Non-Alcoholic Fatty Liver Disease
Mona Morstein, ND
For most patients, there are no real signs or symptoms that they have a fatty liver, outside of the metabolic syndrome picture they probably will demonstrate. – Mona Morstein, ND
Non-alcoholic fatty liver disease (NAFLD) is a leading problem in our overweight, obese, pre-diabetic, and diabetic patients, no matter the age or sex. It is the main category name of the most common liver disease in the United States. Also known as steatosis, NAFLD indicates that there is increased macrovesicular fat accumulation in the liver. Macrovesicular means that there is enough fat in the liver cell to displace the
nucleus to the edge of the cell and risk causing the cell to burst.
While NAFLD is generally considered to be benign, it is a huge risk factor for the patient to develop non-alcoholic steatohepatitis (NASH), which is far from benign. NASH causes inflammation in the liver which leads to scarring, fibrosis and cirrhosis. In fact, NASH is in the group with alcoholism and hepatitis C as being an established risk factor for liver cirrhosis. NASH is defined as inflammation combined with “ballooning degeneration,” which is when hepatocytes become swollen with granular cytoplasm, causing lysis which attracts lymphocytes or other inflammatory cells which release cytokines in response.
The liver typically contains 5% fat, but when it reaches 10% a “fatty liver” develops. The exact methodology is not wholly understood, but when adipocytes engage in lipolysis it brings free fatty acids (FFA) to the liver. This initiates lipid peroxidation, cytokine induction, and mitochondrial dysfunction, and increased production of TNF-a, interleukins, superoxide and other inflammatory chemicals.
Statistics
The statistics regarding the growth of NAFLD and NASH are frightening. Of all cases of liver disease, 25% are due to NAFLD. It is estimated that 25-35% of the US population has NAFLD. This is understandable given that with 24 million diabetics and 57 million pre-diabetic people in the US, that’s 81 million people who are generally overweight or obese, just under a third of the US population. Greater than 90% of NAFLD patients are associated with aspects of the metabolic syndrome profile and have at least one positive index such as obesity, elevated fasting glucose, elevated triglycerides, elevated LDL, or hypertension; in fact, one-third of NAFLD patients have at least 3 of those features.
Looking at the statistics from another angle, 70-80% of obese patients have NAFLD, and it is up to 100% of morbidly obese patients who have it (defined by having a BMI ≥ 40). Approximately 70% of type 2 diabetic patients have NAFLD and 5%-20% of type 2 diabetics will develop NASH-based cirrhosis as a result. NASH is seen most commonly in Caucasians and Hispanics (but is also seen in other races), it is equal in men and women, and is seen in the overweight and obese pediatric population, too.
Etiological Risk Factors and Differential Diagnosis
There are many etiological risk factors for developing NAFLD/NASH. The below conditions and habits can all promote NAFLD/NASH:
• Obesity and insulin resistance
• Alcohol at or greater than 10 drinks/wk
• Acute fulminant or chronic hepatitis (especially Hep C)
• Drugs: valproic acid, corticosteroids, tamoxifen, estrogens, methotrexate
• Environmental factors: organic solvents, polychlorinated biphenyls (PCBs), petrochemicals, imethylformamide
• Metabolic Abnormalities: galactosemia, glycogen storage disease, homocystinuria
• Nutritional Status: Overnutrition, starvation diet and rapid weight loss, total parenteral nutrition (TPN), proteinenergy malnutrition (PEM), celiac
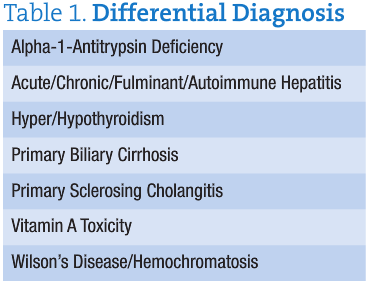
• There are also other conditions which can mimic fatty liver, but these are conditions that need to be properly diagnosed (table 1).
Signs and Symptoms
For most patients, there are no real signs or symptoms that they have a fatty liver, outside of the metabolic syndrome picture they probably will demonstrate. A clinician may palpate hepatomegaly or splenomegaly. Once cirrhosis sets in, patients then exhibit the standard picture. Laboratory analysis includes serum ferritin, elevated as an acute phase marker, although ruling out hemochromatosis is important. That has always been the very first lab index my patients present with.
 Diagnosis
Diagnosis
As NASH develops, elevated ALT > AST presents. Rule out hepatic problems through a good liver panel, as well as the other differential diseases in table 1. A newer test, called FIBROSpect II, shows numerous lab values indicating liver cell injury.
Imaging is difficult. Ultrasound (U/S), a standard inexpensive and non-invasive tool, will not demonstrate fatty liver until the fat has accumulated to 15-30%, which is a very significant advanced amount of fat. Therefore, false negatives can occur with U/S in earlier disease. CT Scan is not used and MRI is gaining ground somewhat, although one cannot discern NAFLD from NASH via MRI. The gold standard is a liver biopsy, which an ND will have to strongly direct a patient to consider doing if blood work clearly suggests a serious case is probably occurring.
NASH can progress to cirrhosis and hepatocellular cancer. Of untreated or poorly treated NAFLD patients, 30% will progress to NASH.
