David M. Brady, ND, DC, CCN, DACBN
This article is one in a series of Clinical Rounds that has been appearing periodically in NDNR. Real case studies from Dr. Brady’s practice are presented. It is his aim to present interesting cases that will facilitate thought and discussion about novel diagnostic and therapeutic techniques for myriad clinical conditions likely to appear in other ND offices.
Patient Presentation and History
A 42-year-old female presented to my practice with the following:
- Fatigue
- Mercury toxicity concern
- Possible candida infection
- Excessive sweating in palms, axillary area and groin
- History of low RBC and WBC count
- History of low cholesterol
- Irregular menses.
The patient was concerned because recent routine laboratory work ordered by her physician indicated that her RBC, WBC and cholesterol were significantly low. She had been suffering from intermittent bouts of fatigue, which she thought were seasonally related; her menstrual cycle had become irregular over the past few years; and she had a long-standing issue with excessive perspiration in the palms, axillary area and groin. Candida infections had also been an occasional problem, and the patient had a previous elevation in her candida IgG antibodies on lab work performed one year before her presentation to my office. The patient brought a salivary cortisol and DHEA test performed during the year previous to presentation, which revealed an elevated noon and depressed afternoon cortisol and low DHEA. She was concerned about suffering from adrenal dysfunction. The patient had several hair analyses performed over a period of eight years, which revealed elevated levels of mercury. She supplemented herself occasionally with selenium in an attempt to chelate the mercury.
Lifestyle and Social Issues
The patient was a nutritionist and fitness consultant by profession. She engaged in proper amounts of exercise with aerobics, lightweight training and sit-ups. She also enjoyed yoga regularly. She admitted to not getting enough sleep, usually retiring at about midnight and rising near 6:30 a.m. Most of her lack of sleep was due to the busy schedule of a professional woman with a husband and two children. She was happy in her relationship with her husband and felt she had a good relationship with her children. Her eating habits were exceptional, with a strong emphasis on a macronutrient-balanced, whole, fresh and organic food diet. She also regularly took a comprehensive basic supplement program, including a quality multi-vitamin mineral, as well as omega-3-fatty acids, mixed tocopherol, Ca/Mg, B-complex, zinc, chromium and selenium.
Physical Examination
The patient’s vitals were normal, with the exception of a slightly low oral temperature of 97.6. EENT examination was normal, with the exception of the patient having braces and metal-containing dental appliances. The thyroid palpated normal without mass or asymmetry, and it was not enlarged. Heart evaluation revealed a normal rate and rhythm without murmur, and lung examination revealed normal breath sounds. Abdominal examination produced no noted tenderness to deep palpation and there were no palpable masses. Neurological examination revealed normal sensory, reflex and motor examinations. Cerebellar testing was negative.
 Initial Impressions
Initial Impressions
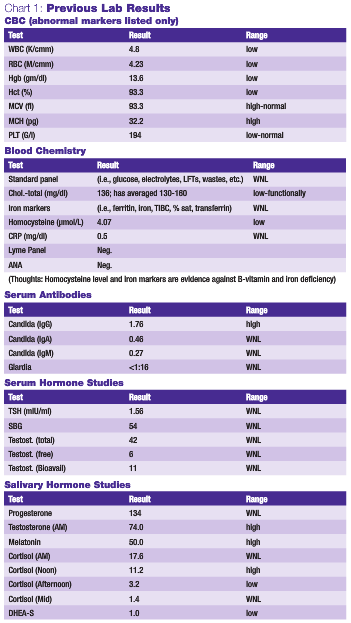
The presence of a broad array of multi-systemic symptoms usually causes the medicine practitioner to ascertain a foundational reason that may correlate to most, if not all, of the patient’s complaints. The prior workup by her medical providers seems to rule out any serious organic disease, making more subtle functional problems the more likely etiology. Foundational problems, such as elevated toxic burden, oxidative stress and sleep deficiency, can lead to global symptomology (i.e., fatigue, metabolic distress, irregular menses, adrenal dysfunction, etc.). Previous laboratory testing performed by her primary medical physician is summarized in Chart 1.
