Student Scholarship Honorable Mention
Lidia Martyanova
Baljit Khamba, ND, MPH
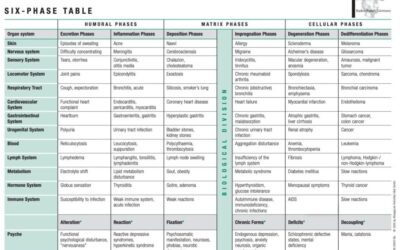
One of the major healthcare problems worldwide is excessive alcohol consumption. The liver is the target organ, since it is the primary site of ethanol metabolism. Excessive and chronic alcohol consumption leads to wide-spectrum, progressive hepatic lesions, ranging from steatosis to cirrhosis. Steatosis is the first physiological response to heavy alcohol drinking, and is characterized by fat deposition in hepatocytes. The next stage is typically progression to hepatitis, which is a more severe, inflammatory type of liver injury. The inflammation in hepatitis can cause fibrosis, and eventually cirrhosis if allowed to continue, which is characterized by excessive liver scarring, vascular alterations, and eventual liver failure.
The development of complications, such as ascites, variceal bleeding, hepatic encephalopathy, spontaneous bacterial peritonitis, or hepatorenal syndrome, has a significant impact on the prognosis of patients with alcoholic cirrhosis. The 5-year survival of individuals who develop any of these complications is only 20-50% of that for patients with compensated cirrhosis.1 Thirty-five percent of heavy drinkers develop end-stage alcoholic liver disease. Within 10 years of the diagnosis of cirrhosis, more than 50% of patients develop ascites. Mortality is 15% at 1-year follow-up and 44% at 5-year follow-up.1 The median survival of patients with ascites refractory to medical treatment is approximately 6 months. There are no FDA-approved pharmacological, supplemental, or nutritional therapies for patients with alcoholic cirrhosis. Hence, this article reviews a case report and the research we conducted on management options for such patients.
Management Options
Much research has been done on both pharmaceutical and nutritional agents that might be of use in patients with alcoholic cirrhosis. Nutritional research has focused primarily on the correction of nutritional deficiencies, such as the fat-soluble vitamins (A, D, E and K); folate, thiamine, niacin, and pyridoxine; and the trace elements zinc, magnesium, and selenium2; as well as on the treatment of abstinence syndrome. Micronutrient supplementation should be considered when deficiencies are detected. Multiple studies demonstrate the importance of zinc in liver disease.3-6 It has been shown that zinc blocks most mechanisms of liver injury, including increased gut permeability, oxidative stress, increased tumor necrosis factor (TNF) production, and hepatocyte apoptosis. Supplementation with 50 mg of elemental zinc could therefore be an effective means of improving liver function in patients with alcoholic liver disease.7
Pharmaceutical treatment options for more severe alcoholic hepatitis include corticosteroids and pentoxifylline, an anti-TNF therapy.8 The rationale for using steroids is their ability to suppress the immune response and proinflammatory cytokine response. Current guidelines suggest discontinuation of therapy if bilirubin levels have not decreased by Day 7 of treatment.9
Naturopathic treatments for alcoholic liver disease include a mixed-strain probiotic, which has been shown in studies to positively influence the gut microbiota, immunological status, and liver function in patients with liver disease.10,11 N-acetylcysteine (NAC), in combination with prednisolone, was shown in a randomized trial to reduce 1-month mortality (8% vs 24%) as well as the incidence of hepatorenal syndrome (9% vs 22%) and infection, compared to prednisolone alone.12 The favorable safety profile of NAC makes it a viable option, in combination with corticosteroids, for patients with severe disease.12 Silymarin (in milk thistle) has been shown in rats to protect against lipid peroxidation due to its antioxidant properties; it also has anti-inflammatory and anti-fibrotic effects.13 Although silymarin research has been conducted on animal models, it has been used to support liver function for decades. Finally, S-adenosylmethionine (SAMe) is a useful agent for these patients. SAMe is an obligatory intermediate in the conversion of methionine to cysteine in the hepatic transsulfuration pathway; it is also involved in the synthesis of polyamines, choline, and glutathione (GSH), and is the major methylating agent for a vast number of molecules via specific methyltransferases.14-17 In one randomized, multicenter trial, supplementation with SAMe was shown to delay liver transplantation and improve survival in patients with alcoholic liver cirrhosis.14
Case Description
KM, a 70-year-old female with decompensated alcoholic liver cirrhosis and refractory ascites, initially presented to Bastyr University Clinic in June 2017. Her height was 5 ft 7 in, and she weighed 201 lb (91 kg). However, her weight would be more accurately determined immediately following paracentesis.
KM is a retired loan officer who lives alone. She was an alcoholic for 40 years and quit just a few years ago. Cirrhosis was diagnosed in 2011, and fluid began building in her abdomen approximately 4 years ago. Family history was non-significant.
