Pain Disrupts Sleep… The Sleep that Eases Pain
Catherine Darley, ND
How many of your chronic pain patients have difficulty sleeping? Does this sleep disturbance contribute to their pain? In a word, yes. It has been found that sleep loss itself is hyperalgesic, and that when chronic pain patients sleep better their pain is reduced.
Sleep Loss Is Hyperalgesic
In recent research, when healthy study participants were allowed only 4 hours of sleep each night for 12 nights, they reported more generalized body pain, back pain, and stomach pain symptoms than when they slept 8 hours each night.1 It is also relevant that their factor-derived variable of sociability–optimism decreased by 15%. The authors conclude “The data suggest that chronic insufficient sleep may contribute to the onset and amplification of pain and affect health by compromising optimistic outlook and psychosocial functioning.”1 Keep in mind that insufficient sleep is probably the most prevalent sleep disorder in America, with only 28% of adults getting the recommended 8 hours or more each night.2
Pain Itself Disturbs Sleep
Multiple studies have looked at how pain disturbs sleep. This is done in people who are not experiencing chronic pain. Several painful stimuli have shown this effect. The first study to discuss was conducted in 2004 by Lavigne et al.3 In this study a hypertonic saline injection was administered during the day, and reported to be painful. That same hypertonic saline injection was given during several sleep stages. It awoke the participants 40% of the time in Stage 2 sleep, 26.7% in deep sleep, and 45.8% in REM. We would expect the pain to awaken the person more during REM as people generally awaken more easily out of REM sleep.
Another method of administering pain during sleep to volunteer subjects is by electrical nerve stimulation that produces a reflex movement.4 Even during sleep this painful nerve stimulation causes a reflex movement, although it is attenuated. In a study of 6 healthy volunteers, as compared with the control values there was a significant increase in the reflex threshold both during NREM and REM sleep. During NREM sleep the reflex threshold showed an increase of 60%. During REM sleep the reflex threshold was 207% higher than the baseline values.4 Looking at these divergent types of pain administration, we can see that various kinds of pain can disturb sleep.
Sleep Disorders in Chronic Pain Conditions
Now let’s look at the sleep of people experiencing various pain conditions. One of the conditions most associated with pain is fibromyalgia. Seventy percent report unrefreshing sleep, including more difficulty falling asleep, staying asleep, waking prematurely, and having fewer hours of sleep.5 On overnight sleep testing, fibromyalgia patients have more stage 1 sleep, more arousals and lower sleep efficiency, similar to those with primary insomnia. In one notable study, 27 of 28 fibromyalgia patients were found to have sleep disordered breathing (SDB).6 When the SDB was treated with nasal continuous positive airway pressure (CPAP), their functional symptoms improved by 23-47%. What other treatment do we know of that will cause such a reduction in pain severity?
Other chronic pain diseases are associated with sleep disturbances. Eighty percent of cluster headache patients have obstructive sleep apnea.7 Subjectively, many irritable bowel syndrome patients experience poor sleep quality, low sleep efficiency, and significant sleep disturbance.5
How Can We Improve the Sleep of Chronic Pain Patients?
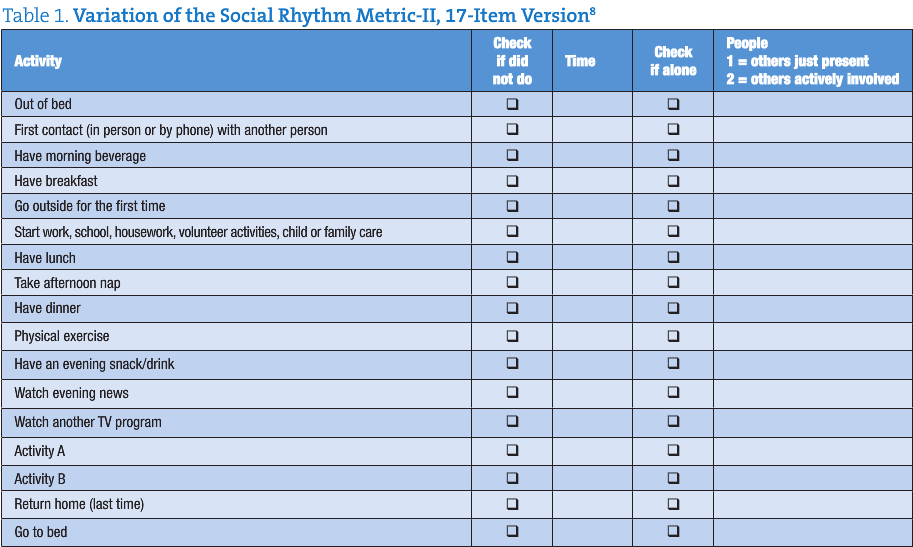
Anecdotally, we hear from pain patients in the clinic that their sleep is disturbed at night by pain. We also learn that they compensate for this by ‘catching up’ on their sleep during the day with naps, or rest periods. Commonly these patients tell of an irregular sleep pattern and lifestyle. A unique tool to capture lifestyle regularity is the Social Rhythm Metric (SRM), developed by Dr. Timothy Monk (table 1).
