A Multifactorial Approach
John Reynolds, ND
 It is an interesting phenomenon that sexual dysfunction has become one of the major reasons why male patients visit their primary care provider. In the past, men seemed determined to remain silent about these private and personal matters. If nothing else, we can thank sildenafil citrate for opening the door to this discussion. Men represent about 90% of my practice, and at least 30% to 40% of them experience low libido or erectile dysfunction (ED). Most patients want an easy fix to their problem in the bedroom. Unfortunately, it is often a multifactorial problem, and a whole-body approach is usually necessary.
It is an interesting phenomenon that sexual dysfunction has become one of the major reasons why male patients visit their primary care provider. In the past, men seemed determined to remain silent about these private and personal matters. If nothing else, we can thank sildenafil citrate for opening the door to this discussion. Men represent about 90% of my practice, and at least 30% to 40% of them experience low libido or erectile dysfunction (ED). Most patients want an easy fix to their problem in the bedroom. Unfortunately, it is often a multifactorial problem, and a whole-body approach is usually necessary.
Erectile dysfunction is defined as the inability to start or maintain an erection 75% of the time.1 This definition was formulated to expand the spectrum of what was once simply called impotence. The stigma of impotence became associated with not only the loss of function but also the loss of something that defined us as men. Men who experienced this would often spend years in denial, with strong feelings of guilt and shame.
What we now know is that ED is common in our society. In a study2 from the Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, it was estimated that more than 18 million men, or approximately 18% of men in the United States, experience ED. The study evaluated 2126 men who participated in the National Health and Nutrition Examination Survey. Erectile dysfunction was defined in the study as “sometimes being able” or “never being able” to get or maintain an erection. In all probability, this issue is severely underreported. In addition, the prevalence of ED increases after age 40 years. In his book Vital Man: Natural Healthcare for Men at Midlife, herbalist Stephen Harrod Buhner3 estimates the incidence to be closer to 30 million cases.
As mentioned before, the origin of ED is multifactorial and is often surprising to our patients. The causes usually include a combination of psychological, pharmacological, vascular, neurological, and hormonal issues. To our patients’ surprise, rarely is the issue simply one of low testosterone level. In one study4 only 29% of 422 men with ED had hormonal deficiencies, and hypogonadism (primary and secondary) accounted for only 19% of the cases. In another study5 of 1022 men, only 4% of men younger than 50 years and 9% of men 50 years or older showed low serum levels of testosterone.
3 Risk Factors
The 3 most important risk factors for developing ED are medication use, cardiovascular disease, and diabetes mellitus. In my practice, antidepressants are the most common class of medications that contribute to ED symptoms. It is not surprising that ED rates seem to have increased since the introduction of fluoxetine in the 1980s. In my practice, if a patient is taking this class of medication, I always discuss its use as a potential obstacle to cure. This is not to say that I immediately separate patients from their antidepressants, but I inform them that this may be the cause of some or all of their symptoms. In addition, ED is thought to be a major adverse effect of many other drugs, including diuretics, antihypertensives, antiseizure medications, antihistamines, muscle relaxants, cancer and chemotherapy drugs, and even nonsteroidal anti-inflammatory drugs. In a 2011 study6 published in the Journal of Urology, nonsteroidal anti-inflammatory drug use was found to be positively correlated with increases in ED.
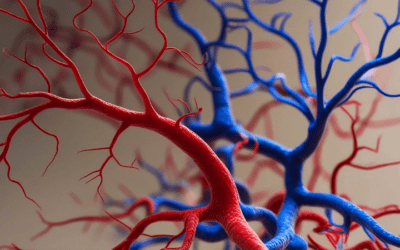
The second 2 most important risk factors for developing ED are related to our lifestyle and diet. Cardiovascular disease and diabetes are associated with our standard American diet and inactivity. Vascular health is an important factor in treating ED. To initiate an erection, blood must be diverted from the hypogastric arterial system to the corpora cavernosae and the corpus spongiosum. This increased pressure prevents outflow through the local venous system. Owing to the increase in intracavernosal blood flow and the decrease in venous outflow, an erection is initiated and maintained. Damage to the arterial or venous system via injury (seen commonly in bicyclists) or by atherosclerosis can increase the risk for developing ED. In addition, much like with the heart, nitric oxide has a key role in relaxation of the local vessels. Remember that sildenafil was initially studied as a heart medication, and some of the adverse effects we see with its use are due to its vasodilatory effects.
Patient History
Patient history is an important component to treating ED. Some would argue that it is the most important part of the workup. It is essential to differentiate acute from chronic cases of ED.
