Larry Chan, DC, ND, R.Ac
A familiar life story: man retires at age 60 or 65 but begins to experience a lack of drive and interest in life’s activities. He exhibits grumpy behavior and withdraws into himself; he may even become depressed and display erratic moods. “Mid-life crisis? Depression? Or could it be a significant decline in the male hormone testosterone?
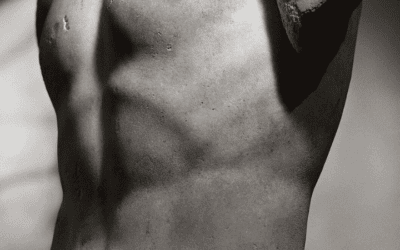
The root of the word is essentially a “pause/cessation” of “androgens”. Andropause is characterized by decreased testosterone levels associated with the normal aging process. The effect of male hormonal imbalance can be devastating with significant effect on how men look, feel and perform.
As many as 25–30 million men in North America between the ages of 35 and 70 are experiencing a phenomenon similar to female menopause called andropause. The decline in male hormone production is much more gradual than the decline in female hormone production. There is no significant event such as a cessation of the female menstrual cycle to mark the onset of andropause in males. A complex of physiological factors in the male usually results in a more urgent realization that they are indeed in a life transition at around the age of 50.
The onset of symptoms is gradual and can be vague, and are often accompanied by mood and attitude changes. Because of this they may be missed or disregarded as a form of depression.
Some common signs and symptoms of andropause include:
- Lack of energy
- Decreased physical strength and endurance
- Declining physical coordination and agility
- Loss of libido
- Decreased sexual performance
- Erectile dysfunction
- Decrease in ambition
- Decrease in work performance
- Weight gain (especially abdominal fat)
- Blood sugar elevation, increased insulin resistance
- Moodiness and depressed feelings
- Irritability, anxiety and loss of stress tolerance
- Increased aches and pains
- Diffuse sweating and hot flushes
- Cognitive decline (memory, concentration)
- Restlessness and insomnia
- Loss of self-esteem and altered state of well-being
- Dermatological changes (loose skin/wrinkles)
Factors that influence the decline of testosterone:
As part of the normal aging process, the body produces declining levels of testosterone after the mid-twenties. Unlike the relative predictable age of women’s menopause, men’s “transition” may be gradual over many decades (beginning in the mid-thirties). The testosterone decline is affected by multiple factors including genetics, nutrition, attitude, lifestyle, stress, alcohol, overall health, trauma, obesity, medications, infections and toxic load. The onset of andropausal symptoms of sufficient severity to lead an individual to seek medical help varies with age and the complex of influencing factors. The exact nature of each man’s symptoms, as well as the age of onset, is therefore highly variable.
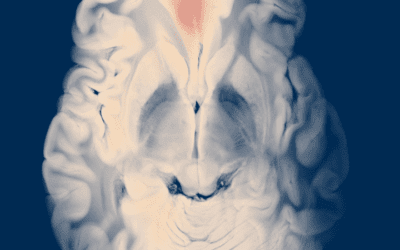
Hypogonadism can be primary or secondary. Primary hypogonadism is when the Leydig cells in the testes fail to secrete adequate levels of testosterone. Secondary hypogonadism occurs when there is a disruption of the hypothalamic–pituitary feedback for adequate Leydig cell stimulation by the pituitary hormone LH (luteinizing hormone). Normal aging factors and/or environmental influences can play a role in the development of hypogonadism.
Testosterone has many physiological benefits including enhancement of libido, increase in lean body mass, maintenance of strong bones, decrease of heart disease risk, lowering of LDL cholesterol and decreased insulin resistance. As men age the delicate balance between testosterone and estrogen may lean in favor of estrogen production. A relative high level of estrogen in the male may decrease the level of LH and therefore decrease testosterone production.
At one time, testosterone was thought to be beneficial only for younger men in terms of the associated masculine characteristics, and that for older men the increasing levels of the metabolite of testosterone, dihydrotestosterone (DHT), was associated with age-related male pattern baldness, and urinary and prostate disorders. The enzyme responsible for the conversion of testosterone to DHT, 5-alpha reductase, becomes more active with age, resulting in decreasing levels of testosterone with increasing levels of DHT. Much early clinical focus was therefore on blocking DHT through the use of 5-alpha reductase inhibition. This biochemical thrust has now been reassessed with more consideration given to the physiological effects of relative higher levels of circulating estrogens.