At the first visit, KM’s review of systems was positive for abdominal pain and constipation, leg swelling, skin rash, and insomnia. At the subsequent visit, 1 month later, she was positive for shortness of breath (SOB), bilateral lower-leg edema, dry cough every night and difficulty breathing when lying down, nasal drip for years, and difficulty walking due to her weight and SOB. By that visit, KM had experienced 7 paracenteses, with approximate fluid removal of 3.5-4 liters weekly. Her SOB and cough were most likely due to the volume of ascitic fluid.
Physical Exam
Physical examination revealed a blood pressure of 110/64 mm/Hg, temperature of 97.7°F, and pulse of 68. Bilateral edema was present on both legs (+3) and there was a notable absence of peripheral pulses – dorsalis pedis and posterior tibial. Auscultation revealed clear respiration in posterior fields, with no wheezing, rhonchi, or accessory muscle use upon respiration. Chest X-ray was unremarkable. KM’s abdomen showed severe ascites, a midline scar, and new stretch marks. Bowel sounds were present in all 4 quadrants. Her abdomen was dull to percussion. Hepatomegaly was present, and the right-upper quadrant was tender to palpation. Scratching on both forearms had produced an erythematous rash on her skin, consisting of multiple macules, 5-6 mm in diameter, variably shaped, and with random distribution on wrists and forearms.
The patient reported poor dietary habits. She usually had 2 meals per day, with large gaps in between. Her diet was characterized by poor nutritional variation and occasional wine consumption. This diet presentation is very common among patients with alcoholic liver disease, which is why nutritional corrections are an first essential step in patient management. KM’s labs was significant for liver failure, prediabetes, and iron deficiency. Diagnoses included alcoholic cirrhosis of the liver with ascites, prediabetes, and iron deficiency anemia.
Treatment Plan
KM’s medication list included furosemide 20 mg/day, along with the spironolactone 50 mg/day, to control her ascites. She was also taking oral lactulose 30 ml 3 times/day as needed to achieve 2-3 soft bowel movements.
Dietary corrections included: avoidance of huge gaps between meals; incorporation of low-glycemic index foods into the diet; sufficient protein intake (1.2-1.5 g/kg/day) but not overload (for controlling blood sugar and preventing hepatorenal syndrome).
Supplement recommendations included:
- Iron, for anemia
- A nutritional and botanical formula for hepatic and gastrointestinal detoxification (2 caps/day);
- Silybin with phosphatidylcholine (1 cap twice daily)
- A probiotic formula containing 8 different strains (1 cap 4 times daily)
- SAMe (1 cap twice daily), for liver function
- Melatonin (3 mg), for sleep
One Month Later
On the second follow-up visit, 1 month later, the patient reported that she had delayed her most recently scheduled paracentesis, and felt better overall. However, it is difficult to objectively assess the progression and effects of supportive treatments for patients in terminal stages of illness. Even though recent literature suggests that the median survival of patients with ascites refractory to medical treatment is approximately 6 months,18 we believe that supportive care can prolong a patient’s function and prevent rapid regression.
Summary
Although much knowledge has been gained in the understanding of the pathology, pathophysiology, epidemiology, and diagnoses of alcoholic liver disease, management options for a satisfactory outcome are still disappointing, and despite a large number of recent treatment trials, the ideal pharmacotherapy approach to alcoholic liver disease remains undefined. The development of complications in patients with alcoholic cirrhosis significantly impacts their prognosis. Once treatment-refractory ascites has developed, median survival drops precipitously. There are no FDA-approved pharmacological, supplemental, or nutritional therapies for patients with alcoholic cirrhosis. Because a naturopathic approach targets physiological function and treats the whole person, it is likely the only effective management option available for the patients with end-stage of alcoholic liver cirrhosis.
Most essential is supportive care and focus on abstinence and nutrition. Malnutrition is prevalent in liver disease, and the degree of malnutrition correlates with the development of serious complications such as encephalopathy, ascites, and hepatorenal syndrome. Research has shown that patients with chronic liver conditions are often deficient in several fat-soluble vitamins, B vitamins, and trace elements. Correction of these deficiencies is essential for restoring function.
Numerous natural agents, such as silymarin, NAC, SAMe, and probiotics have demonstrated efficacy in patients with alcoholic liver cirrhosis, and are all associated with favorable safety profiles. Perhaps the most promising areas for the future research and future clinical trials include gut microbes that target hepatic inflammation and infections through immune modulation, thereby promoting liver regeneration. Clinical trials on the use of all of these agents in human models are needed.
Most importantly, alcoholic liver disease is a preventable disease in the early stages, thus more efforts should be focused on prevention.
References:
- Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7(1):122-128.
- Halsted CH. Nutrition and alcoholic liver disease. Semin Liver Dis. 2004;24(3):289-304.
- Katayama K. Function of zinc in liver disease. [Article in Japanese] Nihon Rinsho. 2016;74(7):1126-11
- Grüngreiff K, Reinhold D, Wedemeyer H. The role of zinc in liver cirrhosis. Ann Hepatol. 2016;15(1):7-16.
