Buddhist meditation has been found to increase cerebral plasticity1,12,14,15 and cerebral blood flow, as well as thickening in brain regions associated with the mental exercises practiced by concentrative and diffuse meditation14,15,18; this suggests a potential role for meditation in brain preservation and enhancement.8 This notion is supported by increased proficiency in several cognitive skills associated with consistent concentrative and diffuse meditation, such as the highly-developed ability to disengage from distractors during concentration and the ability to observe one’s internal states in a non-evaluative way.6,8-13,19
Compelling scientific evidence supports the role of meditation in promoting health, in general,4,6,8 and in treating numerous clinical and psychiatric disorders19-27,33,37,38; however, research on how meditation affects neurobiological pathways governing the stress response is lacking overall. Nonetheless, numerous studies have shown that meditation has a normalizing effect on psychobiomarkers of stress regulation and that it produces overall improvements in self-attributed mood scores.1,6,8,11,20-25
Effect on Telomeres
Moreover, the practice of meditation has been shown to positively affect cellular processes that are affected by stress and linked to disease, as is shown by increased telomerase activity with long-term meditation practice.6,55 Telomeres are terminal DNA-protein complexes consisting of repetitive nucleotide sequences that are located at the ends of chromosomes.56 They are known to ensure genomic stability during cellular replication by protecting the ends of chromosomes from deterioration and from fusing with other chromosomes. However, telomeres shorten under conditions of oxidative stress, as well as with each cell-division cycle. Cell division can no longer occur below a critical telomere length, resulting in a state of senescence.6,56,57
Recent longitudinal studies indicate that telomere length in peripheral blood mononuclear cells can increase over time, suggesting that there may be determinable mechanisms – and therefore possible interventions – that regulate the rate of telomere length alteration.55,58-60 Greater perceived stress, negative affect, and stress-related cardiovascular risk are factors associated with lower telomerase activity and telomere shortening.55,61,62 Individuals who respond with suppressed vagal tone when presented with an acute stressor and who show correspondingly increased measures of negative affect and vulnerability to psychological stressors show reduced telomerase activity.6,55,63,64
EEG Coherence
Buddhist meditation has been found to increase EEG coherence through the synchronization of neural discharges, particularly in the gamma-band frequency (25-70 Hz).1,5,7,12 It is theorized that a brainwave’s amplitude is positively correlated with the degree of precision with which cells oscillate and with the size of the neural population through which the wave is occurring.48,49 Increased EEG coherence is correlated with increased brain-processing capacity in areas such as attention, working memory, learning, and conscious perception.49-52 Synchronization of oscillatory neural discharges, particularly of the gamma-band frequency, appears to play a key role in developing the ability to integrate distributed neural processes into 1 overarching network with highly-ordered cognitive and affective functions, suggesting that gamma synchrony may also play a crucial role in meditation-induced neuroplasticity.6,49,53
Reorganization of Brain Activity Patterns
Intrinsic connectivity networks (ICN) are large-scale brain networks that may function either in an active (engaged) or passive (resting) state, suggesting that the human brain is organized into distinct functional networks.34 Significant progress has been made in investigating the effect of consistent meditation practice on systems for sensory processing and integration, revealing 2 temporally distinct neural modes of self- reference: 1) momentary self-reference centered on the present moment (experiential focus), neurologically correlated with the central executive network; and 2) extended self-reference linking subjective experience across time (narrative focus), neurologically correlated with the default mode network.15,34,35 Another related ICN of importance to overall health and mental well-being is the salience network, associated with resilience and perseverance in the face of stress.6
The default mode network comprises an integrated system for autobiographical, self-centered, and social cognitive functions characterized by ruminative, often subconscious, self-referential narrative thought linking subjective experience across time – which generates one’s concept of self or identity.36 The default mode network concept emerged from a body of evidence demonstrating a consistent pattern of deactivation across a distributed network of brain regions during focused mental tasks; these regions become activated in the absence of such focused mental tasks.36 Conversely, the central executive network is activated (and default mode network deactivated) during focused mental tasks.34,35 There is a third ICN, known as the salience network, acting as a sort of frequency modulator between the activation of the central executive network in the face of cognitively demanding tasks, and the simultaneous deactivation of default mode network.6,34
