Ronald Steriti, ND, PhD
Herpes zoster is a painful vesicular eruption caused by the varicella zoster virus (VZV). It is marked by inflammation of the posterior root ganglia of the spinal or cranial peripheral nerves. After a prodromal illness of pain and paresthesias, erythematous macules and papules develop and progress to vesicles within 24 hours. The vesicles eventually crust and resolve. The crusts fall off in 2 to 3 weeks, leaving behind pink, healing skin.
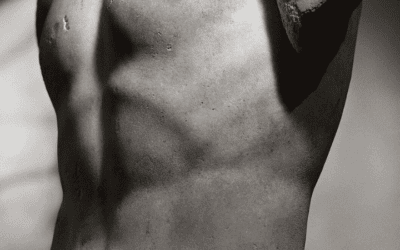
The vesicles typically appear along a single dermatome, and are almost always unilateral. The trunk is most often affected, showing a rectangular belt of rash from the spine around one side of the chest to the sternum.
Herpes zoster ophthalmicus involves the first division of the trigeminal nerve. Ocular complications may lead to permanent blindness if not treated with emergency medical care.
Herpes zoster may be complicated by postherpetic neuralgia, which is persistence of pain caused by irritation of the nerve roots of the spinal cord. This may last from months to years following the initial episode. The pain can be severe enough to be incapacitating, and the elderly are at higher risk (Jung et al., 2004).
Ramsay Hunt syndrome is herpes zoster oticus, an infection of the external auditory canal, associated with severe acute facial paralysis (Uscategui et al., 2008).
Causes
Once a patient has been infected with the varicella zoster virus, the herpes zoster virus lies dormant in the posterior root ganglia. The cause of activation is usually unknown, but seems to be linked to aging, stress or an impaired immune system.
Widespread or recurrent herpes zoster may indicate an underlying problem with the immune system, such as leukemia, Hodgkin’s disease or other cancers, atopic dermatitis, HIV infection or AIDS. People with suppressed immune systems due to organ transplant or treatment for cancer are also at risk.
Data from two large databases suggested that patients with rheumatoid arthritis are at increased risk of herpes zoster. Among patients with rheumatoid arthritis, disease-modifying antirheumatic drugs and/or use of oral corticosteroids appeared to be associated with herpes zoster (Smitten et al., 2007).
Conventional Lab Tests
Herpes zoster is generally identified by the clinical presentation, but tests may include:
- Viral culture of skin lesion
- Tzanck smear, which is helpful for diagnosing acute infection with a herpes virus, but does not distinguish between HSV and VZV
- Complete blood count (CBC), which may show elevated white blood cells, a nonspecific sign of infection
- VZV-specific IgM antibody, which only appears during active varicella zoster or herpes zoster and not while the virus is dormant
- Polymerase chain reaction (PCR) test for VZV DNA
Conventional Treatments
Conventional medications for acute infection include:
- Antivirals: acyclovir, famciclovir and valacyclovir
- Anti-inflammatories: corticosteroids
Conventional treatments for postherpetic neuralgia include:
- Analgesics: commercially available topical capsaicin cream
- GABA analogues: gabapentin, pregabalin
- Tricyclic antidepressants for pain relief
- Opioids for pain relief (Mounsey et al., 2005)
Capsaicin: Capsaicin is a powerful natural pain reliever that lowers the levels of substance P (Mounsey et al., 2005; Fusco and Giacovazzo, 1997; Appendino and Szallasi, 1997; Watson et al., 1993). One study, however, found that it resulted in higher average daily pain and allodynia ratings (Petersen et al., 2000).
Gabapentin: Gabapentin is a drug similar in structure to the neurotransmitter GABA. In 2002, gabapentin was approved for treating postherpetic neuralgia (Moulin, 2006; Beydoun, 1999).
Pregabalin: The U.S. Food and Drug Administration (FDA) approved pregabalin in December 2004 for the treatment of neuropathic pain associated with diabetic peripheral neuropathy and postherpetic neuralgia (Tassone et al., 2007).
Prostaglandin E1: One study found intravenous administration of prostaglandin E1 produces prompt and continuous analgesia in patients with postherpetic neuralgia; PGE(1) has an analgesic effect via improvement of peripheral blood circulation (Kanai et al., 2007).
