Dr. Jaclyn Chasse, N.D
Today, changes in societal norms have led to couples, and women in particular, having children later in life. According to the CDC US National Vital Statistics Report from 2010, women over 40 are the only age group where birth rates are on the rise, increasing 6% between 2007 and 2009.1 Today, 2.6% of births are to women over 40. Certainly, there are increasing challenges with fertility in women over 40. The percentage of genetically normal eggs decreases to less than 10% in women over 40, and fertility rate (per month) declines to <5% in women in their 40s.1 The Southern California Center for Reproductive Medicine has reported an increasing miscarriage rate of 33% in women over 40 and >50% in women over age 45. While fertility can become challenged over 40, there are also benefits to conceiving in your 40s. Women who give birth after 40 have higher rates of college education, are more likely to read to their children, and do not experience the “motherhood penalty” of lost wages incurred by younger moms.2, 3, 4
In addition to fertility challenges, there can be higher risks to children born to older moms. The incidence of Down syndrome increases in women in their 40’s, as high as 1/12 births in women over 45 compared to 1/350 in women in their late 30s. The rates of autism are 50% higher in women over 40 compared to women aged 35-39.5 Higher rates of developmental delay and food allergies in women over 40 has also been reported.6
In older women, the total number of eggs in the ovarian pool declines and additionally, there is a decline in the percentage of genetically normal eggs, as mentioned above. Additionally, as age increases, the endometrial environment and cervical mucous change and there is an increased frequency of cycle abnormality. It is essential for naturopathic doctors to work with women considered (from a fertility perspective) to be of an “advanced age” in order to support their ability to get pregnant, to sustain a healthy pregnancy, and to support the health of the child.
When women over 40 are attempting to conceive, the most common concern is her ovarian reserve. The term ovarian reserve refers to a woman’s reproductive potential and includes factors such as the number and quality of oocytes, their fecundity (likelihood of achieving pregnancy), and their response to ovarian stimulation (both exogenous medications as well as endogenous hormone stimulation). Determination of ovarian reserve can be complicated, but is essential to evaluate to ensure what support may be necessary for the woman.
Historically, basal levels of follicle stimulating hormone (FSH) have been used to determine ovarian reserve. Measured on day 2,3, or 4 of the menstrual cycle, FSH <10 IU/L is indicative of optimal ovarian response. The low FSH value indicates that ovarian response is occurring. As the ovaries become less responsive to the signal from the pituitary, negative feedback of estradiol to the hypothalamus and pituitary decreases and FSH increases. This is seen most notably in menopause, where complete ovarian failure can be measured with an FSH often in the hundreds (See Table 1 for normal values of FSH). Scott et al reports 100% specificity for failure to achieve a live birth when FSH >18 IU/L, but at that high level, sensitivity of the test declines. This assay has high specificity (83-100%) predicting poor response to ovarian stimulation, but there is large inter and intra-cycle variability and there are different reference standards utilized in medical literature.7, 8, 9, 10 Basal estradiol measurement should be measured along with FSH, as an early rise in serum estradiol concentrations is a classic characteristic of reproductive aging and can also lower an otherwise elevated FSH into the normal range. If FSH is within the normal range but estradiol is elevated (>60-80 pg/mL) in the early follicular phase, this is associated with poor ovarian response and lower pregnancy rates11. Other tests including clomiphene citrate (Clomid) challenge tests, and antral follicle counts are also regularly used to measure ovarian response.
A serum marker rising in popularity to evaluate ovarian reserve is Anti-mullerian hormone (AMH). AMH is made by preantricle follicles (follicles in early development), and doesn’t fluctuate as much throughout the menstrual cycle. Optimal AMH levels are between 4.0 and 6.8 ng/mL (28.6-48.5 Pmol/L). Low fertility can be noted when AMH drops below 2.2 ng/mL (15.7 Pmol/L).
There are four leading theories explaining the changes in fertility seen with advancing age, all of which likely factor into the challenges observed in achieving pregnancy. These consist of declining ovarian androgens, mitochondrial defects, oocyte telomere shortening, and dysfunctional granulose cells as a result of exposure to oxidative and carbonyl stress.