Follow-Up History
After reviewing the previously performed tests, I conducted a more detailed and targeted history. The patient reported that a week after receiving a metal-containing biteplate from her orthodontist, she developed a very sore tongue, with severe redness on the tip and generalized inflamed papillae. Her tongue also became very sensitive to spicy and acidic foods. She thought she might be experiencing thrush, and used a mouthwash containing glycothymoline. She also kept the biteplate out more than in. This seemed to help significantly. After 10 days, she re-introduced the biteplate full-time and developed a severe vaginal yeast infection. She self-treated her yeast infection with oil of oregano extract and grapefruit seed extract topical cream. After 10 days or so, the infection resolved. She later developed an acute fingernail abscess, which was treated with amoxicillin and later Augmentin, but eventually cultured positive for candida.
The diagnostic test results the patient presented with were also reflective of the fact that she had been bitten by a tick during the previous year and had developed a classic bull’s-eye rash on her right hip and lymphadenopathy of the inguinal nodes. A Lyme test was performed and she was prescribed doxycycline for three weeks.
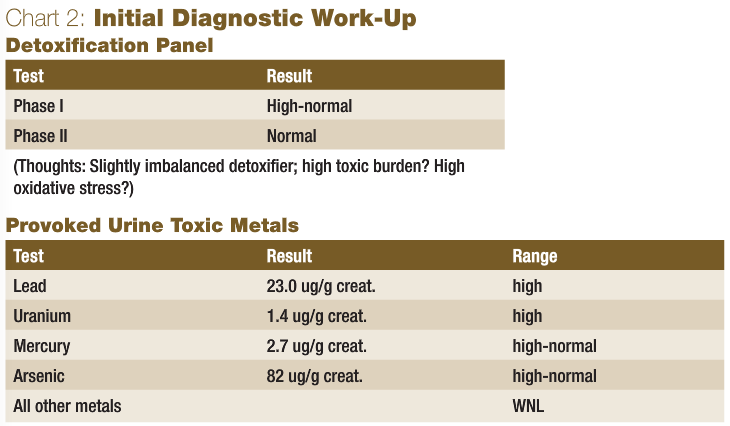
Based on the patient’s updated history and previous testing, my initial diagnostic work-up is shown in Chart 2.
Discussion of Initial Diagnostics
The CBC, basic blood chemistry and thyroid panel were previously performed on this patient, which were appropriate due to her persistent complaints of fatigue. Basic rule-outs, such as anemia, infection and serious internal disorders, had to be performed. While her CBC may be interpreted by some to be reflective of multi-nutritional factor-related anemia, her normal serum iron markers combined with her low homocysteine did not support that conclusion. She also did not have heavy menstrual flow, had a very B-vitamin rich diet, and used supplementation. In this type of case, other reasons for a pancytopenic condition must be considered, including drug side effects, various blood dyscrasias and toxicity (i.e., chemicals and heavy metals). Previously performed serum antibody studies indicated that the patient had been mounting an immune challenge to candida. While the serum hormone markers previously performed on her were normal, salivary hormone studies revealed some imbalances that could explain her irregular menses and excessive sweating, and were likely indicative of functional imbalances of the hormones of the cholesterol-synthesis pathway and catecholamines, possibly secondary to adrenal dysfunction and stress.
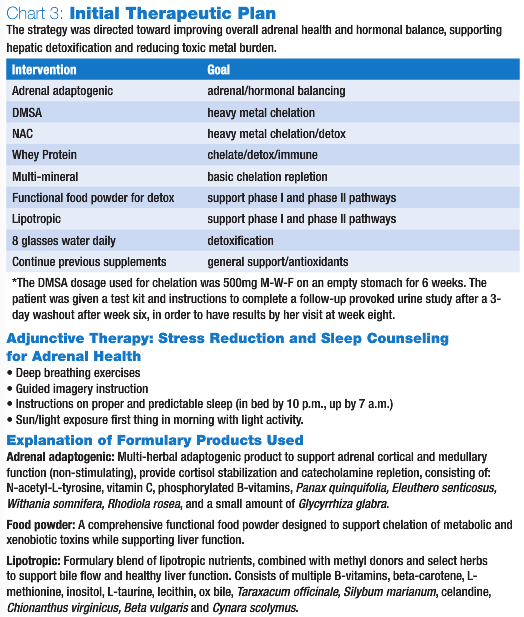
As for the tests performed by myself, the hepatic detoxification panel was ordered to determine the patient’s hepatic performance and her functional ability to detoxify. Since repeated low cholesterol levels can be a sign of poor liver function, many of her symptoms could plausibly have been caused by increased toxic burden and clinical detoxification was potentially necessary, the liver function test was determined to be appropriate. The results showed an increased phase I, with normal phase II activity. This situation made the patient a slight “imbalanced or pathological detoxifier,” which is not optimal, since phase I detoxification results in toxic intermediates, which are more water soluble and readily transported than the original toxin but which must be ultimately conjugated via phase II activity in the liver to mitigate the oxidative stress produced by these radical compounds. If phase I is elevated in a patient, possibly due to significant toxic exposure, the production of toxic intermediates may be greater than the capacity of phase II to conjugate these toxic intermediates rapidly. Due to the patient’s heavy use of antibiotics and her candida problems, a comprehensive stool analysis was suggested, but since there were no overt GI symptoms, the patient and I decided to expend the available financial resources elsewhere. Due to the potential of toxicity, the previous hair analysis results and her metal-containing dental appliances, which she had apparently reacted to in the past, it was determined that a comprehensive evaluation of her toxic metal burden should be performed. A six-hour DMSA (20mg/kg) provoked urine toxic metal analysis was ordered, which revealed elevations of lead and uranium, and levels of mercury and arsenic at the very upper end of the normal range. It was determined that these high-normal values may have been indicative of a high deep-tissue burden, which may become more apparent upon follow-up testing after a course of oral chelation. See Chart 3 for the initial therapeutic plan.