Natural Support
There are several approaches to herpes zoster, including:
- Antivirals: Ganoderma, betadine
- Topical analgesics: peppermint oil, geranium oil
- Nutritional support for the skin: vitamin A, vitamin C, lipoic acid
- Diet: fruits
Antivirals
Ganoderma lucidum: Ganoderma lucidum is a mushroom that modulates the immune system and has potent antiviral activity (Paterson, 2006; Niedermeyer et al., 2005). One study found that a hot water extract of Ganoderma lucidum decreased herpes zoster pain for five Japanese patients. Pain relief started within a few days of intake and was almost complete within 10 days. In the same study, two cases of acute herpes zoster with manifestations, including trigeminal nerve ophthalmia (both patients were 74 years old); one with lower body zoster (70 years old); one with herpes zoster oticus (17 years old); and one with leg herpes (28 years old); responded quickly to treatment. No patient developed post-herpetic neuralgia after more than one year of follow-up (Hijikata et al., 2005).
An earlier study by two of the same researchers found that hot water-soluble extracts of Ganoderma lucidum decreased pain dramatically in two patients with postherpetic neuralgia recalcitrant to standard therapy and two other patients with severe pain due to herpes zoster infection (Hijikata and Yamada, 1998).
Betadine: An article published in 1977 found that Betadine (povidone iodine) antiseptic paint had “good results” in 12 patients with herpes zoster (Woodbridge, 1977).
Topical Analgesics
Peppermint oil: A case report described a 76-year-old woman with post-herpetic neuralgia whose pain had been resistant to standard therapies. The patient was instructed to apply neat peppermint oil (containing 10% menthol) to her skin, resulting in an almost immediate improvement in her pain. This pain relief persisted for 4-6 hours after application of the oil (Davies et al., 2002).
Geranium oil: An article published in the American Journal of Medicine described a multicenter, double-blind crossover study on the use of geranium oil for subjects with moderate to severely painful post-herpetic neuralgia. Geranium oil treatment was associated with a significant reduction in pain for spontaneous and evoked pain, as compared with placebo. Adverse reactions were minor. Geranium oil relieves pain in minutes, and 25% had dramatic pain relief (Greenway et al., 2003).
Nutritional Support for the Skin
Vitamin A: One study found that a deficiency of plasma retinol (vitamin A) is common, particularly in subjects with severe mucositis, and is associated with an increased risk of herpes zoster infection in recipients of hematopoetic stem cell transplant (High et al., 2002).
Vitamin C: A case study published in Anesthesia and Analgesia described a 78-year-old man with intractable T3-6 postherpetic neuralgia. Lab tests were normal except for a low concentration of vitamin C. Treatment with IV ascorbate (2.5g on days 1, 3 and 5) resulted in complete resolution of the intermittent, spontaneous shooting pain and a decrease of his baseline pain (Chen et al., 2006).
An old article published in 1950 mentioned the use of intravenous vitamin C for herpes zoster (Zureick, 1950).
Lipoic acid: Two articles mention the use of lipoic acid for postherpetic neuralgia (Gidal, 2006; Braune, 2004).
Diet: Fruit
A recent study of 243 herpes zoster cases and 483 controls found that individuals who ate less than one piece of fruit per week had more than three times the risk of zoster compared with individuals who ate more than three portions per day (Thomas et al., 2006).
Alternative Therapies
One study used a combination of TCM (acupuncture, cupping and bleeding, and Chinese herbs), local anesthetic filtration and nerve block (German Neural Therapy) with 1% procaine injection on the affected dermatome, and meditation. For all 56 patients, there was a 72.1% average reduction of pain. No significant side effects were reported (Hui et al., 1999).
Misdiagnosis
One article described a patient with a second-degree burn of the forehead, induced by topical application of crushed garlic, which mimicked herpes zoster (Farrell and Staughton, 1996).
 Ron Steriti, ND, PHD is a graduate of SCNM. He is professionally trained in the use of vitamins, herbs, nutritional supplements and classical homeopathy, and is licensed as an ND by the state of Vermont. Dr. Ron’s passions are botani-cal medicine and clinical nutrition based on published scientific research, along with classical homeopathy. He has written extensive nutrition research articles on a variety of chronic dis-eases, and has developed a holistic medical database that keeps him up to date on the latest research.
Ron Steriti, ND, PHD is a graduate of SCNM. He is professionally trained in the use of vitamins, herbs, nutritional supplements and classical homeopathy, and is licensed as an ND by the state of Vermont. Dr. Ron’s passions are botani-cal medicine and clinical nutrition based on published scientific research, along with classical homeopathy. He has written extensive nutrition research articles on a variety of chronic dis-eases, and has developed a holistic medical database that keeps him up to date on the latest research.
