Holly Lucille, ND, RN
In conventional practices, NSAIDs and glucocorticoids are used the most frequently for RA treatment, but they also bring with them a host of side effects, especially in long-term use. Possible adverse effects include stomach and liver damage, allergic reactions, lowered immunity, increased blood pressure, lowered red blood cell activity (myelosuppression), and increased risk of osteoporosis.1,2 Worse yet, even though they help control pain and inflammation, they really only cover the problem for a while. Beyond stopping some of the inflammation, they still can’t stop the joint damage of RA, or lower attendant depression, or address other chronic conditions that can easily present alongside RA. So, aside from some temporary relief, they are essentially “one-note” forms of treatment.I think one of the most difficult things for any practitioner is treating chronic conditions that have left a patient feeling frustrated, helpless, and at the mercy of synthetic drugs that can bring a wake of terrible side effects. As an autoimmune disease, rheumatoid arthritis (RA) falls into a category of illness that is typically difficult to treat conventionally beyond symptom control and – if caught early enough – a slowdown in joint destruction.
The fact that these measures cannot actually stop RA is the difficult part. As any practitioner knows, RA doesn’t just make people feel bad. Left untreated, or improperly treated, it can destroy a life. In especially difficult cases, untreated RA patients may see permanent disability in as little as 3 years following a diagnosis.1,3
This presents a real challenge for natural practitioners, and I think we can do better. Timing is critical: according to a 2011 study published in Clinical Rheumatology,3 the earlier the intervention, the better; however, about 30% of those with the most severe forms of the disease don’t respond to conventional treatments at all.1
Exactly why the body tricks itself into fighting its own tissues in RA is still not proven, though there are strong indications that intestinal permeability (“leaky gut”) plays a powerful role in the development of this disease.4 In a healthy system, the body achieves a homeostasis with regards to the immune system; it runs at a pleasantly “lukewarm” temperature, so to speak. That’s as it should be – just enough to keep viruses and other threats at bay, but not to be on overdrive. Of course, that’s the very problem with RA. The balance is completely off, and the body’s own defenses spin out of control against itself.5
Curcumin to the Rescue
Fortunately, there is hope for healing without complications. It is a compound from an herbal source known to practitioners of traditional Indian and Chinese medicine for generations: curcumin from turmeric (Curcuma longa).
Without a doubt, curcumin is well known to practitioners here in the United States too. And certainly, I’m sure that more than a few reading this column have used it for fighting pain. But I believe that it could be a complete RA-fighting herbal powerhouse unto itself.
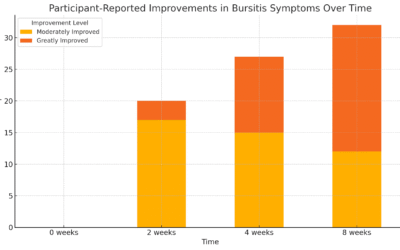
Consider this study, published in Phytotherapy Research. In this randomized 8-week study, 45 participants were randomized to 3 groups.1 All of them had been diagnosed with RA, functional class I or II. Group 1 received diclofenac sodium, 50 mg BID; group 2 received 500 mg BID of an enhanced-absorption curcumin that also contains turmerones from turmeric essential oil; and group 3 received both diclofenac sodium and the curcumin. In both curcumin groups, there were no drop-outs due to adverse effects; however, in the diclofenac sodium-only group, 14% withdrew due to adverse effects.1
Before and after participation, a full check of kidney and liver function, blood sugar, and a complete blood count were performed. There were no significant changes in these measurements, in general, in all of the groups. One laboratory analysis adverse event was reported in the drug (diclofenac sodium) group.1
In the Disease Activity Score-28 (DAS28) assessment, the curcumin-only group showed the best results for disease symptom reduction, followed by the combination therapy of curcumin with diclofenac sodium. Interestingly, the diclofenac sodium-only group scored in last place. So, was curcumin the heavy-lifter here? After all, it was more effective than diclofenac sodium at reducing joint pain and swelling. Taking the curcumin with the drug was no more effective than using the botanical alone, and taking the drug alone was the least effective.1
Aside from those direct symptom changes, the curcumin-only group also showed improvement over others in reducing C-reactive protein (CRP), a measure of chronic inflammation, as well as anti-streptococcal antibodies (ASO) titers, which correlate with severity of RA activity.1
Diclofenac is one of the most commonly prescribed conventional drugs on the planet. Diclofenac sodium is widely used for RA treatment,6 so it was an easy choice for comparison’s sake. And, to be certain, I’d love to see more clinical comparisons regarding curcumin, prescription drugs, and RA. But this is still very impressive.