8-Week Follow-Up
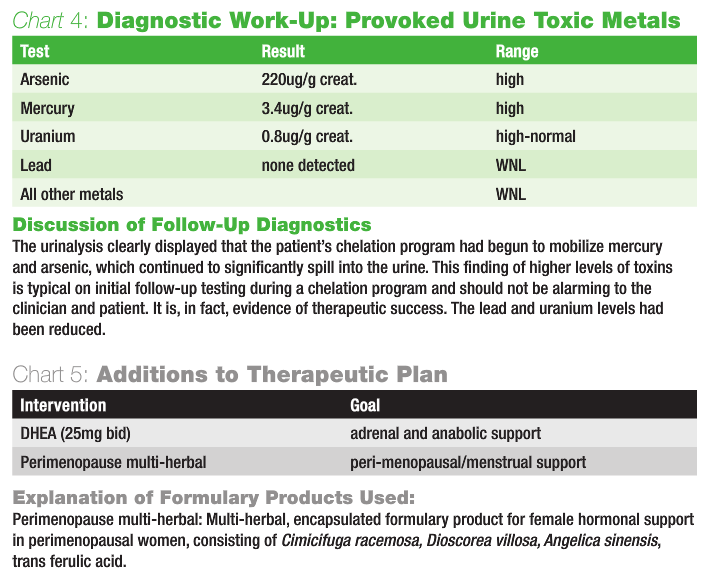
The patient had no specific symptoms other than a mild skin breakout during her first round of chelation. Her sweating problem had not changed over the eight-week period. She complained of dizziness when arising quickly from a lying position and during certain yoga positions. Upon examination, she had a positive Ragland’s test indicative of postural hypotension, with a blood pressure lying down of 105/87 mmHg, and 95/87 mmHg immediately upon standing. Sustained light to the pupils revealed initial constriction, followed by dilation and pulsation. Both the postural hypotension and pupil reactions are indicative of probable continued adrenal dysfunction. The patient also expressed a desire to attempt to better regulate her menses using a natural approach. Chart 4 outlines results from the ordered urinalysis.
The patient was instructed to continue her chelation program for another six weeks, after her two-week rest period from weeks six through eight was completed. The patient was given another test kit and instructions to complete a follow-up provoked urine study after a 3-day washout after week six of her second round of chelation, to have results by her visit at week 16. She was also instructed to continue engaging in stress-reducing recreational activities, as well as all previously prescribed supplements. The follow-up therapeutic strategy continued to be directed toward supporting proper elimination of toxins, reducing oxidative stress, supporting adrenal health, normalizing hormonal balance and menstrual regularity, and enhancing long-term health. Chart 5 outlines additions made to her therapeutic program.
16-Week Follow-Up
Over the course of the patient’s second round of chelation, she experienced a significant vaginal yeast infection. This may have been exacerbated by the immune suppression, which often results from heavy metal toxicity and can exacerbate during chelation programs. She self-treated with oil of oregano topical anti-fungal cream, and the vaginal infection resolved. However, she was experiencing peeling lips and tongue irritation upon presentation and reported that this was common for her when she had a flare-up of yeast. Her mouth still contained the dental appliances, but they were due to be removed within several months. The patient reported that her energy levels had been significantly improving and that she was sleeping eight hours per night. She reported that her sweating issue was much better, but that often improved during the summer months and was exacerbated during the winter, when going from a cold outside environment to warm indoor environment. The postural hypotension issue seemed to have almost completely resolved. Her menstrual cycles had become more regular since starting the herbal therapy at her previous visit, although more time and cycles would be required for a true indication. Follow-up examination revealed no frank oral thrush, although the lips were obviously cracked and irritated. Sitting blood pressure was 100/62 mmHg. Chart 6 shows updated urinalysis results.
