Dr. Jennifer Bunzenmeyer, ND
Hormonal Cacophony: a Bloody Menses
Often, when I ask my clients if they have PMS, they jokingly respond, “you should ask my husband!” It is well accepted that women can be more “sensitive” around their menses but why? Although PMS is accepted as the “norm” in our society, to naturopathic doctors it points to an underlying imbalance in the body. Our job as clinicians is to investigate further and find a solution that brings equilibrium.
Merck manual says that 20-50% of women suffer from some form of premenstrual syndrome (PMS) with 5% suffering from severe premenstrual dysphoric disorder (PMDD). Symptoms occur 7-10 days prior to menses and can range from anxiety, irritability, anger, insomnia, mood dysregulation, depression, difficulty concentrating, fatigue, headaches, breast pain and edema. Other symptoms include nausea/vomiting, constipation, changes in appetite and acne. Eye conditions such as conjunctivitis or visual disturbances and respiratory concerns like allergies and infection can also occur. Symptoms are known to worsen during stress and peri-menopausal years. Diagnosis is through a report of consistent symptoms as there are no specific objective tests conventionally that define PMS. Merck manual reports lab tests and physical exam are not relevant.1
Underlying conditions such as migraines, asthma, epilepsy or herpes often present with onset of symptoms around the PMS time and should be ruled out and addressed first. Treating these conditions may alleviate the PMS symptoms.2 Depression and other mental health conditions (i.e. eating disorders, substance abuse), hormonal contraceptives and menopausal symptoms could also account for PMS symptoms as well. Hence, the need to treat the underlying disorder first to see if this could alleviate PMS symptoms.2
Etiology
Many theories have been speculated of why PMS occurs:
- Hormonal changes including:
- Estrogen and progesterone fluctuations1
- Increased aldosterone or ADH1
- Hyperprolactinemia1
- Hypoglycemia1
- Serotonin deficiency- medications like SSRI’s tend to help PMS and therefore show support for a serotonin deficiency etiology. 1
- Calcium and Magnesium deficiencies1
Let’s first look at the fluctuations of estrogen and progesterone that naturally occur in a woman’s menstrual cycle. Progesterone naturally begins to decrease prior to menses leaving women feeling more sensitive and emotional due to progesterone’s calming effect. If there is an imbalance between estrogen and progesterone, either estrogen being too high or progesterone too low, this can create enhanced PMS symptoms. For simplicity sake, it’s the balance of estrogen relative to progesterone.3 If there is low progesterone this can leave a symptomatic picture like spotting prior to menses, anxiety, insomnia, irritability, depression and hot flashes. Hence, the balance BETWEEN estrogen and progesterone are immensely important.3
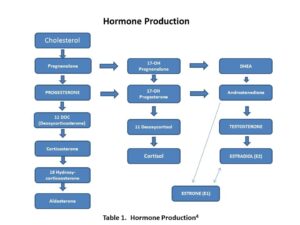
Although estrogen dominance has become a prominent phrase in the clinical world of treating hormone imbalances, this doesn’t entirely capture the whole aspect of hormone imbalance with respect to PMS and other women’s health issues. It is worth noting, hormonal balance comes from an orchestrated balance between many organs such as the hypothalamus, pituitary, ovaries, thyroid, liver and adrenals.4 As clinicians, our job is to look at the symptoms and objective testing and treat accordingly, keeping in mind this fine balance of organs in the hormonal orchestration.
Assessment: The Hormone Orchestration- what affects this fine balance?
| Low ProgesteroneSpotting prior to menses
Anxiety Insomnia Irritability Depression Hot flashes Infertility Miscarriages |
Estrogen DominanceAnxiety
Depression Brain Fog Food cravings Weight Gain Water retention Breast Tenderness Irregular Bleeding Cyclical Headaches/Migraines |
Estrogen Relative to Progesterone
As stated above, the most important aspect is how estrogen and progesterone are in relationship with one another. Estrogen dominance could be from a low progesterone level or a high estrogen level or an estrogen high RELATIVE to progesterone. Progesterone might be in normal levels but estrogen concentration may be high relative to progesterone, leaving an estrogen dominant picture. Or progesterone may be decreasing (common in peri-menopausal years) and therefore estrogen that is unopposed by progesterone acts as if it is at a higher level. To simplify- they work in tandem with each other.