It has been observed that there is an age-related decline in theca cell production of testosterone in women.12 Testosterone increases FSH receptor activity in ovaries, stimulates IGF-1 which may enhance oocyte metabolism and maturation, and improves granulosa cell health. There is a positive association of free androgen index and insulin sensitivity with follicle count after stimulation in women without PCOS and in non-obese women with PCOS as well as a correlation between higher levels of baseline testosterone and number of oocytes retrieved after adjusting for age, BMI, smoking status, and timing. Interestingly, women with PCOS tend to be better candidates for IVF with advanced age, possibly due to their higher testosterone compared to women without PCOS, and women with PCOS tend to preserve the ability to conceive later into life.13, 14
Therapeutically, treatments addressing testosterone have been studied and shown successful in improving fertility in women, including testosterone, DHEA, aromatase inhibitors such as Letrozole, low-dose LH administration, and growth hormone and IGF-1. Within naturopathic therapies, DHEA surfaces as the primary therapeutic used, at a dose of 25 mg three times daily15, 16. At this dose, DHEA has been shown to improve ovarian reserve, promote preantral follicle growth, increase pregnancy rates and lower miscarriage rates (in women over 35).17, 18 AMH rates will also respond to DHEA supplementation.19 To supplement this, you could consider including aromatase inhibiting compounds through diet including green tea, collard greens, grape seed extract and cabernet grapes.20
Mitochondrial changes are both the cause and effect of increased production of reactive oxygen species (ROS) and other toxic metabolic byproducts. Within the ovary, ROS play an important role and are necessary for ovulation to occur properly. ROS also initiate apoptosis of antral follicles. Older granulosa cells have a decreased capacity to mitigate ROS, measured through decreased levels of superoxide dismutase and glutathione. This decreased ability to fight free radicals, associated with advancing age, can lead to increased damage of ovarian lipids, proteins, and DNA.21, 22 In addition to oxidative stress, carbonyl stress plays a role in ovarian damage with age. Glycolysis creates endogenous reactive metabolites other than free radicals called reactive carbonyl species (RCS), and these metabolites can interact with proteins, lipids and DNA. These RCS can glycate proteins causing stable end products called advanced glycation end-products (AGEs) which damage proteins and impair enzyme function. These AGEs have been implicated in several chronic diseases, and can also build up in ovarian tissue leading to impairment in vascularization, cellular hypoxia, decreased cellular update of nutrients and increased oxidative stress. This can endanger follicle maturation and chromosomal integrity.23
Carbonyl and oxidative stress can be addressed through healthy plant-based diet with a focus on balanced blood sugar, exercise and targeted nutrition including intake of green tea and polyphenols.24, 25, 26 Additionally, specific antioxidants show promise in mitigating oxidative and carbonyl stress’ impact on fertility. Several studies have demonstrated the positive effect of melatonin (3mg/day) on fertility, including improved oocyte maturation, increased fertilization rates, and increased pregnancy rates in women taking melatonin while undergoing IVF.27, 28
Mitochondrial defects are the third contributing factor in ovarian aging. The oocyte has the highest number of mitochondria and mitochondrial DNA copies of any cell in the body (200,000 copies per cell; 1-2 orders of magnitude more than highly energy-dependant somatic cells like neurons or muscle cells).29 Nutrients which support mitochondrial function, such as CoQ10, show benefit in supporting fertility for both men and women. In ovarian tissue, CoQ10 deficiency can lead to impaired energy production, increased ROS production, increased lipid oxidation, and even cell death.30 Animal studies have demonstrated that supplementation with CoQ10 can increase follicular maturation and litter size. In humans, this can be supplemented orally (100-200 mg daily) or added to culture medium in IVF.31 In addition to CoQ10, r-alpha lipoic acid may also offer benefit in mitigating oxidative stress.32
The fourth theory of oocyte aging, telomere shortening, has less research associated with it, but we do know that telomere shortening occurs with every cell division, is dependant on genetic predisposition, and also increases as a result of exposure to ROS and genotoxins. Some cells compensate by expressing telomerase, such as stem cells, cancer cells, and male germ cells (leading to preservation of sperm health later into life). Follicles cannot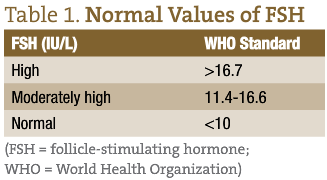 compensate, and telomere shortening may be a protective evolutionary adaptation to ensure the healthiest women reproduce.33
compensate, and telomere shortening may be a protective evolutionary adaptation to ensure the healthiest women reproduce.33
Additional nutrients to consider therapeutically to support oocyte health and fertility in women of advanced reproductive age include myo-inositol (4g daily) or d-chiro inositol (200-600 mg daily) as well as N-acetyl cysteine.34, 35, 36, 37 Additionally, all women attempting conception should be given a basic preconception protocol including a prenatal multivitamin, fish oil, and vitamin D.
With the increase in women attempting pregnancy over 35, it is imperative that every naturopathic physician have options to support optimal ovarian and oocyte health to improve fertility, achieve pregnancy sooner, and increase the health of the child.
