Naturopathic Treatment Options for ADHD
Irene Karatzas, ND
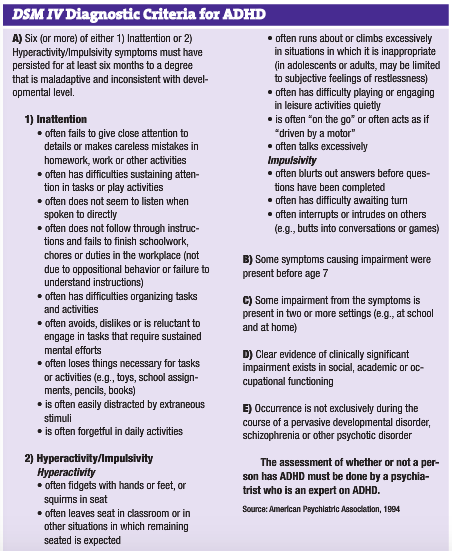
Attention Deficit Disorder (ADD) and Attention Deficit Hyperactivity Disorder (ADHD) are globally recognized as neurobiological disorders that impact a wide range of social, emotional and cognitive developmental processes (Remschmidt and Global ADHD Working Group, 2005; Visser et al., 2007; McLennan, 2006). Different diagnostic criteria have been established for the disorder. According to DSM IV criteria (see Table 1), 4%-8% of children are believed to suffer from ADHD. According to ICD-10 criteria – a stricter diagnostic guideline – the estimated prevalence of ADHD is 1%-3% (Remschmidt and Global ADHD Working Group, 2005; Visser et al., 2007; McLennan, 2006).
Methylphenidate has become the conventional treatment of choice. The medication is a central nervous system stimulant, causing an increase in brain levels of dopamine (Remschmidt and Global ADHD Working Group, 2005; Visser et al., 2007; McLennan, 2006). In addition to stimulants, a number of antidepressant medications may also be employed allopathically in the treatment of ADHD, such as imipramine and bupropion (Remschmidt and Global ADHD Working Group, 2005; Visser et al., 2007; McLennan, 2006). Although often effective for symptoms of ADHD, these medications are associated with a long list of undesirable side effects. In addition to the range of adverse effects associated with these medications comes the stigma of requiring a prescription for mind-altering medication in childhood.
A number of effective naturopathic medicine strategies have emerged for the successful management of ADHD. By combining simple dietary modifications with a select list of supplemental strategies, profound benefit to symptoms of ADHD can often be realized.
Hypoallergenic Diet
A study of 40 children with ADHD were given an elimination diet, and a statistically significant decrease in symptoms of ADHD was found (Pelsser and Buitelaar, 2002). Both immediate and delayed effects are possible with food allergies and sensitivities. Individual food allergy testing may be considered to determine offending foods and maintain a hypoallergenic diet. Enzyme-Linked ImmunoSorbent Assay (ELISA) technology identifies those foods against which the patient is producing IgE and IgG antibodies.
Diet modification plays an important role in the management of ADHD. Dietary recommendations for children with ADHD often include elimination of high-refined carbohydrates, wheat, sucrose, dairy, chocolate and artificial food colorings.
Fish Oil Supplementation
Two recent studies have demonstrated impressive improvement in symptoms of ADD/ADHD through the use of supplemental fish oil (Richardson and Montgomery, 2005; Sinn and Bryan, 2007). The oils utilized delivered a combined total of 750-800mg EPA and DHA per day. The oil used in the studies contained three times more EPA than DHA. Children with ADHD were randomized to receive either placebo or fish oil supplementation. Up to 50% of children receiving fish oil supplements no longer met criteria for ADHD within three months of beginning the supplements. The authors highlight that superior effects were observed as the study progressed; the longer the children took the fish oil, the more their symptoms improved.
Probiotic Supplementation
Several species of bifidobacteria and lactobacilli promote healthy intestinal flora and maintain the mucosal barrier of the gut, preventing pathogenic bacterial, fungal and protozoa from degrading the gut epithelium. Stool samples of children with ADHD were found to have large quantities of known pathogens such as Klebsiella pneumonaie, Citrobacter freundii and Pseudomonas (Pizzorno and Murray, 2006). Small intestine dysbiosis is implicated with elevated levels of the enzyme beta-glucuronidase, which results in heightened blood levels of steroids, negatively impacting children with ADHD (Pizzorno and Murray, 2006).