Monk has found in his extensive work with the SRM, that those people who have the least regularity have a higher prevalence of certain disorders, including anxiety. “Greater variability in rise time, consuming a morning beverage, returning home for the last time, and bedtime were associated with more disturbed sleep.”9 When working with a pain patient we can use this tool to promote greater lifestyle regularity, which in turn will decrease sleep disturbance.
Another documented method to help chronic pain patients sleep is Cognitive-Behavioral Treatment for Insomnia (CBT-I). A group of patients who had insomnia secondary to chronic pain underwent group CBT-I.10 After completion of the program, improvement was seen in sleep latency, time awake after sleep onset, and sleep efficiency.
At the 3-month follow-up post treatment their sleep had continued to improve and there was a trend towards pain reduction. For further discussion of CBT-I, see the April 2009 issue of NDNR.
Lastly, for those chronic pain patients who are on medication for pain, reviewing and adjusting their medication may improve their sleep. Table 2 shows a comparison of some common pain medications and their impact on sleep.11
Summary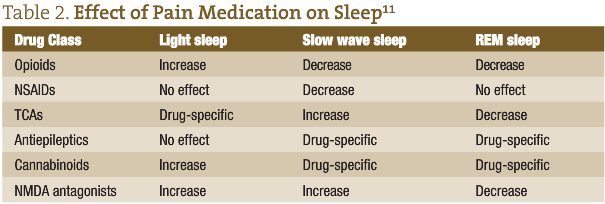
We’ve discussed above how the sleep of chronic pain patients is disturbed, and how sleep disruption itself increases pain. Thus this patient can get into a relentless cycle whereby they can’t sleep because of pain, and the pain is worse because of insufficient sleep. To break this cycle we as naturopathic physicians can first evaluate whether the patient has a sleep disorder such as obstructive sleep apnea or insomnia, among others. Any sleep disorder must be effectively treated. Secondly, we can improve their sleep health by promoting lifestyle regularity. Lastly, we can conduct medication review to ensure no substance is worsening their sleep. With this comprehensive approach we can improve the sleep of the chronic pain patient, and thus decrease their pain.
 Catherine Darley, ND, a graduate of Bastyr University, practices at The Institute of Naturopathic Sleep Medicine in Seattle. Dr. Darley is passionate about the role healthy sleep plays in overall health and quality of life, and is pioneering the field of naturopathic sleep medicine. She gained her expertise by working in the field of sleep research and medicine through naturopathic medical school, and doing multiple preceptorships and post-graduate courses with sleep specialists. In addition to providing patient care, she works to educate the public about sleep health.
Catherine Darley, ND, a graduate of Bastyr University, practices at The Institute of Naturopathic Sleep Medicine in Seattle. Dr. Darley is passionate about the role healthy sleep plays in overall health and quality of life, and is pioneering the field of naturopathic sleep medicine. She gained her expertise by working in the field of sleep research and medicine through naturopathic medical school, and doing multiple preceptorships and post-graduate courses with sleep specialists. In addition to providing patient care, she works to educate the public about sleep health.
References
- Haack M, Mullington JM. Sustained sleep restriction reduces emotional and physical well-being. Pain. 2005;119(1-3):56-64.
- 2009 Sleep in America Poll Highlights. National Sleep Foundation Web site. http://www.sleepfoundation.org/sites/default/files/2009%20POLL%20HIGHLIGHTS.pdf. Published March 2, 2009. Accessed May 6, 2010.
- Lavigne G, Brousseau M, Kato T, et al. Experimental pain perception remains equally active over all sleep stages. Pain. 2004;110(3):646-655.
- Sandrini G, Milanov I, Rossi B, et al. Effects of sleep on spinal nociceptive reflexes in humans. Sleep. 2001;24(1):13-17.
- Shaver JLF. Sleep disturbed by chronic pain in fibromyalgia, irritable bowel, and chronic pelvic pain syndromes. Sleep Medicine Clinics. 2008;3(1):47-60.
- Gold AR, Dipalo F, Gold MS, Broderick J. Inspiratory airflow dynamics during sleep in women with fibromyalgia. Sleep. 2004;27(3):459-466.
- Chervin RD, Zallek SN, Lin X, Hall JM, Sharma N, Hedger KM. Sleep disordered breathing in patients with cluster headache. Neurology. 2000;54(12):2302-2306.
- Monk TH, Flaherty JF, Frank E, Hoskinson K, Kupfer DJ. The Social Rhythm Metric. An instrument to quantify the daily rhythms of life. J Nerv Ment Dis. 1990;178(2):120-126.
- Carney CE, Edinger JD, Meyer B, Lindman L, Istre T. Daily activities and sleep quality in college students. Chronobiol Int. 2006;23(3):623-637.
- Currie SR, Wilson KG, Pontefract AJ, deLaplante L. Cognitive-behavioral treatment of insomnia secondary to chronic pain. J Consult Clin Psychol. 2000;68(3):407-416.
- Lavigne G, Sessl BJ, Choiniere M, Soja PJ, eds. Sleep and Pain. Seattle, WA: IASP Press; 2007:385.