 Dr. Jaclyn Chasse, N.D. is the Medical Director for Emerson Ecologics, and is also a practicing naturopathic doctor in New Hampshire focused on women’s health, infertility, and pediatrics. In 2012, Dr. Chasse was honored to be named Leading Physician in Alternative Medicine by NH Magazine. She is the immediate past-president of the New Hampshire Association of Naturopathic Doctors and currently serves on the Editorial Board of the Natural Medicine Journal as well as on the Boards of the AANP, the American Herbal Products Association and the Endocrinology Association of Naturopathic Physicians.
Dr. Jaclyn Chasse, N.D. is the Medical Director for Emerson Ecologics, and is also a practicing naturopathic doctor in New Hampshire focused on women’s health, infertility, and pediatrics. In 2012, Dr. Chasse was honored to be named Leading Physician in Alternative Medicine by NH Magazine. She is the immediate past-president of the New Hampshire Association of Naturopathic Doctors and currently serves on the Editorial Board of the Natural Medicine Journal as well as on the Boards of the AANP, the American Herbal Products Association and the Endocrinology Association of Naturopathic Physicians.
References
- US CDC National Vital Statistics Report 2010; 59(3).
- Southern California Center for Reproductive Medicine. Fertility and Age information. Available at: http://www.socalfertility.com/age-and-fertility/. Accessibility verified April 23, 2014.
- Gregory E. Ready: Why Women are Embracing the New Later Motherhood. New York. Basic Books 2007; 30.
- Pike MC, Pearce CL, Peters R, Cozen W, Wan P, Wu AH. Hormonal factors and the risk of invasive ovarian cancer: a population-based case-control study. Fertil Steril. 2004;82(1):186-95.
- Jayson S. Delaying kids may prevent financial ‘motherhood penalty’. USA Today. April 16, 2010.
- Shelton JF, Tancredi DJ, Hertz-Picciotto I. Independent and dependant contributions of advanced maternal and paternal ages to autism risk. Autism Research. 2010;3(1):30-9.
- Dioun AF, Harris SK, Hibberd PL. Is maternal age at delivery related to childhood food allergy? Pediatric Allergy and Immunology. 2003;14(4):307-11.
- Jayaprakasan K, Campbell B, Hopkisson J et al. Establishing the intercycle variability of three-dimensional ultrasonographic predictors of ovarian reserve. Fertil Steril. 2008 Dec’90(6):2126-32.
- Scott RT, Hofmann GE, Oehninger S, et al. Intercycle variability of day 3 follicle-stimulating hormone levels and its effect on stimulation quality in in vitro fertilization. Fertil Steril. 1990;54:297-302.
- Kwee J, Schats R, McDonnell J, et al. Intercycle variability of ovarian reserve tests: results of a prospective randomized study. Hum Reprod. 2004;19(3):590-5.
- Esposito M, Coutifaris C, Barnhart KT. A moderately elevated day 3 FSH concentration has limited predictive value, especially in younger women. Hum Reprod. 2002;17(1):118-123.
- Evers JL, Slaats P, Land JA, Dumoulin JC, Dunselman GA. Elevated levels of basal estradiol-17beta predict poor response in patients with normal basal levels of follicle-stimulating hormone undergoing in vitro fertilization.Fertil Steril. 1998;69(6):1010–1014.
- Dickerson EH, Cho LW, Maguiness SD, Killick SL, Robinson J, Atkin SL. Insulin resistance and free androgen index correlate with the outcome of controlled ovarian hyperstimulation in non-PCOS women undergoing IVF. Hum Reprod. 2010 Feb;25(2):504-9.
- Barbieri R, Sluss PM, Powers RD, McShane PM, Vitonis A, Ginsburg E, Cramer DC. Association of body mass index, age, and cigarette smoking with serum testosterone levels in cycling women undergoing in vitro fertilization. Fertil Steril. 2005;83(2):302-8.
- Holte J, Brodin T, Berglund L, Hadziosmanovic N, Olovsson M, Bergh T. Antral follicle counts are strongly associated with live-birth rates after assisted reproduction, with superior treatment outcome in women with polycystic ovaries. Fertil Steril. 2011 Sep;96(3):594-9.
- Barad D, Brill H, Gleicher N. Update on the use of dehydroepiandrosterone supplementation among women with diminished ovarian function. J Assist Reprod Genet. 2007 Dec;24(12):629-34.
- Wiser A, Gonen O, Ghetler Y, Shavit T, Berkovitz A, Shulman A. Addition of dehydroepiandrosterone (DHEA) for poor-responder patients before and during IVF . Hum Reprod. 2010 Oct;25(10):2496-500.