Curcumin & Depression
Now, if the idea of recommending curcumin for RA was only about promoting safe pain relief and stopping joint destruction (as if that isn’t enough), this compound can also relieve one of the worst aspects of RA: depression.
According to the Centers for Disease Control & Prevention (CDC), there is a “high prevalence of anxiety and depression… documented in several clinical populations of people with RA.”7 They also mention that the presence of anxiety and depression often means that people tend to not adhere to their prescribed course of treatments. The benefit of finding a natural therapy for RA and depression seems like a perfect fit for any practitioner. Here too, curcumin shows its versatility.
In a clinical study, patients with major depressive disorder (MDD) showed the greatest response using a combination of fluoxetine and high-absorption curcumin enhanced with turmeric essential oil – a 77.8% response rate, as measured by the Hamilton Depression Rating Scale (HAMD-17).8
What I find interesting is that the single-therapy groups’ scores were virtually identical: fluoxetine at 64.7%, and curcumin at 62.5%. Ie, curcumin essentially worked as well as the prescription drug, fluoxetine, in terms of the measurable changes in the HAMD-17 score from baseline to 6 weeks of treatment, but without side effects.8
In another placebo-controlled study, high-absorption curcumin enhanced with turmeric essential oil showed antidepressant effects in people with MDD 4-8 weeks after treatment.9 Related research found that 500 mg BID of curcumin influenced biomarkers that appear to be associated with depression, including leptin and endothelin-1, and reduced their effects over an 8-wk period.10
Mechanisms of Action
How can curcumin do so much to impact multiple conditions? The answer is that it works along many pathways, whereas synthetic drugs typically work along only 1. Instead of fighting on a narrow front (and incurring side effects along the way), curcumin works widely and deeply to:
- Suppress the activation of nuclear factor-kappa B (NF-ĸB), which regulates the expression of pro-inflammatory gene products
- Downregulate cyclooxygenase-2 (COX-2), the enzyme linked to most inflammation
- Downregulate the expression of cell-surface adhesion molecules linked to inflammation
- Inhibit the activity of pro-inflammatory tumor necrosis factor-alpha (TNF-α)5
Additionally, a Japanese cultured-cell study found that curcumin inhibits histone acetyltransferase, which ultimately helps lower the activity of interleukin (IL)-6, an inflammatory cytokine and causal factor in RA (IL-6 is seen in higher levels in the synovial fibroblasts of RA).11
So, curcumin has plenty of mechanisms of action to support its use. And, in an easily absorbable form, you won’t have to worry about side effects or dosage levels that are too challenging for patient compliance.
Using Curcumin in Clinical Practice
Curcumin also shows remarkable potential to relieve inflammatory bowel disease, making it a perfect agent for countering conditions leading to leaky gut syndrome. In a small clinical study, patients with ulcerative proctitis and Crohn’s disease received daily curcumin.12 The patients with ulcerative proctitis were also taking prescription medications; however, by the end of the 2-month study period, 2 participants were able to stop taking 1 of their prescriptions altogether (including prednisone), and 2 others reduced their dosages. Inflammation levels returned to normal as well. Patients with Crohn’s disease who completed the study (4 out of 5) showed significant improvement, including less frequent bowel movements, less pain and cramping, and better-formed stools.12
The curcumin used in the RA and depression studies was naturally enhanced with turmeric essential oils to boost absorption beyond that of standard 95% extracts, which can necessitate high dosages and cause gastric discomfort. This blending with turmeric oils seems to extend curcumin’s retention time in the plasma, and at significant levels.13 In practical terms, this means that whether recommending for RA or attendant depression, the dosage could be as little as 1000 mg daily in 2 divided doses – definitely an easy level for patient compliance.1,8,9,10
When people suffering from RA first come to my office, they feel frustrated and adrift because they feel powerless over the pain and soreness of the disease. Curcumin’s potential as part of a natural treatment plan for RA is astounding. Numbers from the CDC show that there are 1.5 million Americans with RA,8 so we have our work cut out for us. But having curcumin in our corner makes the fight much easier to win.
