Healed by Regenerative Injection Therapy (RIT)
After Surgical Refusal
David A. Tallman, DC, NMD
 I would like to preface this article by encouraging physicians to refer all patients with tibial eminence fractures to reputable orthopedic surgeons who are keen on the latest and least invasive techniques. I accepted this case only due to the behest of the patient and because I have performed thousands of knee regenerative injection procedures. I do not recommend using this treatment as the sole means of therapy in the way this case was presented, and I strongly and emphatically discourage any non-orthopedic surgeon from taking on this type of trauma in his or her practice
I would like to preface this article by encouraging physicians to refer all patients with tibial eminence fractures to reputable orthopedic surgeons who are keen on the latest and least invasive techniques. I accepted this case only due to the behest of the patient and because I have performed thousands of knee regenerative injection procedures. I do not recommend using this treatment as the sole means of therapy in the way this case was presented, and I strongly and emphatically discourage any non-orthopedic surgeon from taking on this type of trauma in his or her practice
Tibial intercondylar eminence fractures occur due to a forced hyperextension coupled with lateral or rotational movement between the femur and tibia, which place a pathological force upon the anterior cruciate ligament (ACL) that, instead of tearing the ligament, causes an avulsion of the tibial spine bone that the ACL is rooted into. This injury is more common in pediatric and adolescent patients due to the chondroepiphyseal nature1 of the skeletally immature. Bicycling is one of the most common causes of tibial spine fractures2, and some suggest that if knee effusion occurs after a bicycling injury, a tibial spine fracture is present until proven otherwise.
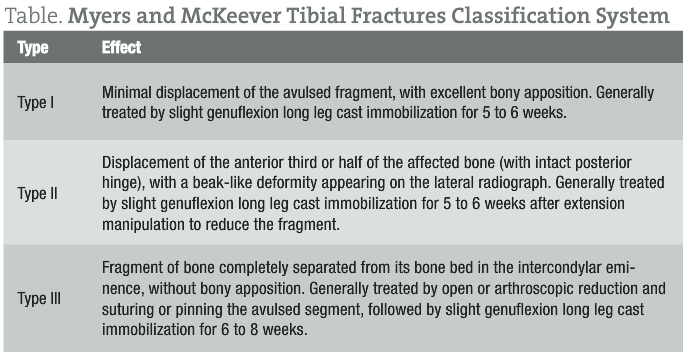
Meyers and McKeever proposed a classification system to describe the severity of tibial fractures to assist surgeons in clinical decision-making, as timing of the treatment for this type of fracture is vital to prevent non-union.
Case History
A PubMed search of tibial spine fractures/tibial eminence fractures reveals a mixed consensus of whether to surgically reduce Type II fractures. Many novel arthroscopic procedures that use absorbable pins and sutures to treat type II and III fractures have been developed over the past couple of years.
I will refer to this patient as Thomas. He presented to my office on August 24, 2010, with an antalgic gait and wore a neoprene brace over his knee. He brought with him his ER notes and a CT scan that was performed at the hospital on the day of the trauma. Exactly one month prior (July 24, 2010) while playing soccer, he sustained a knee injury when he attempted to pivot on an extended knee with his cleated shoe planted in the grass. Thomas noted immediate pain, joint swelling, and an inability to bear weight on his right knee. His friends carried him to the emergency room, where radiographs were taken and a cursory orthopedic exam was performed. The ER doctor interpreted the plain films as negative for fractures, and the orthopedic exam did not reveal ligamentous instability. Thomas was sent home with a prescription of oxycodone and crutches. The hospital staff called Thomas at home a few hours later and asked him to return to the hospital for follow-up imaging. According to the ER notes, a tibial spine fracture was suspected after a radiologist had a chance to read the plain films. Thomas returned to the hospital for a CT scan that revealed a central tibial spine fracture with a 3 mm to 4 mm cranial distraction of the central fracture fragment. He was told to follow up with an orthopedic surgeon in 7 days (July 31, 2010).
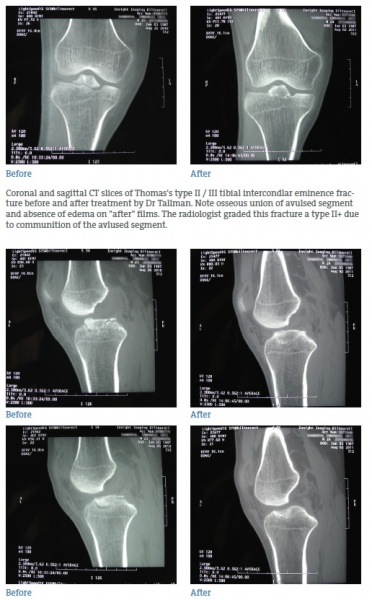
 Thomas, a banquet server, informed me that he did not visit the orthopedic surgeon as scheduled because he did not have insurance and he could not stop working, as his significant other was soon expecting the birth of their first child. I sent Thomas for a follow-up CT scan and had him return the following day. A CT scan dated August 26, 2010, with 3D rendering, demonstrated a mildly communited tibial eminence fracture with a 3.4 mm fracture margin separation along the medial aspect with superior positioning and slight dorsal tilt of the anterolateral aspect of the avulsed segment. I strongly emphasized to Thomas the necessity for arthroscopic surgical fixation of the avulsed segment, as he already had developed a non-union of the fractured segment and was subsequently at risk for early joint degeneration and derangement.