Cases of acute ED, in which a patient reports that he has only recently had problems with function, usually point to (1) the use of a new medication, (2) a recent injury, or (3) in many cases a psychogenic component. The latter is often hardest to treat. Amino acid therapy may assist with the symptom picture, but often a trained counselor is required to help a patient work through deeper issues. Another option here is the use of constitutional homeopathy.
Patients with chronic ED are much more likely to have an issue related to an underlying cardiovascular or blood glucose–related problem. In addition, medication use can have a role here, especially in older men. Chronic ED tends to come on insidiously, and a patient may mention that he is able to get a partial erection but is unable to maintain it throughout the entirety of intercourse. Older men are at most risk, but more than 50% of my patients with chronic ED are younger than 50 years. Treatment focuses on lifestyle and dietary changes, as well as on increased vascular perfusion.
Patient Examination
The patient examination is similar to our standard cardiovascular workup, including a thorough heart and lung examination, with multiple blood pressure readings. In addition, it is essential to check peripheral pulses, listen for bruits, and perform a complete ophthalmic examination. These examinations will help differentiate vascular-related ED from other types. A genital examination and a digital rectal examination are helpful as well.
Laboratory Studies and Imaging
In my practice, I use several laboratory studies for diagnosis and treatment of ED. Basic blood work, including complete blood cell count, comprehensive metabolic profile, prostate-specific antigen test, thyroid studies (thyrotropin, free triiodothyronine, and free thyroxine), and lipid profile, is essential. In addition to these, I always run 4 hormone studies. The hormones that I test are testosterone, estradiol, dehydroepiandrosterone, and cortisol (twice using salivary testing). If my concern is cardiovascular health, I will also include homocysteine, C-reactive protein, and fibrinogen testing to help with diagnosis. Last, it is essential to perform a urine dip in the office to screen for glucose, proteins, or blood in the urine. In many cases, all of these laboratory values will be within the normal range.
Allopathically, a nocturnal penile tumescence test may be performed. This test monitors how rigid and how long the penis stays erect throughout the night. It is used to determine whether the cause of ED is psychogenic or not. Low values on the nocturnal penile tumescence test can often point to vascular-related issues, and Doppler ultrasonography of the penile arteries may be ordered to observe arterial blood flow.
Allopathic Treatments
Most of us are aware of the allopathic treatments of ED. Vascular-related ED is often treated with phosphodiesterase inhibitors. The 3 main drugs are sildenafil, vardenafil dihydrochloride, and tadalafil. These drugs cause increases in nitric oxide levels, which in turn increase vasodilation. Hypotensive adverse effects, such as priapism, and headaches are part of the adverse effect profile. I rarely prescribe these drugs in my practice because of the many adverse effects. They are also contraindicated in men taking nitrates and have little efficacy in men with late-stage diabetes or psychogenic causes of their ED.
Another option is intrapenile injection therapy. This therapy, often called trimix, injects alprostadil, papaverine hydrochloride, and phentolamine mesylate into the corpora cavernosae. This causes localized vasodilation that allows for increased blood flow to the area, as well as decreased blood flow out of the local venous system. The disadvantages are obvious, and training a man to inject tri-mix is not an easy sell.
Allopathically, low testosterone levels are often treated using injectable forms of testosterone. These injectable forms can sometimes lead to unstable amounts of testosterone in the bloodstream. Patients typically inject testosterone intramuscularly every 1 to 2 weeks.
Naturopathic Treatments
Naturopathic treatments of ED are plentiful. In most cases, a combination of several herbs, dietary and lifestyle changes, and hormonal therapies are used. In my practice, I tend to start with the simple things. This includes working with patients to improve their diet and exercise regimen. Included are decreasing simple carbohydrates and sugars and increasing vasoprotective foods, such as berries, and transitioning patients to organic grass-fed meat and wild fish. This treatment alone can have major implications for their overall health and in the treatment of their ED.
Herbs
I also include several herbs, vitamins, minerals, and amino acids that I have found effective in treating ED. Many of these herbs are mentioned by Buhner3 in his book Vital Man.
Gingko biloba is important to assist with circulation throughout the body and the brain. Gingko is appropriate for any area of the body, including the penis, where there is vascular insufficiency. The recommended dosage is between 100 and 300 mg/d.
Tribulus terresteris has been shown to increase serum levels of testosterone by stimulating the release of luteinizing hormone and by increasing vasodilatation. Buhner states that 80% of men taking Tribulus “show increases in or enhancement of libido, erection, ejaculation, sperm health and orgasm.”3(p38) The recommended dosage is 250 to 500 mg 4 times per day.
