Dicken Weatherby, ND and Donald R. Yance, CN, MH, RH
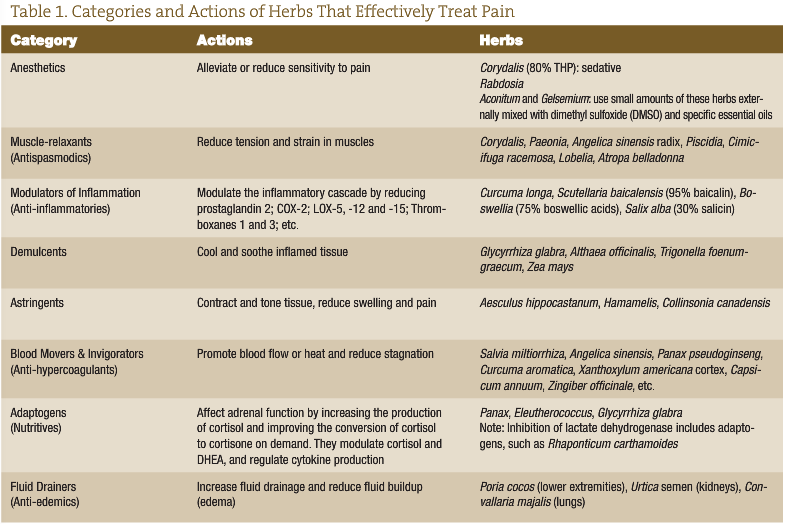
Pain is one of the most common and dreaded symptoms associated with cancer. Botanical and nutritional intervention can provide enormous benefits for controlling cancer pain while at the same time inhibiting the inflammatory-angiogenic process involved in the promotion, progression and invasion of cancer. This article will describe some of the treatments to consider as alternative and/or complementary ways to support patients with cancer who are experiencing pain. This is an overview, and not a comprehensive one, as there is far more we could report on and explore than we have space for in one article.
Cancer-Related Pain
Pain occurs in one-quarter to one-half of patients with newly diagnosed malignancies, in one-third of those undergoing treatment and in more than three-quarters with advanced disease. Overall, 75% of cancer patients who experience pain have pain severe enough to require treatment with opioids. Unrelieved pain directly affects patients’ daily activities, quality of life and psychological status (Twycross and Fairfield, 1982; Cleeland, 1984; Foley, 1985).
Analgesic regimens used are often inadequate, causing patients to experience unnecessary pain, as well as debilitating side effects such as constipation, lack of appetite, fatigue, depression and psychological distress.
Using certain botanical compounds can have a profound effect on relieving pain and associated side effects, improving the quality of life and even improving overall health. Our philosophy is that doctors should never stop helping people with herbs, even up to their transition. It is imperative that healthcare providers be adept at the evaluation and treatment of cancer pain, especially with the availability of excellent botanical-based analgesic therapies.
The effective management of cancer pain hinges on a comprehensive pain assessment, including a history of the pain, including information about its etiology, as well as a complete description of the site(s), pattern, intensity and pathophysiology of the pain (i.e., somatic, visceral, neuropathic; Foley, 2001); physical exam, including a complete neurological examination; relevant diagnostic testing; and the development of a management plan.
There are many contributing factors to consider when treating cancer-related pain with botanical-based formulas. Ask patients to describe their pain and all other symptoms, to help provide an idea of how best to treat them.
Tumor Burden
Cancer patients frequently have more than one cause and more than one locus of pain. In addition, many cancer patients present with a combination of pain types (e.g., visceral and somatic pain; Foley, 2001). The most common causes of cancer-related pain have to do with a tumor invading a particular area of the body, which can result in pressure on an organ or nerve (neuropathic pain). If cancer invades the bone, it causes severe bone pain due to stretching of the periosteum by the cancer, or by stimulation of nerves within the bone.