Recent findings have shown that a gradual, meditation-induced, functional reorganization of brain activity patterns occurs between the default mode network, salience network, and central executive network, where reliance upon the central executive network and salience network seems to increase, and reliance upon the default mode network seems to decrease.34,35 Abnormal activity in this intrinsic connectivity network has been implicated in a number of psychiatric diseases (eg, ADHD, bipolar disorder, borderline personality disorder, depression and anxiety disorders, and schizophrenia).34,35,37 Furthermore, an inability to “switch-off” the hyperactive default mode network through focusing the mind appears to be a major contributor to the disease process,37 suggesting that meditation may aid in reducing symptoms in these disorders.6
Discussion
Allopathic medicine has progressed by way of hypothetical deduction, relying heavily upon pharmaceuticals and technology-based interventions to treat or suppress diseases caused by pathophysiologic processes. While these have had a substantial impact in preserving human health globally, the effectiveness of allopathic medicine remains limited, especially when treating chronic disease and mental illness in which lifestyle, stress, and the environment play major roles.65 Moreover, while naturopathic medicine has made significant strides in treating the body holistically, the field of mind-body medicine still remains quite limited in the naturopathic medical model. Understanding the mechanisms of mental habit pattern formation, as well as familiarity with tools for developing cognitive flexibility and reprisal, are fundamental to facilitating the healing process and aiding patients in making lifestyle changes. Cultivating the capacity to remain deeply unattached to sensory phenomena, including thoughts and emotions, is perhaps one of the most profoundly effective tools for allowing the Vis to move freely toward healing. The continued study and integration of Eastern healing techniques may bring about a complementary model that will contribute to a more systematically comprehensive and holistic approach to patient care overall, particularly in the area of mind-body medicine.
Future Research
The skills developed through meditation practice have significant implications for the treatment of various clinical and psychiatric disorders. The neural correlates of these skills may be partially explained by mechanisms involved in neuroplasticity over the lifespan. These findings also support the notion that concentrative and diffuse meditation practices aid in behavior modification, in attenuating stress-related illness, and in slowing – and perhaps stopping and rehabilitating – neurodegeneration and cognitive decline.7 Future meditation research should aid in developing a clearer understanding of how large-scale brain network organization in the human brain produces cognition. Recent evidence suggests that cognitive function depends on a dynamic interaction of dissociable large-scale brain networks, such as the recently discovered intrinsic connectivity networks.1,34-36 Determining dissociable large-scale brain networks and their cognitive and behavioral correlates in healthy individuals would aid in studying psychiatric diseases by providing a reference point for comparison. Developed meditators may provide researchers with a more objective point of reference for healthy brain function than what may be found in the general population.6
Neuroscientists and physiologists have made strides in elucidating some of the basic biological mechanisms underlying the benefits of meditation. Our understanding, however, is rudimentary at this stage. Continued research in the field of neurometacognition may eventually enable the formulation of a coherent theoretical framework for the neurobiology of consciousness.1,2,6,7,14,16, 31-35 Meditation research can provide a framework for study that will help correlate electrophysiological recordings with simultaneously-activated brain areas and their associated cognitive and behavioral analogues. Buddhist practitioners and literature provide meditation instructions within a comprehensive theoretical framework of the states of consciousness that may be experienced through meditation, which may prove useful in guiding and expediting the investigation.30,39,40,66-68 Moreover, this process may provide a strong and invaluable unification of 2 diametrically opposed methodologies used for the scientific investigation of consciousness – namely, the intellectual and deductive approach taken by Western scientists, and the experiential and inductive approach taken by the Eastern spiritual practitioners.6
