Kristina Conner, ND
Hydrotherapy, a cornerstone of classic naturopathic medicine and once recognized as a powerful healing tool in the days before the dominance of allopathic medicine, saw its heyday in the latter half of the 19th century. By the 1860s, it is estimated that there were more than 70 hydrotherapy centers in the U.S., primarily in New York and New England, and a co-educational hydropathic college in Manhattan. Women were an important part of this movement, including Mary Gove Nichols, Rachel Brooks Gleason and Harriet N. Austin. Women’s health issues were commonly treated using hydrotherapy because of the inclusion of women in the profession, the ease of home treatment, and the perilous treatment of women’s health issues from allopathic doctors. For instance, Benjamin Rush, noted physician and professor of medicine, proposed the theory that lack of menses during pregnancy necessitated venesection to both prevent and treat complications (Donegan, 1986), while influential obstetrician William Dewees recommended lead acetate douches, warm bathing and blood-letting for treatment of the common pregnancy complaint of “fluor albus,” vaginal leucorrhea. Given these options and the hazards of a rapidly industrializing society, it is no wonder that hygienic physicians had great success with hydrotherapy, vegetarian diets and outdoor exercise, with undeniably more satisfied patients.
History is pertinent to the current practice of naturopathic medicine because we are again facing a crisis in women’s healthcare and have something unique to offer. Of the 1.2 million women treated for uterine fibroids between 1998 and 2002 in the U.S., 84.4% received a hysterectomy and 12.3% received a myomectomy (Becker et al., 2005). Although the hysterectomy rate overall decreased between 1997 and 2005, the rate in 2005 was 5 per 1,000 women over age 18 (Merrill, 2008). For the ND, hydrotherapy offers a rational alternative to such extreme measures, since we have a simple, effective and accessible treatment: the sitz bath. This treatment can be used for a variety of ailments, from headaches to prostatitis. But this article focuses specifically on the sitz bath for use in gynecological conditions, highlighting it as one of the most effective and safest treatments in this arena.
Sitz Bath Therapies
The use of sitz baths is well recognized during the first stage of labor (Tournaire and Theau-Yonneau, 2007; Leeman et al., 2003) and the post-partum period (LaFoy and Geden, 1989; Ramler and Roberts, 1986), but there is less consideration for use during pregnancy. The hot sitz bath, as with any hot therapy, is contraindicated during pregnancy (Li et al., 2003), yet regular warm or cold baths can relieve pain while preparing for labor, as well as shorten its duration. Nichols used daily preparatory treatment of a wet sheet pack, 1-2 neutral sitz baths and cold enemas as needed, along with attention to diet, air and exercise (Donegan, 1986). For a less extensive protocol, we can look to Martin Luther Holbrook, a hydropathic doctor who recommended nightly neutral sitz baths with massage of the back and hips (Donegan, 1986).
There is a lack of recent research in the use of hydrotherapy for most conditions besides musculoskeletal complaints, especially in the U.S. and Canada, so we cannot base our protocols entirely on recent evidence using a diagnosis-based approach. Instead, it is useful to categorize these gynecological conditions into basic categories, which can then be related to older information. The four basic categories, and gynecological conditions associated with each, are:
- Spasmodic: dysmenorrhea, chronic pelvic inflammatory disease (PID)
- Excess/Inflammatory: cystitis, acute PID, vaginitis with pruritis, endometriosis
- Congestive: uterine fibroids, vaginitis without pruritis, amenorrhea, ovarian cysts
- Deficient/Prolapsed: prolapse, menometrorrhagia, enuresis
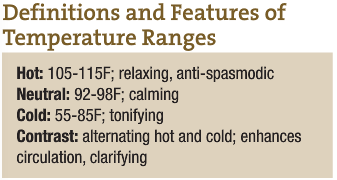
Most gynecological conditions will fall into one of the categories above; the treatment is then to use the appropriate type (temperature) of sitz bath. (See Definitions and Features of Temperature Ranges for details.) Spasmodic-type conditions will respond best to hot sitz baths; inflammatory conditions to neutral temperatures; and so forth. Length of treatment is determined by the type; cold sitz bath durations are shorter than hot or contrast; neutral sitz baths can last up to 2 hours for full effect. (See Procedures for sitz bath procedures.) Although safety is not well studied, when correct procedure is followed, sitz bathing is presumably safe. Debility is the only absolute contraindication to treatment; all other conditions need only to be assigned the correct therapy. For instance, acute PID is contraindicated in all types of sitz baths except the neutral sitz bath, for which it is indicated.
In many cases, more than one category could be considered, so a more complicated clinical assessment with often a more complicated sitz bath protocol will be needed to determine the underlying etiology. For instance, a woman with uterine fibroids, considered a congestive condition, eventually becomes deficient when this condition is prolonged, so she needs both contrast and cold sitz baths. In this instance, treatment could be separated: contrast sitz baths when there is no menstrual flow and cold sitz baths when there is excessive menstrual flow. This protocol is similar to that of Simon Baruch, a medical doctor who was prominent in the field of “scientific” hydrotherapy in the U.S., who used daily cold sitz baths from day 5 of the menses (or at the start of excessive bleeding if there was an irregular cycle) until bleeding ceased (Baruch, 1897).
Revisiting older protocols also sparks ideas about additions or changes to the treatments. For example, take the recommendations of Fox, a pioneer in the field of hydrology and the first editor of The Archives of Medical Hydrology. For vaginismus and dysmenorrhea, Dr. Fox used regular neutral baths. We could expect an additional effect from sedative herbs or Epsom salts. For congestive conditions like uterine fibroids, he recommended salt sitz baths, which we could also use, and sulphur sitz baths, which we would substitute with peloid or Epsom salts. We could also extend this protocol to other congestive pelvic conditions like polycystic ovarian syndrome, a condition not likely recognized in his time, or subfertility, a condition with growing incidence. For inflammatory conditions like endometriosis, or vaginitis with discharge, he used neutral to hot salt baths (Fox, 1914). Here our modern update would be the addition of peloid or antimicrobial herbs. In addition, we could add a general treatment to the protocol, such as constitutional hydrotherapy, which most modern patients would benefit from due to the higher degree of suppression and other detrimental effects of today’s lifestyle.