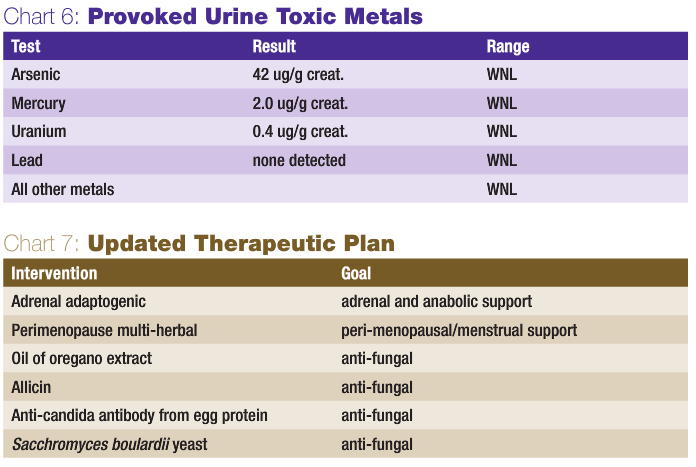 The patient was instructed to discontinue her chelation program. Resumption of chelation will be considered in three to six months, based on results of further provoked urine studies. It often requires multiple chelation cycles over several years with lengthy washout periods to completely eliminate heavy metals from the body. This is particularly true in those patients with significantly high levels of mercury. The patient was also instructed to continue engaging in stress-reducing recreational activities and exercise, as well as to continue her previous basic, not therapeutic, supplement regiment. She was instructed to once again utilize the glycothymoline mouthwash for the mouth irritation and to continue a maintenance dosage of herbal adaptogenic and feminine hormonal support. The patient was also prescribed an aggressive three-week natural anti-fungal protocol (see Chart 7 for details).
The patient was instructed to discontinue her chelation program. Resumption of chelation will be considered in three to six months, based on results of further provoked urine studies. It often requires multiple chelation cycles over several years with lengthy washout periods to completely eliminate heavy metals from the body. This is particularly true in those patients with significantly high levels of mercury. The patient was also instructed to continue engaging in stress-reducing recreational activities and exercise, as well as to continue her previous basic, not therapeutic, supplement regiment. She was instructed to once again utilize the glycothymoline mouthwash for the mouth irritation and to continue a maintenance dosage of herbal adaptogenic and feminine hormonal support. The patient was also prescribed an aggressive three-week natural anti-fungal protocol (see Chart 7 for details).
Discussion
Detoxification and chelation of heavy metals can be a long and arduous process that requires a commitment by the patient in terms of treatment compliance and financial resources. While oral chelation is much less expensive than intravenous chelation, it still often requires a prolonged course of treatment and serial diagnostic testing to monitor progress and produce a successful outcome. It is incumbent on the practitioner to understand the process, have patience and fully explain the entire scope of the problem and process of chelation to the patient at the outset. Mercury, and other metal, toxicity is becoming extremely prevalent. Practitioners who have the ability to accurately detect and treat this problem will create a successful niche within their practices, which can be of great value to patients and communities.
I encourage and welcome questions and comments regarding this case, as well as other clinical issues. Please direct questions to me at dbrady@bridgeport.edu.
 David M Brady, ND, DC, CCN, DACBN is the chief medical officer of Designs for Health and serves as a technical consultant to Metametrix Clinical Laboratory. He presently is director of the Human Nutrition Institute at the University of Bridgeport (UB), and also an association professor of clinical sciences at UB. Brady also maintains a private practice at The Center for the Healing Arts in Orange, Conn., where he specializes in functional and metabolic medicine.
David M Brady, ND, DC, CCN, DACBN is the chief medical officer of Designs for Health and serves as a technical consultant to Metametrix Clinical Laboratory. He presently is director of the Human Nutrition Institute at the University of Bridgeport (UB), and also an association professor of clinical sciences at UB. Brady also maintains a private practice at The Center for the Healing Arts in Orange, Conn., where he specializes in functional and metabolic medicine.