The neurological and physiological correlates of specific practices differ significantly between populations, such as the differences one may find among monks, laypersons, adults, children, and individuals with psychopathology. Researchers must be specific about the style of meditation practice and the population under investigation, or else risk causing experimental confounds that produce results with limited or no potential for broader scientific comparison or application. Longitudinal studies on Buddhist meditation are lacking overall and would be of great use in determining neural development and reorganization with meditation experience and in verifying behavioral, experiential, and physiological modifications over time in relation to constant information (eg, Buddhist texts). Longitudinal studies would also aid in separating out the specific neurological/behavioral factors affected by meditation, itself, from those found across individuals who are already likely to practice meditation.6
A Role for Buddhist Theory
The aspects of Buddhist theory that have been scientifically investigated thus far have served mainstream psychology and cognitive neuroscience well, making Buddhist theory a potential avenue for in-depth and critical scientific investigation. Such investigations may provide a useful and arguably necessary broadening of perspective with regard to defining and treating psychopathology. It has been suggested that the mechanisms underlying psychiatric symptom reduction occur at a level of “personality reorganization,” because almost all of the commonly defined personality types – healthy, neurotic, borderline, psychotic, and so on – can be recognized in terms of personality development and organization over time.69 Therefore, in the context of meditation in the clinical setting, it may be useful to think of mental illness in terms of a symptomatic continuum, from most to least pathological, with the aim of progressively reducing symptoms through shifting the mind and body toward a holistic state of natural balance.6,69
The Western scientific study of meditation has, in large part, been conducted with minimal reference to its religious and spiritual origins, and only a brief overview of the most fundamental and commonly practiced forms of Buddhist meditation has been presented here. However, Buddhism has been successful in maintaining the practice and teaching of insight meditation for over 2500 years, and an extensive and detailed literature is devoted to theoretical aspects of the stages of meditative experience, or the “process of insight.”39,66-69 Investigation of these texts reveals a theoretical science with corresponding technical meditation instructions that guide the practitioner, in a stepwise manner, through a process of coming out of suffering (or attachment to ego) by gradually deepening his or her knowledge of experiential reality. In short, this process involves a gradual cumulative development of specific faculties of awareness that the individual uses to literally heal his or her own body while maximizing awareness and equanimity toward sensory experience and creating space for the integration of new information.
A detailed synopsis of this process and its implications is beyond the scope of this article. However, future articles will provide a more in-depth analysis of the healing process allowed by meditation via the Vis and how this process allows the body to function more optimally throughout the lifespan. In the interim, a wide body of literature is available for readers who are interested in further exploration.6,39,66-70
Acknowledgements: Sussanna Czeranko, ND, was the acting supervisor for this Student Writer’s Scholarship article. While she did not coauthor the article, she did provide approval of its validity, as well as supportive encouragement.
 Craig S. Mehrmann, BSc, is currently in his second year at NCNM, earning doctoral degrees in naturopathic and classical Chinese medicine. He studied neuroscience and philosophy at the University of Massachusetts Amherst, where he received scholarships to conduct research on memory formation and the neurobiology of stress and disease. After graduating, he spent 3 years working as a psychiatric counselor in acute and non-acute settings while maintaining an intensive meditation practice in the United States and Burma and conducting research as an affiliate of Massachusetts General Hospital and Harvard Medical School on the neurobiology of insight meditation and its applications in the psychiatric setting. His present research is focused on refining and integrating the contextual understanding of mind-body medicine, and on applying traditional human developmental models to modern holistic healthcare systems. His special interests in medicine lie in mind-body medicine, as well as psychiatric and pediatric healthcare. Mr Mehrmann is President-elect of NMSA International.