Symptoms of estrogen dominance include symptoms of anxiety, depression, brain fog, food cravings, weight gain, water retention, breast tenderness, irregular bleeding and cyclical headaches or migraines. Conditions associated with high estrogen levels include uterine fibroids, endometriosis, amenorrhea, uterine cancer and decreased cognition. 4
Estrogen dominance can be caused from a variety of reasons. Exogenous estrogens from our environment such as xenoestrogens could be contributing to excess estrogen. Xenoestrogens are chemicals that are manmade and have an estrogenic effect in the body. Wildlife studies have shown now that some fish are even changing gender due to high levels of estrogens in our water sources.4 Other sources of xenoestrogens include fat-soluble estrogen from livestock or poultry, organochlorides, PCB’s, PVC’s – various man-made chemicals found in our households.4 High endogenous estrogen occurs with obesity as fat cells tend to hold onto estrogen. Lastly, our liver has to metabolize and break down the estrogen, therefore liver function needs to be optimal in order to do this.
Stress
When we are stressed, the stress hormones cortisol and adrenaline increase. Progesterone is a precursor hormone in the production of cortisol, hence with increased demand of stress hormones, lower progesterone levels may result.4 This theory supports the need to support the adrenal glands with various naturopathic therapies – adaptogenic herbs, nutritional supplementation and lifestyle modification (routine, dietary blood sugar balance and stress management). Stress can also affect a woman’s other hormones including testosterone, leading women to feel tired and sometimes a low libido.4 This demonstrates the need to look at all hormones and consider the whole orchestration of hormonal balance in PMS.
Nutritional Factors
Dietary factors can play a large role in producing PMS symptoms. A low nutrient diet full of junk food, fried foods, low fiber and few vegetables will not provide the nutrients to prevent PMS. Calcium and magnesium deficiencies are suspected in the etiology of PMS. Serotonin deficiency is also a suspected cause of PMS symptoms. Without sufficient protein in our diet, we are unable to attain the amino acid tryptophan, needed to produce serotonin. Lastly, blood sugar balance through diet is also needed to help with PMS symptoms such as anxiety, depression, insomnia and headaches.
Treatment Options
Addressing the Estrogen Dominant Picture
Exogenous Estrogens
Removing exogenous estrogens from the patient’s environment is critical. Advising patients as to where such chemicals occur, how levels build up in the body and how to remove them is essential.
Vitex Agnus (Chastetree)
Vitex has long been used in traditional medicine to treat PMS. It has a dopaminergic effect acting at the pituitary dopamine receptors (D2) which can help with breast pain in PMS when women have high prolactin levels.5
Another small multi-center, prospective, open-label, single-arm, phase 3 study showed promising results of Vitex. 69 patients received a 20 mg extract of Vitex agnus-castus over 3 menstrual cycles with patients recording their symptoms through a visual analog score (VAS). PMS symptoms evaluated and recorded included irritability, anger, depression, fatigue, drowsiness, sleeplessness, breast fullness, bloating, headache and skin disorder. There was a statistically significant reduction in the total VAS score (P<0.001) after the first menstrual cycle with this score continuing to decrease in the next two cycles. By the end of the third cycle, almost all patients had no symptoms or mild symptoms.6
Liver Nutrition to Help with Conjugation of Estrogen
Estrogen is conjugated through various pathways in the liver and various nutritional/herbal natural health products (NHPs) will help with this conjugation. Estrogen’s oxidative metabolism is mediated through the liver’s cytochrome p450 system. 2-hydroxylation of estrogens is induced by indole-3-carbinol (I3C), a nutrient found in cruciferous vegetables like broccoli and cabbage. In one study, I3C was given to 10 women for 2 months and 7 men for 1 week. Urinary samples were taken from individuals to monitor estrogen excretion through gas chromatography-mass spectrometry assessment. Results showed a significant increase in urinary excretion of C-2 estrogens.7 Hence, when looking at an estrogen excess picture, I3C or other NHPs that work on this pathway can help in balancing estrogen and progesterone through conjugation of the excess estrogen. When we decrease the body burden of estrogen, progesterone concentration relative to estrogen will increase and therefore symptoms of PMS will decrease. Although, this is just a theory (to my knowledge) and more research is needed on this. Anecdotally, I think we could agree that many of us naturopathic doctors, including myself, have seen this work for PMS clinically.