References
Appendino G, Szallasi A: Euphorbium: modern research on its active principle, resiniferatoxin, revives an ancient medicine, Life Sci 60(10):681-96, 1997.
Beydoun A: Postherpetic neuralgia: role of gabapentin and other treatment modalities, Epilepsia 40(Suppl 6):S51-6, 1999.
Braune S: Evidence-based pharmacotherapy of neuropathic pain syndromes (translated), MMW Fortschr Med 146(50):49-51, 2004.
Chen JY et al: Treatment of postherpetic neuralgia with intravenous administration of vitamin C, Anesth Analg 103(6):1616-7, 2006.
Davies SJ et al: A novel treatment of postherpetic neuralgia using peppermint oil, Clin J Pain 18(3):200-2, 2002.
Farrell AM, Staughton RC: Garlic burns mimicking herpes zoster, Lancet 347(9009):1195, 1996.
Fusco BM, Giacovazzo M: Peppers and pain. The promise of capsaicin, Drugs 53(6):909-14, 1997.
Gidal BE: New and emerging treatment options for neuropathic pain, Am J Manag Care 12(9 Suppl):S269-78, 2006.
Greenway FL et al: Temporary relief of postherpetic neuralgia pain with topical geranium oil, Am J Med 115(7):586-7, 2003.
High KP et al: Low plasma concentrations of retinol and alpha-tocopherol in hematopoietic stem cell transplant recipients: the effect of mucositis and the risk of infection, Am J Clin Nutr 76(6):1358-66, 2002.
Hijikata Y, Yamada S: Effect of Ganoderma lucidum on postherpetic neuralgia, Am J Chin Med 26(3-4):375-81, 1998.
Hijikata Y et al: Effect of an herbal formula containing Ganoderma lucidum on reduction of herpes zoster pain: a pilot clinical trial, Am J Chin Med 33(4):517-23, 2005.
Hui F et al: Integrative approach to the treatment of postherpetic neuralgia: a case series, Altern Med Rev 4(6):429-35, 1999.
Jung BF et al: Risk factors for postherpetic neuralgia in patients with herpes zoster, Neurology 62(9):1545-51, 2004.
Kanai A et al: Effectiveness of prostaglandin E1 for the treatment of patients with neuropathic pain following herpes zoster, Pain Med 8(1):36-40, 2007.
Moulin D: Does acute pain associated with herpes zoster respond to treatment with gabapentin?, Nat Clin Pract Neurol 2(6):298-9, 2006.
Mounsey AL et al: Herpes zoster and postherpetic neuralgia: prevention and management, Am Fam Physician 72(6):1075-80, 2005.
Niedermeyer TH et al: Antiviral terpenoid constituents of Ganoderma pfeifferi, J Nat Prod 68(12):1728-31, 2005.
Paterson RR: Ganoderma – a therapeutic fungal biofactory, Phytochemistry 67(18):1985-2001, 2006.
Petersen KL et al: Capsaicin evoked pain and allodynia in post-herpetic neuralgia, Pain 88(2):125-33, 2000.
Smitten AL et al: The risk of herpes zoster in patients with rheumatoid arthritis in the United States and the United Kingdom, Arthritis Rheum 57(8):1431-8, 2007.
Tassone DM et al: Pregabalin: A novel gamma-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders, Clin Ther 29(1):26-48, 2007.
Thomas SL et al: Micronutrient intake and the risk of herpes zoster:a case-control study, Int J Epidemiol 35(2):307-14, 2006.
Uscategui T et al: Antiviral therapy for Ramsay Hunt syndrome (herpes zoster oticus with facial palsy) in adults, Cochrane Database Syst Rev Oct 8;(4):CD006851, 2008.
Watson CP et al: A randomized vehicle-controlled trial of topical capsaicin in the treatment of postherpetic neuralgia, Clin Ther 15(3):510-26, 1993.
Woodbridge P: The use of betadine antiseptic paint in the treatment of Herpes simplex and Herpes Zoster, J Int Med Res 5(5):378-81, 1977.
Zureick M: Therapy of herpes and herpes zoster with intravenous vitamin C (translated), J Prat Rev Gen Clin Ther 64(48):586, 1950.