Thomas, a banquet server, informed me that he did not visit the orthopedic surgeon as scheduled because he did not have insurance and he could not stop working, as his significant other was soon expecting the birth of their first child. I sent Thomas for a follow-up CT scan and had him return the following day. A CT scan dated August 26, 2010, with 3D rendering, demonstrated a mildly communited tibial eminence fracture with a 3.4 mm fracture margin separation along the medial aspect with superior positioning and slight dorsal tilt of the anterolateral aspect of the avulsed segment. I strongly emphasized to Thomas the necessity for arthroscopic surgical fixation of the avulsed segment, as he already had developed a non-union of the fractured segment and was subsequently at risk for early joint degeneration and derangement.
Thomas calmly refused my referral to an orthopedic surgeon and told me that if I did not treat him, he would continue to carry on working and limping on his injured knee. With a signed consent as to the awareness of the nature and gravity of his injury and also of the consequences of non-surgical intervention, I cautiously agreed to treat Thomas’s knee.
Treatment
On a monthly basis I performed a series of regenerative injection therapy around the circumference of the avulsed segment, fashioned after a direct needling method I pioneered. I also treated the medial and lateral collateral, transverse intermeniscal, and coronary ligaments, as well as the medial meniscus tibial anchoring fibers and meniscal roots. After his third treatment, Thomas stopped wearing the brace due to lack of perceived instability and pain. His knee effusion was also no longer present after his third treatment. After his fifth treatment, Thomas was no longer experiencing pain or dysfunction unless he performed a deep squat. He stated that he could work all day without any pain or tiredness in his knee. Thomas did not return to his follow-up visit after his sixth treatment (Jan 3, 2011) due to his knee feeling normal again. He agreed to my insistence on a follow-up CT months later to determine resolution of non-union.
Follow-up
The CT scan dated August 2, 2011, demonstrated that the tibial eminence fracture has healed with osseous union to the tibia, with the tibial eminence remaining in elevated position. The radiologist also noted a complete resolution of prior joint effusion. He informed my office staff that Thomas has returned to normal activities, although a little guarded while playing soccer.
Conclusion
An MR scan would have been ideal to evaluate the menisci, the cruciate ligaments, and articular cartilage shortly after the injury. Obtaining an MR scan is important to determine meniscal injury, as the CT scan cannot be relied upon to rule out a meniscus tear3. Follow-up CT was chosen because the initial diagnosis and reference point of the avulsion was made by CT. Even though the avulsion was healed, I still believe that arthroscopic fixation would have been the treatment of choice to position the eminence in its original position. It is possible that the eminence could have healed in a correct position if a knee extension manipulation maneuver followed by non-weight bearing was performed after the first RIT. Nonetheless, it is interesting that Thomas’s osseous union occurred without any periods of non-weight bearing and having continued to work daily as a banquet server during the course of the entire treatment. The treatments also possibly addressed ACL trauma and laxity that can occur due to stretch and elevated union4.
 David A. Tallman, DC, NMD graduated from Texas Chiropractic College in 1999 and SCNM in 2002. His practice has been limited to orthopedics since graduation, and he has performed more than 14 000 spine and joint regenerative injection procedures.
David A. Tallman, DC, NMD graduated from Texas Chiropractic College in 1999 and SCNM in 2002. His practice has been limited to orthopedics since graduation, and he has performed more than 14 000 spine and joint regenerative injection procedures.
References
1. Woo SL, Hollis JM, Adams DJ, et al. Tensile properties of the human femur-anterior cruciate ligament-tibia complex: The effects of specimen age and orientation. Am J Sports Med. 1991;19(3):217-225.
2. Nichols, JN, Tehranzadeh, J. A review of tibial spine fractures in bicycle injury. Am J Sports Med. 1987;15:172-174.
3. Mui LW, Engelsohn E, Umans H. Comparison of CT and MRI in patients with tibial plateau fracture: Can CT findings predict ligament tear or meniscal injury? Skeletal Radiol. 2007;36(2):145-51. Epub. Nov 30, 2006.
4. Reeves KD, Hassanein KM. Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity. Altern Ther Health Med. 2003; 9(3):58-62.