Traditional Chinese Medicine (TCM) Theory
From a Traditional Chinese Medicine (TCM) theory, we know the emotion of the liver is irritability and it is necessary for the liver energy to “run smoothly” prior to the menses cycle. If not, this can lead to a host of PMS symptoms including irritability and anger. We also know that, from a TCM perspective, our emotions/stress can impact the liver energy, supporting the observation that emotion affects the physical and vice versa.
With PMS symptoms, especially with irritability and mood fluctuations, I have seen time and time again where liver herbs like milk thistle, dandelion, globe artichoke, calcium-d-glucarate and I3C can really help. Many of my clients don’t want to go off their liver herbs!
Serotonin Imbalances and Stress
St. John’s Wort
It’s been known to have a serotonergic effect in the body, thus helping with conditions such as depression and anxiety. A RCT, double-blind controlled cross-over study involving 36 women who were diagnosed with PMS, were given either 900 mg of St. John’s Wort (standardized to 0.18% hypericin; 3.38% hyperforin) or placebo for two menstrual cycles. Cytokines (IL-1 beta, IL-8, interferon (IFN)-gamma and TNF-alpha) along with hormones (FSH, LH, estradiol, progesterone, prolactin and testosterone) were assessed in both the follicular and luteal phases in both groups. St. John’s Wort showed a statistically significant improvement in physical and behavioural symptoms such as food craving, insomnia, confusion, crying, fatigue, swelling, poor coordination and headaches (P<0.05). It, however, did not find a significant effect in mood and pain symptoms such as anxiety, impulsivity, depression and aggression.8,9
Rhodiola Rosea
This is primarily a central nervous system (CNS) adaptogenic herb. Rhodiola has been shown to influence neurotransmitters such as serotonin, norepinephrine and dopamine. It has been reported to prevent stress-induced depletion of catecholamines. Rhodiola is viewed as a herb to use for sleep disturbances due to physical or intellectual stress and also has been shown to decrease salivary cortisol levels.10 Rhodiola is a good candidate to supplement when a patient has a high-stress history, to prevent the decrease in progesterone levels through shunting into cortisol.
B-Vitamins
Vitamin B6, B12 and B3 are all needed as co-factors for serotonin production. A B-Complex supplement can be helpful in aiding serotonin production and as a support for stress.
Calcium, Magnesium and Vitamin D
In a small study of 62 students (31 PMS cases vs 31 controls), PMS participants showed a significant reduction in calcium and magnesium serum levels with a 19% and 14% respective increased risk in PMS for each unit decrease in calcium and magnesium serum levels. It was also noted that more than 1/3 of PMS cases were shown to be magnesium deficient. The above study also noted in their discussion that another study found there was a 61% decrease and 62% decrease in physical and psychological symptoms respectively of PMS when 1000mg of calcium was supplemented per day.11,12
Hence, addressing diet or adding supplementation to ensure adequate intake of calcium and magnesium is a baseline treatment strategy for PMS.
Conventional Medical Treatment
Conventional treatment involves lifestyle modification and exercise as first-line suggestions for treatment of mild to moderate PMS/PMDD.13
If pharmacotherapy is needed, SSRI’s such as fluoxetine, sertraline and paroxetine are top choices for PMDD and mood symptoms.13,14 Combined oral contraceptives are used for more physical symptoms of PMS.14 Anxiolytics, spironolactone and non-steroidal anti-inflammatory drugs can be used for symptomatic relief when needed.13
Summary
The hormone orchestration of PMS is an involved process that needs a thorough investigation on the clinician’s part to unwind the etiology and to work with these symptoms. With diligence and application of naturopathic principles supported by scientific evidence, naturopathic doctors have a diverse tool kit to help our patients.
