Hilary Costello, ND
It was a beautiful spring day in Portland. My day at the office was filled with diverse and unique dermatology cases. One patient, Mrs. A (61 years old), accompanied by her friendly husband, presented with complaints of a lump on her back, previously diagnosed by her primary care physician as a lipoma. She was instructed to leave it alone and not worry about it unless it started to bother her. She explained that sleeping on her back and leaning back in chairs had become progressively more uncomfortable. She was seeking a second opinion and wanted “whatever it was” removed.
I took the case and attained all of the pertinent history. The lump had been steadily growing for two years and had become more noticeable as she slowly lost 25 pounds. She had a breast reduction two years ago and a history of cellulitis after the operation. She was being treated for benign hematuria, hypertension and depression with pharmaceuticals. There was no family history of lipomas or other skin abnormalities. Overall, the patient was in good health and had a positive outlook on life. The three of us spent some time getting to know each other while I prepared for the physical exam.
Giant Lipoma
I asked her to show me the area of concern. She turned around and lifted up her blouse to expose her back. I did not see it. I looked carefully and lifted her blouse higher to locate the area she was referring to. I asked her to point to the area and she said, “it’s just in the middle.” I placed my hand on her skin to palpate the area, and suddenly my field of awareness shifted. It was not the little lipoma I was searching for. I finally could see and feel the giant lump in her back. It was amazing for me because in my experience as a physician and student, I had never seen such a huge lipoma. My whole hand cupped over the area of the growth. The size reminded me of the bulge of a newborn’s head as it presses against the perineum before birth.
The lipoma’s location was slightly to the right of the spinal column on the posterior torso, approximately between T7 and T12, oriented toward the left at the superior border, measuring just more than 4 inches long and 3.7 inches wide. The lipoma palpated deep within the tissue. At the center, it measured 2 inches above the skin surface. The skin color, moisture, texture and turgor were all within normal limits. We located a few other superficial skin growths on her torso and face (nevus, skin tags and one small lipoma near the larger lesion) that we agreed should be removed due to tactile irritation and chronic sun exposure. Her vital signs were within normal limits.
We discussed the procedure, along with the alternatives and risks involved. I explained the excision procedure, anesthesia, suturing material and types, and the recovery period. I told her that I used botanical medicine during the surgery and a combination of homeopathics and botanicals for post-op treatment and aftercare for her to complete at home. She asked questions and we discussed the fact that many insurance companies do not cover NDs, despite our ability and license to perform in-office dermatological surgeries of this nature and complexity in Oregon.
She was interested in moving forward with the process and we scheduled the surgery a few weeks out. She and I established a rapport and relationship that allowed her to decide to pay my fees out of pocket instead of going to her dermatologist at the hospital, who could perform the same procedure. She felt more comfortable in the care of an ND because of our way of practicing medicine and the comfortable office setting. This type of scenario unfolds in my office frequently. Many of my patients are looking for a personable doctor in addition to the assurance of quality care, especially in the time of surgery. This is a driving force of my practice in dermatological surgery.
Over the next few weeks I prepared for this massive excision. I wanted to ensure that I could remove the lipoma in one piece. The complete excision of a lipoma is crucial because if a piece remains or if it becomes disintegrated in the process, the likelihood of it growing back dramatically increases. I was also concerned about the lipoma’s proximity to the spinal column, and its depth. I called on my closest surgery mentors to review the procedure and discuss potential complications. As the date approached, I felt confident about successfully performing the surgery.
Lipoma Removal
I instructed Mrs. A to discontinue her daily aspirin dose a few days before the surgery. She and her husband arrived at 9 a.m. We discussed the follow-up instructions and reviewed the informed consent paperwork. My assistant took her vitals: BP 138/88 RAS, 130/86 LAS, HR 74, RR 14, temperature 98.5F. I prepared the anesthesia in a 10cc sterile syringe (5cc lidocaine 2% with epinephrine 1:100,000, 5cc bupivacaine 0.25%) and used a 25-gauge 1.5-in needle for injection. During the procedure we prepared an additional 10cc syringe of the same formula.
As we prepared for the surgery, I spent a long time palpating the lipoma to identify the optimal incision line. In my mind I was reviewing Langer’s lines, gently pulling and pushing her skin around to find her unique lines of tension. As I had palpated at our first visit, the growth was firmly attached to the underlying tissue and the skin moved freely over the surface. I helped Mrs. A get comfortable in a prone position on the table with pillows and bolsters. I cleaned her skin with alcohol to remove any oil, and placed an adherent sterile fenestrated drape (3-in circular opening) over the lesion and established a sterile field. I cleaned the area three times with sterile iodine swabs. My initial ink line for the incision was 2.4 inches. I injected the anesthesia along the incision line, waited several minutes, and tested the area with the tip of the needle for sensitivity. I told Mrs. A that feeling pressure is normal, but to inform me of any sharp sensation during the procedure. She gave me the go ahead and I began.
I used a #10 sterile disposable scalpel to make the initial opening. The yellow fat layer was immediately visible and I thought I was at the surface of the lipoma due to the color and texture. It separated easily from the overlying epidermis by use of curved hemostats using standard undermining technique. I did this while thinking it would soon come out of her skin. After about 20 minutes I realized that the lipoma extended much deeper into her back and that I was not able to reach this area because of all of the adhesions. At this point I used my index finger to attempt to palpate the base of the lipoma with little success. I decided to make the incision longer, hoping to get to the bottom of the lipoma.