Inflammation
Inflammation promotes cancer and pain, and cancer promotes inflammation. It is a vicious cycle that must be a focus of botanical intervention when treating any stage of cancer, particularly advanced cancer. The most common pro-inflammatory pathways involved in cancer initiation, promotion and progression are cyclooxygenase (COX)-2 and lipoxygenase (LOX)-5, -12 and -15, as well as IL-6 and TNF-a. Recent findings indicate that COX-2, the inducible form of the COX isoenzymes, acts as a potent inducer of angiogenesis. Many botanical compounds are capable of acting as inhibitors of COX enzymes. More recently, substantial preclinical evidence demonstrated that COX-2 and LOX-5 inhibiting compounds have anti-angiogenic properties that open the possibility of using them for the treatment of angiogenesis-dependent diseases. Overstimulation of COX-2 creates inflammation, promotes pain, cancer, angiogenesis and cachexia (Kiefer and Dannhardt, 2004; Zha et al., 2004; Monnier et al., 2005).
Morphine, which is effective for cancer pain relief, elicits many adverse side effects. These effects include drug dependency, respiratory depression, decreased mental alertness, constipation and, most of all, a suppression of the “vital force,” which usually culminates in a sad ending to the person’s earthly life. The fundamental principle of co-author Donald Yance’s holistic, integrative approach, referred to as the Eclectic Triphasic Medical System (ETMS, discussed in the May NDNR), is to support the vital force as central to any protocol. Cancer patients with chronic pain need botanical support to build up their life force in order to have the energy to relieve pain and get well.
Panax ginseng extract exerts protective effects against morphine-induced depression and has shown an ability to potentiate the drug’s pain-relieving effect. P. ginseng extract supplementation could effectively reduce the dosage of morphine, which then would reduce the side effects. Several studies have shown P. ginseng extract to induce analgesia and inhibit the tolerance to analgesic drugs (Nemmani and Ramarao, 2002a, 2002b; Sengupta et al., 2004). Mumie (Shilajit), an adaptogen from Russia referred to as Mountain rock juice, has demonstrated an ability to prolong the analgesic effects of morphine (Tiwari et al., 2001). Shilajit in Sanskrit means ‘‘conqueror of mountains and destroyer of weakness.’’ (Schepetkin et al., 2002). Epimedium brevicornum has played a vital, multifaceted role in traditional Asian medicine for at least 1,000 years. Epimedium specifically increases bone mineralization and growth (Meng et al., 2005). In our view, adaptogenic formulas are central when forming a treatment protocol for cancer-related pain.
Vitamin D
Vitamin D (3000-4000IU) is essential in the treatment of bone metastasis and bone pain. Vitamin D prevents generalized and localized bone loss, and works well with bisphosphonates. Oral vitamin D supplementation alone, however, appears to be insufficient to prevent bone loss and bone pain in cancer patients. Intravenous (IV) therapy with potent nitrogen-containing bisphosphonates has shown promising efficacy (Saad et al., 2004).
Botanicals with an anabolic effect, such as Rhaponticum c., mumie, the extract pantocrine, and nutrients such as boron, vitamin D and whey protein concentrate, are essential components for outlining an effective protocol for the cancer patient with bone metastasis.
Vitamin K
In the past decade it has become evident that vitamin K has a significant role to play in human health that is beyond its well-established function in blood clotting. There is a consistent line of evidence in human epidemiologic and intervention studies that clearly demonstrates that vitamin K can improve bone health (Weber, 2001). Vitamin K plays a role in bone health, as bone gamma-carboxyglutamic acid (bone Gla) protein (the principle non-collagenous protein of bone, also called osteocalcin) and matrix Gla protein are dependent on vitamin K for their synthesis (Booth, 2000). In advanced stages of patients with bone metastasis and hypercalcemia, serum osteocalcin levels are increased, and vitamin K can help to reverse this. Vitamin K mediates the carboxylation of osteocalcin, helping to strengthen the bone. It also possesses anti-inflammatory as well as anti-cancer effects (Suzuki et al., 1989; Francini et al., 1988).
Neuropathic Pain
Any injury to the peripheral or central nervous system can cause neuropathic pain. This is often characterized by paroxysms of shock-like pain on top of a burning or constricting sensation. Neuropathic pain in patients with cancer commonly arises from a tumor invading or compressing the peripheral nerve, nerve plexus or spinal cord. It can occur as a result of surgery, radiation or chemotherapy as exemplified by post-mastectomy and post-thoracotomy syndromes, radiation-induced plexopathies and chemotherapy-induced neuropathies. Neuropathic pain can also accompany disorders that are unrelated to the tumor or its treatment, such as diabetes mellitus, nerve entrapment syndromes and herpes zoster (Martin and Hagen, 1997). See the accompanying list for some natural neuropathic pain relief options.