- Sengupta S, Wroblewski K, Aronsohn A, et al. Screening for Zinc Deficiency in Patients with Cirrhosis: When Should We Start? Dig Dis Sci. 2015;60(10):3130-3135.
- Plotnikova EY, Baranova EN, Maksimov SA. Hepatic Encephalopathy And Tissue Zinc Levels In Liver Disease, Diagnosis And Treatment. [Article in Russian] Eksp Klin Gastroenterol. 2015;(7):46-54.
- Mohammad MK, Zhou Z, Cave M, et al. Zinc and liver disease. Nutr Clin Pract. 2012;27(1):8-20.
- Rosato V, Abenavoli L, Federico A, et al. Pharmacotherapy of alcoholic liver disease in clinical practice. Int J Clin Pract. 2016;70(2):119-131.
- European Association for the Study of the Liver. EASL clinical practical guidelines: Management of alcoholic liver disease. J Hepatol. 2012;57(2):399-420.
- Marlicz W, Wunsch E, Mydlowska M, et al. The effect of short term treatment with probiotic VSL#3 on various clinical and biochemical parameters in patients with liver cirrhosis. J Physiol Pharmacol. 2016;67(6):867-877.
- Dhiman RK, Rana B, Agrawal S, et al. Probiotic VSL#3 reduces liver disease severity and hospitalization in patients with cirrhosis: a randomized, controlled trial. Gastroenterology. 2014;147(6):1327-1337.e3.
- Nguyen-Khac E, Thevenot T, Piquet MA, et al. Glucocorticoids plus N-acetylcysteine in severe alcoholic hepatitis. N Engl J Med. 2011;365(19):1781-1789.
- Clichici S, Olteanu D, Nagy AL, et al. Silymarin inhibits the progression of fibrosis in the early stages of liver injury in CCl4-treated rats. J Med Food. 2015;18(3):290-298.
- Mato JM, Cámara J, Fernández de Paz J, et al. S adenosylmethionine in alcoholic liver cirrhosis: a randomized, placebo-controlled, double-blind, multicenter clinical J Hepatol. 1999;30(6):1081-1089.ew.
- Rambaldi A, Gluud C. S-adenosyl-L-methionine for alcoholic liver diseases. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD002235.
- Song Z, McClain CJ, Chen T. S-Adenosylmethionine protects against acetaminophen-induced hepatotoxicity in mice. Pharmacology. 2004;71(4):199-208.
- McClain CJ, Hill DB, Song Z, et al. S-Adenosylmethionine, cytokines, and alcoholic liver disease. Alcohol. 2002;27(3):185-192.
- Senousy BE, Draganov PV. Evaluation and management of patients with refractory ascites. World J Gastroenterol. 2009;15(1):67-80
 Lidia Martyanova came to the United States from Russia in 2011 in order to learn English and earn a degree in naturopathic medicine. She graduated from Bastyr University in the summer of 2018. Lidia completed her first medical degree in Russia, along with an internship in general practice and residency in gastroenterology. However, while working as a doctor in Russia, she felt that conventional medicine was missing many essential pieces, and she was drawn to naturopathic medicine philosophy and approach. Lydia has strong interests in gastroenterology, women’s health, children’s health, functional medicine, nutrition, naturopathic medicine, and naturopathic aesthetics.
Lidia Martyanova came to the United States from Russia in 2011 in order to learn English and earn a degree in naturopathic medicine. She graduated from Bastyr University in the summer of 2018. Lidia completed her first medical degree in Russia, along with an internship in general practice and residency in gastroenterology. However, while working as a doctor in Russia, she felt that conventional medicine was missing many essential pieces, and she was drawn to naturopathic medicine philosophy and approach. Lydia has strong interests in gastroenterology, women’s health, children’s health, functional medicine, nutrition, naturopathic medicine, and naturopathic aesthetics.
***
 Baljit Khamba, ND, MPH, is a licensed naturopathic doctor in California. Dr Khamba completed her (honors) Bachelor of Science degree (specializing in psychology), as well as her Masters in Public Health degree, at York University, in Toronto, Canada. She received her naturopathic doctoral degree from the Canadian College of Naturopathic Medicine (CCNM), also in Toronto. She was also involved with research projects at the University of Alberta on natural health product safety. Dr Khamba is a member of the American Osteopathic Association of Prolotherapy Regenerative Medicine.
Baljit Khamba, ND, MPH, is a licensed naturopathic doctor in California. Dr Khamba completed her (honors) Bachelor of Science degree (specializing in psychology), as well as her Masters in Public Health degree, at York University, in Toronto, Canada. She received her naturopathic doctoral degree from the Canadian College of Naturopathic Medicine (CCNM), also in Toronto. She was also involved with research projects at the University of Alberta on natural health product safety. Dr Khamba is a member of the American Osteopathic Association of Prolotherapy Regenerative Medicine.