Craig S. Mehrmann, BSc, is currently in his second year at NCNM, earning doctoral degrees in naturopathic and classical Chinese medicine. He studied neuroscience and philosophy at the University of Massachusetts Amherst, where he received scholarships to conduct research on memory formation and the neurobiology of stress and disease. After graduating, he spent 3 years working as a psychiatric counselor in acute and non-acute settings while maintaining an intensive meditation practice in the United States and Burma and conducting research as an affiliate of Massachusetts General Hospital and Harvard Medical School on the neurobiology of insight meditation and its applications in the psychiatric setting. His present research is focused on refining and integrating the contextual understanding of mind-body medicine, and on applying traditional human developmental models to modern holistic healthcare systems. His special interests in medicine lie in mind-body medicine, as well as psychiatric and pediatric healthcare. Mr Mehrmann is President-elect of NMSA International.
References:
- Slagter HA, Davidson RJ, Lutz A. Mental training as a tool in the neuroscientific study of brain and cognitive plasticity. Front Hum Neurosci. 2011;5:17.
- Raffone A, Srinivasan N. The exploration of meditation in the neuroscience of attention and consciousness. Cogn Process. 2010;11(1):1-7.
- Young JD, Taylor E. Meditation as a voluntary hypometabolic state of biological estivation. News Physiol Sci. 1998;13:149-153.
- Sudsuang R, Chantanez V, Veluvan K. Effects of Buddhist meditation on serum cortisol and total protein levels, blood pressure, pulse rate, lung volume and reaction time. Physiol Behav. 1991;50(3):543-548.
- Lutz A, Brefczynski-Lewis J, Johnstone T, Davidson RJ. Regulation of the neural circuitry of emotion by compassion meditation: effects of meditative expertise. PLoS One. 2008;3(3):e1897.
- Mehrmann C, Karmacharya R. Principles and neurobiological correlates of concentration, diffuse, and insight meditation. Harv Rev Psychiatry. 2013;21(4):205-218.
- Lutz A, Dunne JD, Davidson RJ. Meditation and the neuroscience of consciousness: an introduction. In: Zelazo P, Moscovitch M, Thompson E, eds. The Cambridge Handbook of Consciousness. New York, NY: Cambridge University Press; 2007:81-109.
- Dakwar E, Levin FR. The emerging role of meditation in addressing psychiatric illness, with a focus on substance use disorders. Harv Rev Psychiatry. 2009;17(4):254-267.
- Gunaratana B. Mindfulness in Plain English. Somerville, MA: Wisdom Publications; 2007.
- Kabat-Zinn J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin Psychol Sci Pract. 2003;10:144-153. Available at: http://www-psych.stanford.edu/~pgoldin/Buddhism/MBSR2003_Kabat-Zinn.pdf. Accessed November 15, 2014.
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350-1352.
- Cahn BR, Polich J. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol Bull. 2006;132(2):180-211.
- Goleman D. The Buddha on meditation and states of consciousness. In: Shapiro DH Jr, Valsh RN, eds. Meditation, Classic and Contemporary Perspectives. Piscataway, NJ: Aldine Transaction; 2008:345-347.
- Brefczynski-Lewis JA, Lutz A, Schaefer HS, et al. Neural correlates of attentional expertise in long-term meditation practitioners. Proc Natl Acad Sci U S A. 2007;104(27):11483-11488.
- Farb NAS, Segal ZV, Mayberg H, et al. Attending to the present: meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci. 2007;2(4):313-322.
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci. 2008;12(4):163-169.
- Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11(3):230-241. Available at: http://www.mbcttrainingen.nl/Resources/Mindfulness%20Definition.pdf. Accessed November 15, 2014.
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: an integrative review. Clin Psychol Rev. 2009;29(6):560-572.
- Hayes SC, Jacobson NS, Follette VM, Dougher MJ, eds. Acceptance and Change: Content and Context in Psychotherapy. Reno, NV: Context Press; 1994.
- Marlatt GA, Witkiewitz K, Dillworth TM, et al. Vipassana meditation as a treatment for alcohol and drug use disorders. In: Hayes SC, Follette VM, Linehan MM, eds. Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition. New York, NY: The Guilford Press; 2004: 261-287.