Treatment – Standard Allopathic Care
Standard medical care is not established. Avoidance of alcohol is vital. Slow weight loss is encouraged. Starvation diets, such as hCG or quick weight loss, are a huge risk factor for furthering fatty liver and worsening the denigration of liver cells. These should be avoided in fatty liver patients. They absolutely cannot lose more than 3.5 lbs/wk, although 1-2 lbs/wk is safe and effective for these patients.
Medications used typically include thiazolidinediones, which can slow down liver inflammation during use.
Metformin, exenatid and statins are also used, as well as anti-obesity medications such as orlistat and sibutramine. Some studies show minor benefit of ursodeoxycholic acid lowering steatosis, although it does not improve inflammation or fibrosis. MDs also investigate sleep apnea, and consider bariatric surgery; liver transplantation is necessary in a cirrhotic and failing liver.
Naturopathic Protocols
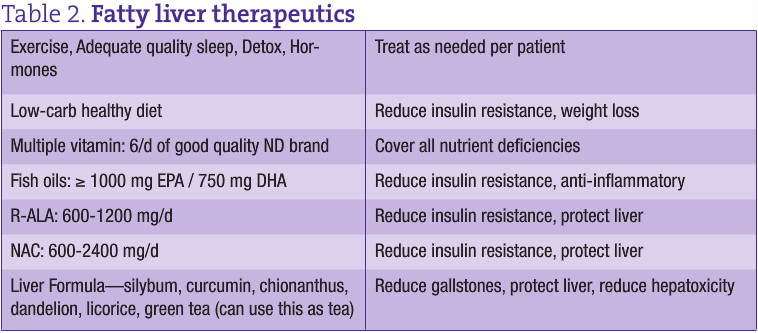
Naturopathic care should include dietary changes, slow weight loss, increasing antioxidants and anti-inflammatory agents, and nutrient support (table 2). The best diet is to incorporate one of insulin resistance—include healthy oils and protein, lowered grains and starchy vegetables, and have good produce intake; eliminate sugar/junk food, trans-fats and overeating. Patients must absolutely exclude alcohol, coffee, and sugary or artificially sweetened drinks. It’s helpful if they eat “bitters” which are good flavor to promote liver/gallbladder functioning.
Exercise must be begun and devoted to with a mix of aerobic and anaerobic types. A cardiovascular analysis of the patient may first need to occur. Good sleep, at least 6-9 hours per night is required, or hormones such as leptin and ghrelin will not be in balance, and appetite control will suffer. Some patients may require environmental detoxification if their past history notably illustrates problematic toxin exposure. Castor oil packs can be nourishing and cleansing to the liver, as well as constitutional hydrotherapy.
Nutrients shown in studies to support fatty livers and insulin resistance include fish oils, chromium, zinc, fiber, Gymnema sylvestre, vitamin D (if deficient), R-alpha lipoic acid (R-ALA), betaine/SAMe, n-acetylcysteine (NAC), mixed vitamin E, selenium, probiotics, lecithin, cholagogue and liver protectant botanicals, curcumin and resveratrol, licorice, green tea, milk thistle, and Cordyceps sinensis.
Follow-up with patients should include weight measurement, dietary, supplementation and exercise compliancy, blood work measuring decrease in lab indices, and repeat of imaging or biopsy. Naturopathic medicine can be immensely helpful to this growing and serious condition plagueing so many of our patients. We need to watch out for fatty livers and initiate protocols to help the liver heal.
 Mona Morstein, ND is Chair of Nutrition, Gastroenterology professor and clinical Supervisor at SCNM. Dr. Morstein is aleading naturopathic expert on pre-diabetes and diabetes and medical problems related to those illnesses. She is a common speaker on diabetes throughout the naturopathic profession. Dr. Morstein is also owner/moderator of NaturopathicChat on Yahoo, the largest naturopathic email group in the world.
Mona Morstein, ND is Chair of Nutrition, Gastroenterology professor and clinical Supervisor at SCNM. Dr. Morstein is aleading naturopathic expert on pre-diabetes and diabetes and medical problems related to those illnesses. She is a common speaker on diabetes throughout the naturopathic profession. Dr. Morstein is also owner/moderator of NaturopathicChat on Yahoo, the largest naturopathic email group in the world.
References
1. Albano, E, Mottaran, E. et al, Alimentary Pharmacology and Therapeutics, Vol 22 Issue 2, 71-73, 10/14/05 AND Day, CP et al, NASH. Gastroenterology 1998, 114:842
2. (Statistics) Centers For Disease Control; Dr. Melissa Palmer “Hepatitis and Liver Disease”.
3. (Differntial diagnosis) AGA Medical Position Statement: Non-Alcoholic Fatty Liver Disease, Gastroenterology 2002; 123:1702-1704 AND Valera, JM, Hurtado C, Et al, Study of Celiac Disease in patients with non-alcoholic fatty liver and autoimmune hepatic diseases. Gastroenterology Hepatol. 2008 Jan; 31(1):8-11.
4. (U/S) Anna Wieckowsak Nonalcoholic Fatty Liver Disease, Cleveland Clinic Meded.com AND Radu, Corina, Grigorescu, Mircea, Et al, “Prevalence and Associated Risk Factors of Non-Alcoholic Fatty Liver Disease in Hospitalized Patients”, Journal of Gastrointestinal and Liver Diseases. www.jgld.ro/32008/32008_1.html
5. (Progression to NASH): Farrell GC, Larter CZ, “Nonalcoholic Fatty liver disease: from steatosis to cirrhosis”. Hepatology. 2006 Feb; 43(2 Suppl 1): S99-S112.