- Gleicher N, Barad DH. Dehydroepiandrosterone (DHEA) supplementation in diminished ovarian reserve (DOR). Reprod Biol Endocrinol. 2011 May 17;9:67.
- Gleicher N, Ryan E, Weghofer A, Blanco-Mejia S, Barad DH. Miscarriage rates after dehydroepiandrosterone (DHEA) supplementation in women with diminished ovarian reserve: a case control study. Reprod Biol Endocrinol. 2009 Oct 7;7:108.
- Gleicher N, Weghofer A, Barad DH. Improvement in diminished ovarian reserve after dehydroepiandrosterone supplementation. Reprod Biomed Online. 2010 Sep;21(3):360-5.
- Eng ET, Ye J, Williams D, et al. Suppression of estrogen biosynthesis by procyanidin dimmers in red wine and grape seeds. Cancer Res. 2003 Dec 1;63(23):8516-22.
- Devine PJ, Perreault SD, Luderer U. Roles of reactive oxygen species and antioxidants in ovarian toxicity. Biol Reprod. 2012 Feb 9;86(2):27.
- Matos L, Stevenson D, Gomes F, Silva-Carvalho JL, Almeida H. Superoxide dismutase expression in human cumululs oophorus cells. Mol Hum Reprod. 2009 Jul;15(7):411-9.
- Tatone C, Carbone MC, Campanell G et al. Female reproductive dysfunction during ageing: role of methylglyoxal in the formation of advanced glycation endproducts in ovaries of reproductively-aged mice. J Bil Regul Homeostat Agents. 2010 Jan-Mar;24(1):63-72.
- Peng X, Ma J, Chen F, Wang M. Naturally occurring inhibitors against the formation of advanced glycation end-products. Food Funct. 2011 Jun;2(6):289-301.
- Falone S, D’Alessandro A, Mirabilio A et al. Late-onset running biphasically improves redox balance, energy- and methylglyoxal-related status, as well as SIRT1 expression in mouse hippocampus. PLoS One. 2012;7(10):e48334.
- Rizzo P, Raffone E, Benedetto V. Effect of the treatment with myo-inositol plus folic acid plus melatonin in comparison with a treatment with myo-inositol plus folic acid on oocyte quality and pregnancy outcome in IVF cycles. A prospective, clinical trial. Eur Rev Med Pharmacol Sci. 2010 Jun;14(6):555-61
- Batioqlu A, Sahin U, Gurlek B, Ozturk N, Unsal E. The efficacy of melatonin administration on oocyte quality. Gynecol Endocrinol. 2012 Feb;28(2):91-3
- May-PanloupP, Chretien MF, Malthiery Y, Reynier P. Mitochondrial DNA in the oocyte and the developing embryo. Curr Top Dev Biol. 2007;77:51-83.
- Pignatti C, Cocchi M, Weiss H. Coenzyme Q10 levels in rat heart of different age. Biochem Exp Biol. 1980;16(1):39-42.
- Bentov Y, Yavorska T, Esfandiari N, Jurisicova A, Casper R. The contribution of mitochondrial function to reproductive aging. J Assist Reprod Genet. 2011 Sept;28(9):773-83.
- Gendelman M, Roth Z. Incorporation of coenzyme Q10 into bovine oocytes improves mitochondrial features and alleviates the effects of summer thermal stress on developmental competence. Biol Reprod. 2012;87:118.
- Kalmbach KH, Antunes DMF, Dracxler RC, Knier TW, Seth-Smith ML, Wang F, et al. Telomeres and human reproduction. Fertil Steril. 2013;99(1):23-9.
- Galletta M, Grasso S, Vaiarelli A, Roseff SJ. Bye-bye chiro-inositol- myo-inositol: true progress in treatment of polycystic ovary syndrome and ovulation induction. Eur Rev Med Pharmacol Sci. 2011 Oct;15(10):1212-4.
- Nestler J, Jakubowicz DJ, Reamer P, Gunn RD, Allan G. Ovulatory and metabolic effects of D-chiro inositol in the polycystic ovary syndrome. N Engl J Med. 1999 Apr 29;340(17):1314-20.
- Ciotta L, Stracquadanio M, Pagano I, Carbonaro A, Palumbo M, Gulino F. Effects of myo-inositol supplementation on oocyte’s quality in PCOS patients: a double blind trial. Eur Rev Med Pharmacol Sci. 2011 May;15(5):509-14.
- Liu J, Liu M, Ye X et al. Delay in oocyte aging in mice by the antioxidant N-acetyl-cysteine (NAC). Hum Reprod. 2012 May;27(5):1411-20.