Nutritional Interventions
Studies suggest both that children with ADHD are likely to be deficient in magnesium and that the deficiency is associated with ADHD. A study of 116 children with ADHD concluded that 95% had magnesium deficiency (Kozielec and Starobrat-Hermelin, 1997). Another study supplemented 200mg/day of magnesium to 50 children with ADHD for six months. When compared to the control group of 25 ADHD kids, there was a decrease in hyperactivity (Starobrat-Hermelin and Kozielec, 1997).
Iron deficiency in children with ADHD vs. iron deficiency in an age- and sex-matched control group suggests that low iron stores contribute to ADHD. Children may benefit from iron supplementation by displaying improved attention, as iron does play a role in synthesis of neurotransmitters (Konofal et al., 2004).
Numerous studies suggest several biochemical heterogeneous etiologies for ADHD, including: food and additive allergies, heavy metal toxicity and other environmental toxins, low-protein/high-carbohydrate diets, mineral imbalances, essential fatty acid and phospholipid deficiencies, amino acid deficiencies, thyroid disorders and B-vitamin deficiencies. When nutritional interventions were used, findings support that the effectiveness may be equal to methylphenidate treatment (Harding et al., 2003).
 Functional Testing To Consider When Treating ADHD
Functional Testing To Consider When Treating ADHD
- Gastrointestinal Assessment: Intestinal permeability, comprehensive stool and digestive analysis, H. Pylori assay, candida antibodies, urinary organic acids profile, urinary peptides, breath testing (post-lactose and post-glucose or lactulose).
- Nutritional Assessment: RBC/serum minerals and vitamins, amino acids, RBC EFAs, urine elements.
- Allergy Assessment: Airborne, diet/symptom diary, elimination diet-food challenge, RAST or ELISA.
- Toxicology Assessment: Liver detoxification capability, fractionated porphyrins, post-chelation urine testing, toxin panels, whole blood lead, stool toxic metal assay, urinary D-glucaric acid, mercapturates.
Irene Karatzas, ND practices at the West Vancouver Wellness Centre in British Columbia. She is a graduate of CCNM in Toronto. Dr. Karatzas is trained in treating various health issues by using laboratory testing and conducting physical examinations. She is also certified in acupuncture and intravenous therapy.
References
Remschmidt H and Global ADHD Working Group: Global consensus on ADHD/HKD, Eur Child Adolesc Psychiatry May;14(3):127-37, 2005.Visser SN et al: National estimates and factors associated with medication treatment for childhood attention-deficit/hyperactivity disorder, Pediatrics Feb;119 Suppl 1:S99-106, 2007.
McLennan JD: Deciding on stimulant use for childhood ADHD: maintaining focus on the key questions, Can Fam Physician Aug;52:940-1, 945-6, 2006.
Pelsser LM and Buitelaar JK: Favourable effect of a standard elimination diet on the behavior of young children with attention deficit hyperactivity disorder (ADHD): a pilot study, Ned Tijdschr Geneeskd Dec 28;146(52):2543-7, 2002.
American Psychiatric Association: DSM IV: Diagnostic and Statistical Manual of Mental Disorders (ed 4), Arlington, 1994, American Psychiatric Association.Richardson AJ and Montgomery P: The Oxford-Durham study: a randomized, controlled trial of dietary supplementation with fatty acids in children with developmental coordination disorder, Pediatrics May;115(5):1360-6, 2005.Sinn N and Bryan J: Effect of supplementation with polyunsaturated fatty acids and micronutrients on learning and behavior problems associated with child ADHD, J Dev Behav Pediatr Apr;28(2):82-91, 2007.Pizzorno Joseph E and Murray Michael T: Textbook of Natural Medicine, Vol. 2 (ed 3), London, 2006, Churchill Livingstone.
Kozielec T and Starobrat-Hermelin B : Assessment of magnesium levels in children with attention deficit hyperactivity disorder (ADHD), Magnes Res Jun;10(2):143-8, 1997.
Starobrat-Hermelin B and Kozielec T: The effects of magnesium physiological supplementation on hyperactivity in children with attention deficit hyperactivity disorder (ADHD). Positive response to magnesium oral loading test, Magnes Res Jun;10(2):149-56, 1997.
Konofal E et al : Iron deficiency in children with attention-deficit/hyperactivity disorder, Arch Pediatr Adolesc Med Dec;158(12):1113-5, 2004.
Harding KL et al: Outcome-based comparison of Ritalin versus food-supplement treated children with AD/HD, Altern Med Rev Aug;8(3):319-30, 2003.