As we mentioned earlier, this is just a brief overview of some considerations when treating cancer pain. Botanical and nutritional approaches are a powerful, often underutilized ally that can greatly support patients with cancer. As NDs and preventive-oriented practitioners who believe in Primum Non Nocere, we owe it to our patients to educate ourselves in this growing field.
Natural Neuropathic Pain Relief Options
- Intravenous magnesium
- Specific B-vitamins such as B12, B1 and B6
- Folic acid
- Specific amino acid compounds, including glutamine (preferably as magnesium glutamine chelate) and acetyl-l-carnitine
- Lipoic acid
- High doses of the fatty acid compounds GLA and EPA/DHA
- Adaptogens, including Panax, Epimedium and Mumie
It is also helpful to treat blood deficiency when present. Anemia (both iron deficiency and bone marrow related), common in advanced cancer, can contribute to fatigue and pain. Blood-building and blood-moving herbs are important for the successful treatment of pain control.
Sources: Jaitly, 2003; Brill et al., 2002; Wang et al., 2005; Granados-Soto et al., 2004; Caram-Salas et al., 2004; Reyes-Garcia et al., 2004; Chiechio et al., 2004; Ghelardini et al., 2002; Braune, 2004; Hahm et al., 2004.
 Dicken Weatherby, ND is based in southern Oregon. A graduate of NCNM, Dicken is co-author of the bestselling book Blood Chemistry and CBC Analysis-Clinical Laboratory Testing from a Functional Perspective. He has self-published seven other books in the field of alternative medical diagnosis, has created numerous information products, and runs a number of successful Web sites (www.BloodChemistryAnalysis.com, www.Health-E-Marketing.com and www.StrawBale.com). He is involved in research, writing and consulting, and teaches functional diagnosis seminars in both the U.S. and his native country, the U.K.
Dicken Weatherby, ND is based in southern Oregon. A graduate of NCNM, Dicken is co-author of the bestselling book Blood Chemistry and CBC Analysis-Clinical Laboratory Testing from a Functional Perspective. He has self-published seven other books in the field of alternative medical diagnosis, has created numerous information products, and runs a number of successful Web sites (www.BloodChemistryAnalysis.com, www.Health-E-Marketing.com and www.StrawBale.com). He is involved in research, writing and consulting, and teaches functional diagnosis seminars in both the U.S. and his native country, the U.K.
 Donald Yance, CN, MH, RH is an internationally known herbalist and nutritionist. He is the founder and medical director of the Centre for Natural Healing in Ashland, Ore. Through extensive research and clinical practice, he has developed his Triphasic system, which forms the cornerstone of his clinical approach. Donald is the founder and formulator of Natura Health Products, and founder and president of The Mederi Foundation, whose programs promote health education and clinical research on the use of natural medicine, with an emphasis in the field of integrative oncology.
Donald Yance, CN, MH, RH is an internationally known herbalist and nutritionist. He is the founder and medical director of the Centre for Natural Healing in Ashland, Ore. Through extensive research and clinical practice, he has developed his Triphasic system, which forms the cornerstone of his clinical approach. Donald is the founder and formulator of Natura Health Products, and founder and president of The Mederi Foundation, whose programs promote health education and clinical research on the use of natural medicine, with an emphasis in the field of integrative oncology.
References
Twycross RG and Fairfield S: Pain in far-advanced cancer, Pain 14:303-310, 1982.
Cleeland CS: The impact of pain on the patient with cancer, Cancer 54:2635-2641, 1984.
Foley KM: The treatment of cancer pain, N Engl J Med 313:84-95, 1985.
Foley K: Supportive care and quality of life. In: DeVita VT Jr et al. (eds), Cancer: Principles and Practice of Oncology (6th ed). Philadelphia, 2001, Lippincott Williams & Wilkins.
Kiefer W and Dannhardt G: Novel insights and therapeutical applications in the field of inhibitors of COX-2, Curr Med Chem Dec;11(24):3147-61, 2004.
Zha S et al: Cyclooxygenases in cancer: progress and perspective (review), Cancer Lett Nov 8;215(1):1-20, 2004.