If testosterone levels are normal, and a man is experiencing signs of andropause, the problem may well be estrogen. Both men and women have a specific ratio of testosterone to estradiol. Young men have an average ratio of 50:1; the ratio drops with age as low as 8:1 in normal aging. The average 60-year-old male has more circulating estrogen in his bloodsteam than the average 60-year-old female. Higher estrogen levels may have many beneficial effects for menopausal women, but excess amounts in “andropausal” men may be catastrophic.
The conversion of testosterone to estradiol takes place under the influence of the enzyme aromatase. Testosterone can convert to estradiol; DHT does not. There is evidence that prostate health is related to the balance between levels of estradiol and DHT. Therefore a man with even a normal level of testosterone but with an increased estrogen level may in effect be andropausal due to the inhibiting effects of estrogen.
What are some common causes of elevated estrogen in men?
- Obesity: this can lead to high estrogen levels in both males and females. Adipose tissue contains aromatase and therefore results in higher conversion of testosterone to estradiol. Obesity lowers testosterone levels in all age ranges.
- Pharmaceutical drugs: many drugs can block testosterone production or accelerate the effects of aromatase. One example is the diuretic Lasix; this drug causes the loss of zinc stores and consequently reduced testosterone production.
- Zinc deficiency: zinc is a mineral essential for testosterone production. Zinc deficiency reduces the pituitary’s release of luteinizing and follicle stimulating hormone necessary for the stimulation of the Leydig cells for testosterone production. Zinc is also an inhibitor of aromatase.
- Stress and psychological factors: through the hypothalamus and other endocrine feedback loops, cortisol and other stress hormones can have a profound effect on testosterone production and metabolism.
- Liver function: a healthy liver is essential for elimination of toxins and the production and repair of all body systems; hormones, connective tissue and the organs themselves. An overburdened liver or diminished liver function can ultimately lead to altered endocrine balance.
- Alcohol consumption: aside from the obvious stress caused to the liver by alcohol consumption, prolonged alcohol abuse is associated with a higher level of body estrogen. Alcohol decreases zinc levels in the body. Heavy drinkers often exhibit related symptoms of gynecomastia and testicular atrophy.
- Increasing insulin resistance: altered sugar metabolism and elevated blood sugar can lead to obesity and a plethora of effects on body hormonal balance and altered tissue repair and organ dysfunction.
Long-term effects associated with andropause
Testosterone affects many metabolic functions in the body including the generating of red blood cells in bone marrow and osteogenesis. Prolonged diminished levels of testosterone may therefore result in osteoporosis and potential anemia. Other significant long-term effects include frailty due to loss of lean body mass; obesity and abdominal fat accumulation; increased cardiovascular disease risk; erectile dysfunction and emotional depression.
Therapeutic considerations
If diagnosed, andropause is very responsive to treatment with an integrative approach. Restoring the levels of bioavailable testosterone (free or unbound) is at the center of the treatment objective. This may involve prescribing testosterone itself in various forms and/or eliminating the identified factors that are inhibiting testosterone availability.
It is necessary to first assess the andropausal patient by performing a complete male hormonal analysis including free and total testosterone, DHT, sex hormone binding globulin (SHBG), estradiol, progesterone and PSA test for prostate, before a rational and effective treatment protocol can be devised.
Medical treatments include oral supplementation (testosterone undecanoate) taken daily and injectible forms (Depo-Testosterone Cypionate and Testosterone enanthate.) There are also bio-identical gels/creams as well as testosterone seed implants.
A thorough naturopathic assessment that integrates the parameters of toxic burden, organ health, diet and lifestyle, exercise (weight lifting increases testosterone levels), stress elimination and emotional health is essential in the successful management and treatment of the andropausal male.
References:
Ron Rothenberg MD & Kathleen Becker MA
Forever Ageless: published by California HealthSpan Institute
Eugene Shippen MD & William Fryer
The Testosterone Syndrome: published by M. Evans & Co. New York
Paul Yanick, Jr. PhD & Vincent Giampapa MD
Pro Hormone Nutrition: published by Longevity Institute International
Dr. Chan is a 1989 graduate of Canadian College of Naturopathic Medicine and received a Doctorate in Chiropractic Medicine from Canadian Memorial Chiropractic College in 1982. With a doctorate in Traditional Chinese Acupuncture, Dr. Chan is a registered acupuncturist in British Columbia. He is a diplomat of the American Academy of Anti-Aging Health Practitioners and the American College for Advancement of Medicine. As a founding partner, he practices at the Integrative Healing Arts Center, a large multidisciplinary clinic established in 1985 in Vancouver, B.C.; www.integrative.ca.