- Teasdale JD, Segal ZV, Williams JM, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615-623.
- Wolf DB, Abell N. Examining the effects of meditation techniques on psychosocial functioning. Res Soc Work Pract. 2003;13(1):27-42.
- Shannahoff-Khalsa DS. Kundalini Yoga meditation techniques for the treatment of obsessive-compulsive and OC spectrum disorders. Brief Treat Crisis Interv. 2003;3:369-382. Available at: http://btci.stanford.clockss.org/cgi/reprint/3/3/369. Accessed November 15, 2014.
- Marlatt GA, Marques JK. Meditation, self-control and alcohol use. In: Stuart RB, ed. Behavioral Self-Management: Strategies, Techniques and Outcome. New York, NY: Brunner/Mazel; 1977:117-153.
- Linehan MM, Comtois KA, Murray AM, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757-766.
- Fjorback LO, Walch H. Meditation based therapies—a systematic review and some clinical observations. Religions. 2012;3(1):1-18.
- Kabat-Zinn J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life. New York, NY: Hyperion; 1994.
- Teasdale JD, Segal Z, Williams JM. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness training) help? Behav Res Ther. 1995;33(1):25-39.
- Kristeller JL, Hallett CB. An exploratory study of meditation-based intervention for binge eating disorder. J Health Psychol. 1999;4(3):357-363.
- Kornfield J. A Path with Heart: A Guide Through the Perils and Promises of Spiritual Life. New York, NY: Bantam; 1993.
- Gilbert P, ed. Compassion: Conceptualizations, Research and Use in Psychotherapy. New York, NY: Routledge; 2006.
- Henry WP, Schacht TE, Strupp HH. Patient and therapist introject, interpersonal process, and differential psychotherapy outcome. J Consult Clin Psychol. 1990;58(6):768-774.
- Rubia K. The neurobiology of meditation and its clinical effectiveness in psychiatric disorders. Biol Psychol. 2009;82(1):1-11.
- Bressler SL, Menon V. Large-scale brain networks in cognition: emerging methods and principles. Trends Cogn Sci. 2010;14(6):277-290.
- Manna A, Raffone A, Perrucci MG, et al. Neural correlates of focused attention and cognitive monitoring in meditation. Brain Res Bull. 2010;82(1-2):46-56.
- Raichle ME, MacLeod AM, Snyder AZ, et al. A default mode of brain function. Proc Natl Acad Sci U S A. 2001;98(2):676-682.
- Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49-76.
- Daniels JK, McFarlane AC, Bluhm RL, et al. Switching between executive and default mode networks in post traumatic stress disorder: alteration in functional connectivity. J Psychiatry Neurosci. 2010;35(4):258-266.
- Goenka SN. Mahasatipatthana Sutta: The Great Discourse on Establishing Awareness. Seattle, WA: Vipassana Research Institute; 1996.
- Hanh TN. The Miracle of Mindfulness: A Manual of Meditation. Boston, MA: Beacon Press; 1976.
- Dietrich A. Functional neuroanatomy of altered states of consciousness: the transient hypofrontality hypothesis. Conscious Cogn. 2003;12(2):231-256.
- Lou HC, Norwak M, Kjaer TW. The mental self. Prog Brain Res. 2005;150:197-204.
- Luders E, Kurth F, Mayer EA, et al. The unique brain anatomy of meditation practitioners: alterations in cortical gyrification. Front Hum Neurosci. 2012;6:34.
- Lazar SW, Kerr CE, Wasserman RH, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16(17):1983-1987.
- Holzel BK, Ott U, Gard T, et al. Investigation of mindfulness meditation practitioners with voxel-based morphometry. Soc Cogn Affect Neurosci. 2008;3(1):55-61.