 Holly Lucille, ND, RN (“Dr. Holly”), is a nationally recognized licensed naturopathic physician, author, educator, and consultant. She is a graduate of the Southwest College of Naturopathic Medicine in Tempe, AZ, where she received the prestigious Daphne Blayden Award. Dr Holly has a private practice in Los Angeles (Healing from Within Healthcare) and volunteers at the LA Free Clinic. She lectures throughout the nation, has appeared on national media programs, and is the author of Creating and Maintaining Balance: A Women’s Guide to Safe, Natural, Hormone Health.
Holly Lucille, ND, RN (“Dr. Holly”), is a nationally recognized licensed naturopathic physician, author, educator, and consultant. She is a graduate of the Southwest College of Naturopathic Medicine in Tempe, AZ, where she received the prestigious Daphne Blayden Award. Dr Holly has a private practice in Los Angeles (Healing from Within Healthcare) and volunteers at the LA Free Clinic. She lectures throughout the nation, has appeared on national media programs, and is the author of Creating and Maintaining Balance: A Women’s Guide to Safe, Natural, Hormone Health.
References
- Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res. 2012;26(11):1719-1725.
- McGettigan P, Henry D. Use of non-steroidal anti-inflammatory drugs that elevate cardiovascular risk: an examination of sales and essential medicines lists in low-, middle-, and high-income countries. PLoS Med. 2013;10(2):e1001388
- Rindfleisch JA, Muller D. Diagnosis and management of rheumatoid arthritis. Am Fam Physician. 2005;72(6):1037-1047.
- Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78.
- Jantan I, Ahmad W, Bukhari SN. Plant-derived immunomodulators: an insight on their preclinical evaluation and clinical trials. Front Plant Sci. 2015;6:655.
- Altman R, Bosch B, Brune K, et al. Advances in NSAID development: evolution of diclofenac products using pharmaceutical technology. Drugs. 2015;75(8):859-877.
- Centers for Disease Control & Prevention. Rheumatoid Arthritis. Updated October 28, 2015. CDC Web site. http://www.cdc.gov/arthritis/basics/rheumatoid.htm. Accessed December 1, 2015.
- Sanmukhani J, Satodia V, Trivedi J, et al. Efficacy and safety of curcumin in major depressive disorder: a randomized controlled trial. Phytother Res. 2014;28(4):579-585.
- Lopresti AL, Maes M, Maker GL, et al. Curcumin for the treatment of major depression: a randomised, double-blind, placebo controlled study. J Affect Disord. 2014;167:368-375.
- Lopresti AL, Maes M, Meddens MJ, et al. Curcumin and major depression: A randomized, double-blind, placebo-controlled trial investigating the potential of peripheral biomarkers to predict treatment response and antidepressant mechanisms of change. Eur Neuropsychopharmacol. 2015;25(1):38-50.
- Wada TT, Araki Y, Sato K, et al. Aberrant histone acetylation contributes to elevated interleukin-6 production in rheumatoid arthritis synovial fibroblasts. Biochem Biophys Res Commun. 2014;444(4):682-686.
- Holt PR, Katz S, Kirshoff R. Curcumin therapy in inflammatory bowel disease: a pilot study. Dig Dis Sci. 2005;50(11):2191-2193.
- Antony B, Merina B, Iyer VS, et al. A Pilot Cross-Over Study to Evaluate Human Oral Bioavailability of BCM-95CG (Biocurcumax), A Novel Bioenhanced Preparation of Curcumin. Ind J Pharm Sci. 2008;70(4):445-449.