Lepidium peruvianum stimulates the release of testosterone and has an affinity for the adrenal glands. Low levels of cortisol can have a major effect on the development of ED. Lepidium has been found to be effective in treating selective serotonin reuptake inhibitor–induced sexual dysfunction.7 The recommended dosage is 2 to 3 g/d.
Several other important herbs are used in treating ED. These include Muira, yohimbe, Panax, Eleuthrococcus, Rhodiola, Vaccinium, Pinus (pollen), Avena, and Allium.
Supplements
Supplements are also used to treat ED. Several are very helpful.
Arginine with pycnogenol assists with nitric oxide release and vasodilation of the vessels. In one study8 92.5% of individuals with ED who were given both of these 2 components together reported normal erections after 3 months of treatment. The recommended dosage is 500 mg of arginine 4 times per day, with 40 mg of pycnogenol 3 to 4 times per day.
Dehydroepiandrosterone is the most abundant steroid in the body and is a mild androgen. It is a precursor to building testosterone and often is depleted well before testosterone. The recommended dosage is 25 to 50 mg/d.
Zinc with copper is an essential component of the treatment plan for every male patient with ED. It is essential in the production and motility of sperm. In addition, zinc is an important coenzyme in the production of testosterone. High dosages of zinc (>60 mg) have been shown to increase testosterone levels. The recommended dosage is 30 to 50 mg of zinc, with 3 to 5 mg of copper (10:1 ratio).
Important vitamin supplements are Bs, C, and D. Also essential are tyrosine, omega-3s, magnesium, and selenium, to name a few.
Bioidentical Hormone Therapy
Bioidentical hormone therapy can also be useful in the treatment of ED. Hypogonadism is defined as a free testosterone level of less than 60 ng/dL or a total testosterone level of less than 200 ng/dL.
The average man produces approximately 8 to 15 mg/d of testosterone. There are many forms of testosterone. Testosterone USP (United States Pharmacopeia) is a natural bioidentical testosterone that can be compounded into a cream or gel. Testosterone should be started at a low dosage owing to adverse effects and because the body often converts excess testosterone to estrogen. This is typically avoided when a smaller daily dose is given rather than a larger intramuscular injection. Dosages are established on an individual basis, but in most cases I start men with low testosterone levels on daily doses of about 25 to 50 mg in a cream or gel. This is applied to the inner arms and thighs, and precautions must be taken to prevent secondary application to significant others.
 John Reynolds, ND is co-owner of Oregon Natural Medicine, an integrated medicine clinic in northeast Portland. He is a graduate of National College of Natural Medicine, Portland, and enjoys practicing all aspects of primary care but has a special interest in men’s health. He was introduced to holistic medicine at an early age growing up in the Florida Keys. His mother was one of the first licensed midwives in the state. His passions include traveling and photography.
John Reynolds, ND is co-owner of Oregon Natural Medicine, an integrated medicine clinic in northeast Portland. He is a graduate of National College of Natural Medicine, Portland, and enjoys practicing all aspects of primary care but has a special interest in men’s health. He was introduced to holistic medicine at an early age growing up in the Florida Keys. His mother was one of the first licensed midwives in the state. His passions include traveling and photography.
References
- UpToDate. Martin KA. Evaluation of male sexual dysfunction. May 2011. http://www.uptodate.com/contents/evaluation-of-male-sexual-dysfunction?source=search_result&selectedTitle=1~150. Accessed September 22, 2011.
- Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med. 2007;120(2):151-157.
- Buhner SH. Vital Man: Natural Healthcare for Men at Midlife. New York, NY: Avery Books; 2003.
- Slag MF, Morley JE, Elson MK, et al. Impotence in medical clinic outpatients. JAMA. 1983;249(13):1736-1740.
- Buvat J, Lemaire A. Endocrine screening in 1,022 men with erectile dysfunction: clinical significance and cost-effective strategy. J Urol. 1997;158(5):1764-1767.
- Gleason JM, Slezak JM, Jung H, et al. Regular nonsteroidal anti-inflammatory drug use and erectile dysfunction. J Urol. 2011;185(4):1388-1393.
- Dording CM, Fisher L, Papakostas G, et al. A double-blind, randomized, pilot dose-finding study of maca root (L. meyenii) for the management of SSRI-induced sexual dysfunction. CNS Neurosci Ther. 2008;14(3):182-191.
- Stanislavov R, Nikolova V. Treatment of erectile dysfunction with pycnogenol and l-arginine. J Sex Marital Ther. 2003;29(3):207-213.