- Luders E, Toga A, Lepore N, Gaser C. The underlying anatomical correlates of long-term meditation: larger hippocampal and frontal volumes of grey matter. Neuroimage. 2009;45(3):672-678.
- Grant JA, Courtemanche J, Duerden EG, et al. Cortical thickness and pain sensitivity in zen meditators. Emotion. 2010;10(1):43-53.
- Niedermeyer E, da Silva FL. Electroencephalography: Basic Principles, Clinical Applications, and Related Fields. New York, NY: Lippincott Williams & Wilkins; 2004.
- Lutz A, Greischar LL, Rawlings NB, et al. Long-term meditators self-induce high-amplitude gamma synchrony during mental practice. Proc Natl Acad Sci U S A. 2004;101(46):16369-16373.
- Sheppard WD. Pretrial EEG coherence as a predictor of semantic processing effects in a lexical decision test. Dissertation Abstr Int. 1998;49:B3610.
- Sheppard WD 2nd, Boyer RW. Pretrial EEG coherence as a predictor of semantic priming effects. Brain Lang. 1990;39(1):57-68.
- Cardin JA, Carlen M, Meletis K, et al. Driving fast-spiking cells induces gamma rhythm and control sensory responses. Nature. 2009:459(7247):663-667.
- Baldeweg T, Spence S, Hirsch SR, Gruzelier J. Gamma-band electroencephalographic oscillations in a patient with somatic hallucinations. Lancet. 1998;352(9128):620-621.
- Lama D, Cutler HC. The Art of Happiness, 10th Anniversary Edition: A Handbook for Living. New York, NY: Riverhead; 2009.
- Jacobs TL, Epel ES, Lin J, et al. Intensive meditation training, immune cell telomerase activity, and psychological meditators. Psychoneuroendocrinology. 2011;36(5):664-681.
- Blackburn EH. Structure and function of telomeres. Nature. 1991;350(6319):569-573.
- Fossel M. Role of cell senescence in human aging. J Anti Aging Med. 2000;3(1):91-98.
- Epel ES, Merkin SS, Cawthon R, et al. The rate of leukocyte telomere shortening predicts mortality from cardiovascular disease in elderly men. Aging (Albany, NY). 2008;1(1):81-88.
- Nordfjall K, Svenson U, Norrback KF, et al. The individual blood cell telomere attrition rate is telomere length dependent. PLoS Genet. 2009;5(2):e1000375.
- Farzaneh-Far R, Lin J, Epel E, et al. Telomere length trajectory and its determinants in persons with coronary artery disease: longitudinal findings from the heart and soul study. PLoS One. 2010;5(1):e8612.
- Epel ES, Blackburn EH, Lin J, et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A. 2004;101(49):17312-17315.
- Epel ES, Lin J, Wilhelm FH, et al. Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinology. 2006;31(3):277-287.
- Porges SW. Cardiac vagal tone: a physiological index of stress. Neurosci Biobehav Rev. 1995;19(2):225-233.
- Carney RM, Blumenthal JA, Stein PK. Depression, heart rate variability, and acute myocardial infarction. Circulation. 2001;104(17):2024-2028.
- National Institute of Mental Health. Available at: http://www.nimh.nih.gov/statistics/index.shtml. Accessed November 15, 2014.
- Buddhaghosa B, Nyanamoli B, trans. The Path of pPurification: Visuddhimagga. Kandy, Sri Lanka: Buddhist Publication Society; 1991.
- Bhikkhu P. Vimuttidhamma: From Chakra to Dhammachakra. Thailand: Dhamma Publication Fund; 2011.
- Ingram DM. Mastering the Core Teachings of the Buddha: An Unusually Hardcore Dhamma Book. London, England: Aeon Books; 2008.
- Wilber K, Engler J, Brown DP. Transformations of Consciousness: Conventional and Contemplative Perspectives on Development. Boston, MA: Shambala; 1986.
- Vago DR, Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front Hum Neurosci. 2012;6:296.