Kristen Haabala, ND
Mark Kaye, DC
Menopause is the clinical term used after menstruation has ceased for 1 year, after which women are considered postmenopausal.1 In the last 1 to 2 years before the final menstrual period, estrogen loss accelerates, and menopausal symptoms may become more pronounced. The age range for natural menopause is 40 to 58 years, with 51 being the median age for menopause in the Western world. An estimated 6000 American women transition to menopause every day.2 As life expectancy continues to extend, an unprecedented number of women will spend 30 to 35 years of their lives beyond menopause.
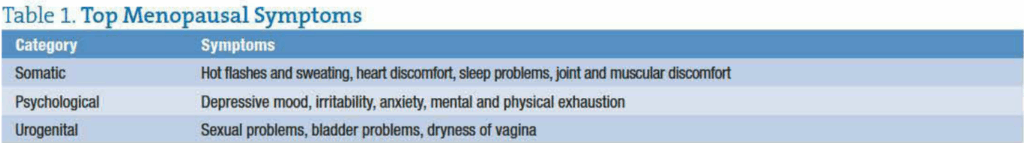
Menopausal symptoms typically fall into 3 categories (Table 1),3 with hot flashes being the most common and potentially debilitating. Nearly 80% of women in Western countries suffer from hot flashes, with 30% reporting hot flashes severe and frequent enough to seriously affect quality of life.4 Emerging research found that severity of hot flashes is associated with endothelial dysfunction, which contributes to early stages of atherosclerosis.5 The decline in estrogen during this transition also puts women at risk for multiple diseases and other functional abnormalities such as osteoporosis and cardiovascular disease.6,7
Hormone Replacement Therapy
Hormone replacement therapy (HRT), either with estrogen or estrogen plus progestin, is considered the most effective treatment option for relief of hot flashes and other menopausal symptoms.8 However, due to potential HRT-associated health hazards, women should consult with their physicians prior to HRT to determine whether potential benefits outweigh risks. Currently, the North American Menopause Society and the American College of Obstetricians and Gynecologists recommend using the lowest effective dose and for the shortest duration possible. Women over 60 years old who experienced natural menopause at a typical age and never used HRT are discouraged from doing so without compelling reasons.4 Women with a history of cardiovascular events, venous thromboembolism, breast or uterine cancer, or liver disease should not use estrogen to alleviate vasomotor symptoms.1
Other short-term pharmacological treatments for women unable or unwilling to use HRT include antidepressants (serotonin-norepinephrine reuptake inhibitor or selective serotonin reuptake inhibitor class), an anticonvulsant agent (gabapentin), and antihypertensive medication (clonidine). However, these drugs have not been approved by the Food and Drug Administration for relief of vasomotor symptoms, and all have potential adverse effects.1
Phytoestrogens, the Most Popular Natural Approach
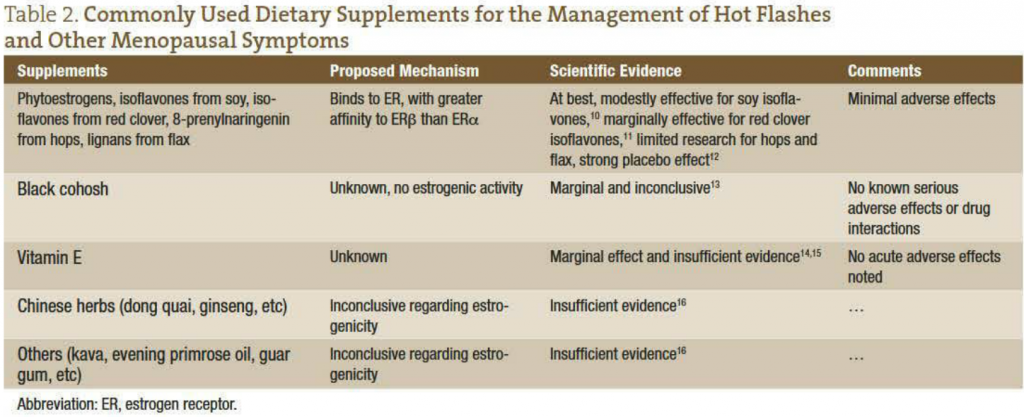
It comes as no surprise that women are actively seeking out “natural” approaches such as herbal remedies for treating hot flashes (Table 2). The most popular category, and the most studied, is phytoestrogens, plant substances found in soy, red clover, flax, hops, and other sources that possess weak estrogenic activity by binding to estrogen receptors (ERs). Phytoestrogens appear to have higher affinity to ERb (mainly expressed in nonreproductive tissues such as cardiovascular system and brain) than to ERa (mainly expressed in uterus, hypothalamus, bone, and other classical estrogen target tissue), but their potencies are much weaker than that of estrogen.9 Systematic review of literature found that phytoestrogens such as isoflavones, lignans, and 8-prenylnaringenin have, at best, only modest effect in ameliorating hot flash number, frequency, and intensity, as well as other menopausal symptoms. Nonphytoestrogen remedies include black cohosh, vitamin E, and various Chinese herbs. Their mechanisms of action remain to be elucidated. While the benefits of black cohosh preparations remain controversial, other remedies lack sufficient clinical evidence to support their use in managing menopausal symptoms.