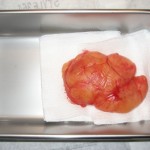
I expressed to Mrs. A and her husband, who was intently watching the entire procedure from the foot of the table, that I was not sure that I would be able to remove the lipoma because of the amount of adhesions and the depth. Incredibly, while saying that my index finger found its way to the bottom of the lipoma. It was located neatly in its capsule beneath the fat layer that I had been tediously working with. I quickly cut away the connective tissue that separated my tools from the lipoma. This took only seconds. Suddenly, the lipoma burst forth, completely encapsulated with an intact vascular system on its surface. The lipoma bulged out of the skin as the skin pulled tightly together beneath it at its base. It appeared like a pedunculated mushroom because of all of the adhesions at the base. Mrs. A’s husband, myself and my assistant were amazed at its size and appearance.
I knew I needed to work very fast, because the risk of infection increases each minute. I quickly lifted the lipoma and began to use the scalpel to release it from the underlying tissue. As I was maneuvering the lipoma, I realized that it was adhered to the paraspinal muscles. I carefully made cuts, detached the lipoma and placed it in a stainless steel container to prepare it for a biopsy sample.
There was an immense open space in Mrs. A’s back after the lipoma was removed. I used sterile saline to irrigate the tissues and placed two internal absorbable vertical mattress sutures to close up the space (vicryl 4.0). I decided to place a subcuticular suture (nylon 4.0) instead of simple interrupted sutures to minimize scarring. At each end of the subcuticular suture, I placed one simple interrupted suture for extra support (nylon 6.0). I treated the excision line with a minor surgery botanical formula consisting of Calendula officinalis succus, Hypericum canadensis, Centella asiatica and Echinacea spp. tinctures. I routinely use this formula for all surgeries. It is antimicrobial, supports healing and reduces scarring. Tincture of benzoin was placed parallel to the excision line on each side and five sterile adhesive strips were used. Three adherent sterile pads protected the area.
I instructed Mrs. A to use the botanical tincture topically 3-5 times per day for 14 days, when the sutures would be removed. I was clear with her that our communication in regard to pain or potential infection over the next 2 weeks was crucial. I told her to call me immediately if any signs or symptoms presented. One of my mentors recommended a prophylactic 10-day course of cephalexin 500mg BID due to the size and location of the lipoma, the procedure time and her age. Mrs. A and I discussed the potential risks and decided against the antibiotics because of the successful nature of the surgery.
I gave her Arnica 200C, 3 pellets qd x 3d to help with the bruising and bleeding. She tolerated the post-op “deep” pain with the help of acetaminophen with codeine (hydrocodone was not an option for her due to past drug reaction on file at her pharmacy). She had a high pain tolerance and was not interested in being heavily medicated for pain or discomfort.
When she left the office, I had the huge specimen, measuring 4.7 x 3.5 x 2.0 inches. I playfully looked at my tiny biopsy jars and wondered how I would make it fit. I decided to dissect a piece and submit it to the lab. After lab analysis, the pathologist reported a lesion composed of sheets of mature adipocytes with no evidence of malignancy, as we had expected.
Follow-Up
After two weeks I was excited to see the patient. Mrs. A’s healing was rapid, with no sign of infection, swelling or underlying tissue damage. Her skin was smooth and securely closed. At the appointment, Mrs. A reported that she was very happy with the surgery. She said that she had slept on her back for the first time in years. The surgery had positively affected her quality of life. When I saw her back, it was amazing. Her body had healed so quickly and the suture line after removal of the subcuticular stitch revealed minimal scarring.
I felt triumphant for our medicine, that we as NDs can serve our patients in new ways, expanding our specialized skills, applying our philosophy of medicine and pushing to expand our licenses in the U.S. I shared the tremendous feeling of success with my colleagues, and we experienced a ripple effect of new excitement for our medicine. These moments of shared enthusiasm and success are the guiding forces that will direct the future of naturopathic medicine.
 Hilary Costello, ND graduated from NCNM after receiving her BA in biology and fine arts painting from Sarah Lawrence College in New York. She practices in downtown Portland at Nature Cures Clinic (NatureCuresClinic.com) and Pearl MedSpa specializing in dermatology, minor surgery and pediatrics. Radiosurgery is one of her primary modalities and she has become an expert in this field. Her passions include medical and botanical illustrations/paintings, youth mentorship programs (MaidenSpirit.com) and humanitarian work for Ethiopia. Dr. Costello is the mother of three daughters, and she and her husband are avid organic gardeners.
Hilary Costello, ND graduated from NCNM after receiving her BA in biology and fine arts painting from Sarah Lawrence College in New York. She practices in downtown Portland at Nature Cures Clinic (NatureCuresClinic.com) and Pearl MedSpa specializing in dermatology, minor surgery and pediatrics. Radiosurgery is one of her primary modalities and she has become an expert in this field. Her passions include medical and botanical illustrations/paintings, youth mentorship programs (MaidenSpirit.com) and humanitarian work for Ethiopia. Dr. Costello is the mother of three daughters, and she and her husband are avid organic gardeners.