References
- Pinkerton, J. Premenstrual syndrome (PMS). Merck Manual Professional Website. http://www.merckmanuals.com/professional/gynecology-and-obstetrics/menstrual-abnormalities/premenstrual-syndrome-pms. Last reviewed November 2015. Accessed August 2, 2016.
- Hudson, T. Pre-Menstrual syndrome; A Natural Approach. Tori Hudson, N.D. Blog [Internet]. October, 2006. [Acessed August2-15,2016]. Available from: http://drtorihudson.com/articles/premenstrual-syndrome-a-natural-approach/
- Nash, G. Rhythms & Regulations: Connections between Mood and Neuroendocrine Function [Webinar]. Seroyal International; 2016. Available from: seroyalcme.ca
- Pick, Marcelle. Estrogen Dominance- Is it Real? Women to Women-Health Library [Internet]. [Accessed August 2-15, 2016]. Available from: https://www.womentowomen.com/hormonal-health/estrogen-dominance/2/
- Wuttke W, Jarry H, Christoffel V, et al. Chastetree (Vitex agnus-castus)- Pharmacology and Clinical Indications. Phytomedicine. 2003;10(4):348-57.
- Momoeda, M, Sasaki H, Tagashira E, et al. Efficacy and safety of Vitex agnus-castus extract for treatment of premenstrual syndrome in Japanese patients: a prospective, open-label study. Ther. 2014;31(3):362-73.
- Michnovicz J, Adlercreutz H, Bradlow H L. Changes in Levels of Urinary Estrogen Metabolites after Oral Indole-3-Carbinol Treatment in Humans. J Natl Cancer Inst. 1997;89(10):718-723.
- Canning S, Waterman M, Orsi N, et al. The efficacy of Hypericum perforatum (St John’s Wort) for the treatment of premenstrual syndrome: a randomized, double-blind, placebo-controlled trial. CNS Drugs. 2010;24(3):207-25.
- Hudson, T. St. John’s Wort for treatment of Pre-Menstrual Syndrome (PMS). Dr. Tori Hudson, N.D. Blog [Internet]. May, 2010. [Accessed August 11,2016]. Available from: http://drtorihudson.com/botanicals/st-johns-wort-for-treatment-of-premenstrual-syndrome-pms/
- Head K, Kelly, G. Nutrients and Botanicals for Treatment of Stress: Adrenal Fatigue, Neurotransmitter Imbalance, Anxiety and Restless Sleep. Alt Med Rev. 2009;Vol.14, No. 2;114-140.
- Saeedian, K. Amani R., Cheraghian B. The Association between the Risk of Premenstrual Syndrome and Vitamin D, Calcium, and Magnesium Status among University Students: A Case Control Study. Health Promot Perspect. 2015; 5(3):225-30.
- Akhlaghi F, Hamedi A, Javadi Z, Hosseinipoor F. Effects of calcium supplementation on premenstrual syndrome. Razi Journal of Medical Sciences. 2004;10:669-675. [In Persian].
- Jarvis C, Lynch AM, Morin AK. Management strategies for premenstrual syndrom/premenstrual dysphoric disorder. Ann Pharmacother. 2008;42(7):967-78.
- Ryu A, Kim TH. Premenstrual syndrome: A mini review. Maturitas. 2015; 82(4):436-40.
 Dr. Jennifer Bunzenmeyer, ND is a registered Naturopathic Doctor, Medical Advisor, and consultant with over 1 1 years clinical experience in Calgary, AB. She is recognized highly in the women’s and mental health fields; having been interviewed in leading lifestyle magazines including Chatelaine, Alive, Fresh Juice and Avenue.
Dr. Jennifer Bunzenmeyer, ND is a registered Naturopathic Doctor, Medical Advisor, and consultant with over 1 1 years clinical experience in Calgary, AB. She is recognized highly in the women’s and mental health fields; having been interviewed in leading lifestyle magazines including Chatelaine, Alive, Fresh Juice and Avenue.
Having held a presidential position for a Toastmasters club, she speaks regularly for corporations, school boards and small businesses. She has excellent Clinic Management, Operational and Leadership experience in running a successful clinic. She is currently working towards her Professional Coaching Certification in order to assist clients and corporations achieve their best self.






