A Phytoestrogen Like No Other
In Germany, where research on herbal relief for menopausal symptoms has been conducted and widely prescribed since the 1940s, clinicians have been recommending a proprietary and standardized extract from the root of Siberian rhubarb (Rheum rhaponticum) since 1993. The main constituents of this extract are hydroxystilbenes, including rhaponticin, desoxyrhaponticin, rhapontigenin, and desoxyrhapontigenin.17 Unlike other medicinal rhubarb species such as Chinese rhubarb plant (Rheum palmatum or Rheum officinale), Siberian rhubarb root extract does not contain anthraquinones (eg, emodin and rhein), which not only have a laxative effect but may also increase the risk of unwanted adverse effects in the breast and endometrium, possibly related to activation of ERa.
Clinical trials (summarized in Table 3) have demonstrated that 1 tablet (4 mg) daily of the Siberian rhubarb root extract offers significantly effective relief vs placebo for the 11 most common menopausal symptoms, including hot flashes. Participating women have reported symptom reduction that continues over 3, 6, 12, and 24 months to help improve quality of life through additional improvements in sleep quality and reduced anxiety and depression.

These clinical data consistently show that the proprietary Siberian rhubarb root extract is safe and well tolerated both in short-term and long-term studies. No serious adverse events have been associated with intake, and no clinically relevant changes in endometrial biopsies, bleeding, weight, blood pressure, pulse, or other standard laboratory variables have been observed in these studies17-21 with hundreds of patients.
The proprietary Siberian rhubarb root extract does not contain estrogen but appears to be a selective ERb agonist based on in vitro data.17 Estrogen receptor b, which mediates the anxiolytic and antidepressant effects of estrogen, has been suggested to alleviate menopausal symptoms, including depression and anxiety. Research suggests that ERb negatively regulates ERa in tissues that express both receptors and may therefore protect against ERa-mediated effects in the breast and endometrium.22,23 This targeted influence on ERb may explain why clinical evidence supports its effectiveness and safety.
Healthy Lifestyle Choices for Menopause Miseries
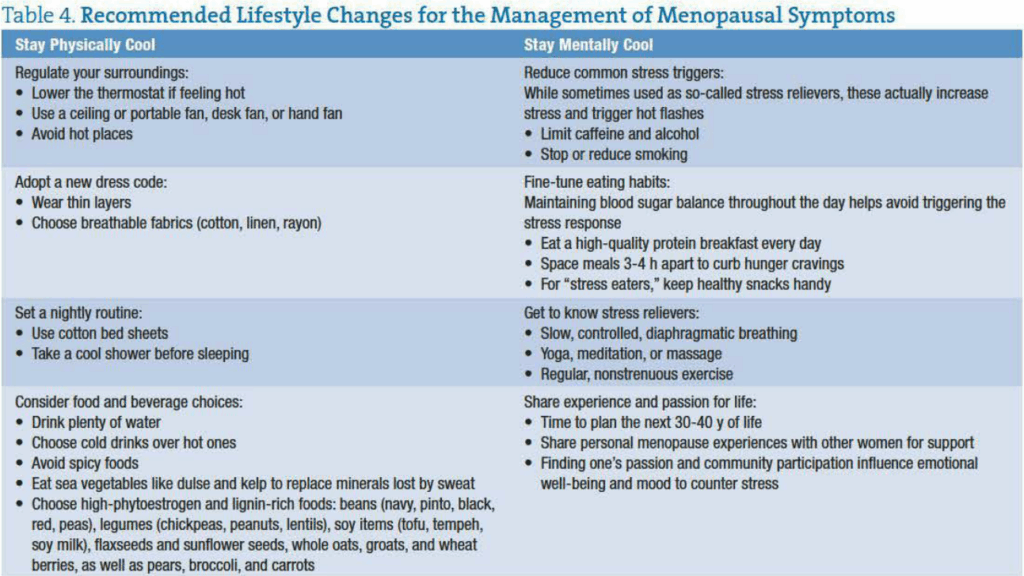
Lifestyle changes, including regulation of core body temperature, relaxation techniques, regular physical activity, weight loss, and smoking cessation, may help reduce the risk of vasomotor symptoms and should be implemented by all women with symptomatic menopause. Recommended lifestyle changes are summarized in Table 4.