Monnier Y et al: Inhibition of angiogenesis by non-steroidal anti-inflammatory drugs: from the bench to the bedside and back, Curr Drug Targets Inflamm Allergy Feb;4(1):31-38, 2005.
Nemmani KV and Ramarao P: Role of benzodiazepine-GABAA receptor complex in attenuation of U-50,488H-induced analgesia and inhibition of tolerance to its analgesia by ginseng total saponin in mice, Life Sci 70(15):1727-40, 2002a.
Nemmani KV and Ramarao P: Ginseng total saponin potentiates acute U-50,488H-induced analgesia and inhibits tolerance to U-50,488H-induced analgesia in mice, Pharmacol Biochem Behav, May;72(1-2):1-6, 2002b.
Sengupta S et al: Modulating angiogenesis: the yin and the yang in ginseng, Circulation Sep 7;110(10):1219-25, 2004.
Tiwari P et al: Effects of Shilajit on the development of tolerance to morphine in mice, Phytother Res Mar;15(2):177-9, 2001.
Schepetkin I et al: Medical drugs from humus matter: Focus on mumie, Drug Dev Res Dec;57(3):140-159, 2002.
Meng FH et al: Osteoblastic proliferative activity of Epimedium brevicornum Maxim. Phytomedicine 2005 Mar;12(3):189-93, 2005.
Saad F et al: Skeletal morbidity in men with prostate cancer: quality-of-life considerations throughout the continuum of care, Eur Urol Dec;46(6):731-40, 2004.
Weber P: Vitamin K and bone health, Nutrition, Oct;17(10):880-887, 2001.
Booth S: Vitamin K and the skeleton. Proceedings of the 4th International Symposium on Nutritional Aspects of Osteoporosis, May 17-20, 2000. Lausanne, Switzerland. In: Burckhardt P et al. (eds), Nutritional Aspects of Osteoporosis. A Serono Symposia S.A. Publication. New York, 2000, Springer-Verlag.
Suzuki S et al: Clinical evaluation of serum osteocalcin in patients with bone metastasis of breast cancer [in Japanese], Nippon Gan Chiryo Gakkai Shi Oct 20;24(10):2386-93, 1989.
Francini G et al: Serum osteocalcin concentration in patients with prostatic cancer, Am J Clin Oncol 11 Suppl 2:S83-7, 1988.
Martin LA and Hagen NA: Neuropathic pain in cancer patients: Mechanisms, syndromes, and clinical controversies, J Pain Symptom Manage 14:99-117, 1997.
Jaitly V: Efficacy of intravenous magnesium in neuropathic pain, Br J Anaesth Aug;91(2):302, 2003.
Brill S et al: Efficacy of intravenous magnesium in neuropathic pain, Br J Anaesth Nov;89(5):711-4, 2002.
Wang ZB et al: Thiamine, pyridoxine, cyanocobalamin and their combination inhibit thermal, but not mechanical hyperalgesia in rats with primary sensory neuron injury, Pain Mar;114(1-2):266-77, 2005.
Granados-Soto V et al: Effect of diclofenac on the antiallodynic activity of vitamin B12 in a neuropathic pain model in the rat, Proc West Pharmacol Soc 47:92-4, 2004.
Caram-Salas NL et al: Antinociceptive synergy between dexamethasone and the B vitamin complex in a neuropathic pain model in the rat, Proc West Pharmacol Soc 47:88-91, 2004.
Reyes-Garcia G et al: Oral administration of B vitamins increases the antiallodynic effect of gabapentin in the rat, Proc West Pharmacol Soc 47:76-9, 2004.
Chiechio S et al: Metabotropic receptors as targets for drugs of potential use in the treatment of neuropathic pain, J Endocrinol Invest 27(6 Suppl):171-6, 2004.
Ghelardini C et al: Acetyl-l-carnitine induces muscarinic antinoci[c]eption in mice and rats, Neuropharmacology Dec;43(7):1180-7, 2002.
Braune S: Evidence-based pharmacotherapy of neuropathic pain syndromes [in German], MMW Fortschr Med Dec 9;146(50):49-51, 2004.
Hahm JR et al: Clinical experience with thioctacid (thioctic acid) in the treatment of distal symmetric polyneuropathy in Korean diabetic patients, J Diabetes Complications Mar-Apr;18(2):79-85, 2004.