Obstacles and Advantages to Hydrotherapy
Since we have a wider range of therapies available, it is possible to create more individualized treatments, but there are some obstacles to using hydrotherapy in modern practice. First is the lack of availability of equipment and space for most NDs in private practice. It does take some dedication to using the therapy, especially because nutritional, herbal or other treatments work well and may be more accessible to a modern patient population. There may also be reluctance on the part of the patient to using a time-consuming, effort-intensive and sometimes uncomfortable protocol. Here we may follow the advice of Dr. Baruch, who found that, “Most women object strenuously to the cold hip bath … therefore, wise to forestall their fears by reassuring them of the necessity and great value of brief hip baths in these conditions” (Baruch, 1897). There is also the perception (among both patients and physicians) that hydrotherapy is old-fashioned, and therefore not applicable to current practice.
Alternatively, there are some distinct advantages of using hydrotherapy as a primary modality. Modifications can easily be made so that the treatments are more accessible. The sitz bath in particular is well-suited to home treatment, with proper patient instruction. Not only is hydrotherapy excellent for stimulating the Vis, the activity engages the patient in a unique way, making her accountable for the progress of care. A series of in-office treatments deepens and strengthens the physician-patient bond, the positive effects of which cannot be underestimated. And finally, even though the practice of gynecology may have changed and added new diagnoses, many of the underlying causes have not changed. A recent study confirms that the use of a traditional approach (acupuncture) as an adjuvant treatment to embryo transfer improves the success rate of pregnancy and live birth in women undergoing a technological approach – in vitro fertilization (Manheimer et al., 2008). Will we find that hydrotherapy may offer similar benefits in gynecological conditions, either as adjunct or primary treatment? By incorporating more of this foundational approach into naturopathic practice, we will be able to better answer that question.
Procedures
 Hot Sitz Bath
Hot Sitz Bath
- Prepare sitz bath. Add herbs or extracts as desired
- Water level: ½in below umbilicus
- Temperature: 105-115F
- Duration: 3-10 minutes
- Include a hot foot bath (105-115F). Finish hot foot bath with cold water poured over feet
- Apply cold compresses to forehead and back of neck
- Finish with cool sponging or spray to the pelvic area
- Dry patient and let rest for at least 30 minutes
Neutral Sitz Bath
- Water level: at umbilicus
- Temperature: 92-98F
- Duration: 15 minutes to 2 hours
- Hot foot bath optional
Cold Sitz Bath
- Water level: ½in below umbilicus
- Temperature: 55-75F
- Duration: 30 seconds to 8 minutes
Contrast Sitz Bath
- Prepare 2 sitz baths. Add herbs or extracts if desired
- Hot temperature: 105-115F for 2-5 minutes
- Water level: ½in above umbilicus
- Include a hot foot bath (110-115F)
- Apply cold compresses to forehead and back of neck during hot sitz bath
- Cold temperature: 55-85F for 20-60 seconds
- Water level: ½in below umbilicus
- Include a foot bath (105-110F)
- Repeat for 3 cycles total. Always finish with cold
- Ensure that the patient is covered and does not get chilled, especially during extended treatments
- A typical cycle would be 3 minutes hot, 30 seconds cold. Temperature and duration can be altered according to strength of the patient
Source: adapted from Lectures in Naturopathic Hydrotherapy
 Kristina Conner, ND graduated from Bastyr University in 2001. She completed her residency at the University of Bridgeport, College of Naturopathic Medicine. Dr. Conner is zealous about making classical naturopathic medicine pertinent to current practice. She is currently an assistant professor at NUHS, where she teaches, among other subjects, hydrotherapy.
Kristina Conner, ND graduated from Bastyr University in 2001. She completed her residency at the University of Bridgeport, College of Naturopathic Medicine. Dr. Conner is zealous about making classical naturopathic medicine pertinent to current practice. She is currently an assistant professor at NUHS, where she teaches, among other subjects, hydrotherapy.
References
Donegan J: “Hydropathic Highway to Health”: Women and Water-cure in Antebellum America. Westport, 1986, Greenwood Press.
Tournaire M and Theau-Yonneau A: Complementary and alternative approaches to pain relief during labor, Evid Based Complement Alternat Med 4(4):409-17, 2007.
Leeman L et al: The nature and management of labor pain: part 1. Nonpharmacologic pain relief, Am Fam Physician 68(6):1109-12, 2003.
LaFoy J and Geden EA: Postepisiotomy pain: warm versus cold sitz bath, J Obstet Gynecol Neonatal Nurs 18(5):399-403, 1989.
Ramler D and Roberts J: A comparison of cold and warm sitz baths for relief of postpartum perineal pain, J Obstet Gynecol Neonatal Nurs 15(6):471-4, 1986.
Li DK et al: Hot tub use during pregnancy and the risk of miscarriage, Am J Epidemiol 158(10):931-7, 2003.
Baruch S: The Principles and Practice of Hydrotherapy. New York, 1897, William Wood and Co.
Fox RF: Principles and Practice of Medical Hydrology. New York, 1914, William Wood and Co.
Manheimer E et al: Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta-analysis, BMJ 336(7643):545-9, 2008.
Boyle and Saine: Lectures in Naturopathic Hydrotherapy. East Palestine, 1988, Buckeye Naturopathic Press.