New “Cool Kid” on the Block
The proprietary Siberian rhubarb root extract has been used in Germany since 1993. Recent clinical trials have consistently demonstrated its efficacy in reducing hot flashes and other menopausal symptoms, whereas investigations of other natural remedies indicate inconsistent results and ambiguous efficacy. Unlike HRT, the extract does not contain estrogen or very potent activators of ERs and remains effective and safe in long-term treatment. This new “cool” kid on the block, used in conjunction with personalized lifestyle changes, should offer positive clinical outcomes for women in various stages of menopausal transition.
Acknowledgment
We thank Dr Jyh-Lurn Chang and Lyra Heller for manuscript preparation.
 Mark Kaye, DC is the Director of Clinical Services at Metagenics. He has been at Metagenics for 17 years, engaging in a variety of educational responsibilities including national and international speaking tours, regional training program, and professional re-licensing programs. In addition, he is actively engaged in research & development, education, training, and clinical protocol and product support for practitioners. Prior to joining Metagenics, Dr Kaye practices as a clinician in a private practice setting for 9 years, holding prior licensure in Arizona, California, and the state of Maine. Dr Kaye is a graduate of the Los Angeles College of Chiropractic in Whittier, California, holding a Bachelor of Science in biology and an undergraduate degree in chemistry.
Mark Kaye, DC is the Director of Clinical Services at Metagenics. He has been at Metagenics for 17 years, engaging in a variety of educational responsibilities including national and international speaking tours, regional training program, and professional re-licensing programs. In addition, he is actively engaged in research & development, education, training, and clinical protocol and product support for practitioners. Prior to joining Metagenics, Dr Kaye practices as a clinician in a private practice setting for 9 years, holding prior licensure in Arizona, California, and the state of Maine. Dr Kaye is a graduate of the Los Angeles College of Chiropractic in Whittier, California, holding a Bachelor of Science in biology and an undergraduate degree in chemistry.
 Kristen Haabala, ND received her doctorate in Naturopathic Medicine from the National College of Natural Medicine (Portland, Oregon). Prior to attending NCNM, Kristen received her bachelor’s degree in Biomedical Science from St. Cloud State University. Additional post-doctorate education includes training in the areas of Functional Medicine, Frequency Specific Microcurrent, and Lifestyle Medicine with certification as a First Line Therapy health care practitioner. She completed her residency work under Dr Kristi Hughes. Dr Haabala is now the owner of Midwest Natural Medicine in Alexandria, Minnesota. Her practice is focused on educating patients on the power of living a healthy lifestyle, offering natural healthcare solutions to today’s complicated medical conditions. She strives to create a personalized treatment program for each patient with a supportive environment for improving holistic health.
Kristen Haabala, ND received her doctorate in Naturopathic Medicine from the National College of Natural Medicine (Portland, Oregon). Prior to attending NCNM, Kristen received her bachelor’s degree in Biomedical Science from St. Cloud State University. Additional post-doctorate education includes training in the areas of Functional Medicine, Frequency Specific Microcurrent, and Lifestyle Medicine with certification as a First Line Therapy health care practitioner. She completed her residency work under Dr Kristi Hughes. Dr Haabala is now the owner of Midwest Natural Medicine in Alexandria, Minnesota. Her practice is focused on educating patients on the power of living a healthy lifestyle, offering natural healthcare solutions to today’s complicated medical conditions. She strives to create a personalized treatment program for each patient with a supportive environment for improving holistic health.
References
Nelson HD. Menopause. Lancet. 2008;371:760-770.
North American Menopause Society. Overview of menopause and aging. http://www.menopause.org/docs/2012/cg_a.pdf?sfvrsn=2 Accessed October 15, 2012.
Heinemann K, Ruebig A, Potthoff P, et al. The Menopause Rating Scale (MRS) scale: a methodological review. Health Qual Life Outcomes. 2004;2:45. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC516787/. Accessed October 15, 2012.
Umland EM. Treatment strategies for reducing the burden of menopause-associated vasomotor symptoms. J Manag Care Pharm. 2008;14:14-19.
Bechlioulis A, Naka KK, Papanikolaou O, Kontostolis E, Kalantaridou SN, Michalis LK. Menopause and hormone therapy: from vascular endothelial function to cardiovascular disease. Hellenic J Cardiol. 2009;50:303-315.
Eaker ED, Chesebro JH, Sacks FM, Wenger NK, Whisnant JP, Winston M. Cardiovascular disease in women. Circulation. 1993;88:1999-2009.
Khosla S. Update on estrogens and the skeleton. J Clin Endocrinol Metab. 2010;95:3569-3577.
North American Menopause Society. The 2012 hormone therapy position statement of: the North American Menopause Society. Menopause. 2012;19:257-271.
Sunita P, Pattanayak SP. Phytoestrogens in postmenopausal indications: a theoretical perspective. Pharmacogn Rev. 2011;5:41-47.
North American Menopause Society. The role of soy isoflavones in menopausal health: report of the North American Menopause Society/Wulf H. Utian Translational Science Symposium in Chicago, IL (October 2010). Menopause. 2011;18:732-753.
Coon JT, Pittler MH, Ernst E. Trifolium pratense isoflavones in the treatment of menopausal hot flushes: a systematic review and meta-analysis. Phytomedicine. 2007;14:153-159.
Lethaby AE, Brown J, Marjoribanks J, Kronenberg F, Roberts H, Eden J. Phytoestrogens for vasomotor menopausal symptoms. Cochrane Database Syst Rev. 2007:CD001395.
Palacio C, Masri G, Mooradian AD. Black cohosh for the management of menopausal symptoms: a systematic review of clinical trials. Drugs Aging. 2009;26:23-36.
Barton DL, Loprinzi CL, Quella SK, et al. Prospective evaluation of vitamin E for hot flashes in breast cancer survivors.
J Clin Oncol. 1998;16:495-500.
Ziaei S, Kazemnejad A, Zareai M. The effect of vitamin E on hot flashes in menopausal women. Gynecol Obstet Invest. 2007;64:204-207.
North American Menopause Society. Treatment of menopause-associated vasomotor symptoms: position statement of the North American Menopause Society. Menopause. 2004;11:11-33.
Heger M, Ventskovskiy BM, Borzenko I, et al. Efficacy and safety of a special extract of Rheum rhaponticum (ERr 731) in perimenopausal women with climacteric complaints: a 12-week randomized, double-blind, placebo-controlled trial. Menopause. 2006;13:744-759.
Kaszkin-Bettag M, Ventskovskiy BM, Kravchenko A, et al. The special extract ERr 731 of the roots of Rheum rhaponticum decreases anxiety and improves health state and general well-being in perimenopausal women. Menopause. 2007;14:270-283.
Hasper I, Ventskovskiy BM, Rettenberger R, Heger PW, Riley DS, Kaszkin-Bettag M. Long-term efficacy and safety of the special extract ERr 731 of Rheum rhaponticum in perimenopausal women with menopausal symptoms. Menopause. 2009;16:117-131.
Kaszkin-Bettag M, Beck S, Richardson A, Heger PW, Beer AM. Efficacy of the special extract ERr 731 from rhapontic rhubarb for menopausal complaints: a 6-month open observational study. Altern Ther Health Med. 2008;14:32-38.
Kaszkin-Bettag M, Ventskovskiy BM, Solskyy S, et al. Confirmation of the efficacy of ERr 731 in perimenopausal women with menopausal symptoms. Altern Ther Health Med. 2009;15:24-34.
Frasor J, Barnett DH, Danes JM, Hess R, Parlow AF, Katzenellenbogen BS. Response-specific and ligand dose–dependent modulation of estrogen receptor (ER) a activity by ERb in the uterus. Endocrinology. 2003;144:3159-3166.
Lindberg MK, Moverare S, Skrtic S, et al. Estrogen receptor (ER)-b reduces ERa-regulated gene transcription, supporting a “ying yang” relationship between ERa and ERb in mice. Mol Endocrinol. 2003;17:203-208.






















