Homeopathic Treatment of PANS
Vis Medicatrix Naturae
Jamie Oskin, ND
PANS1 (formerly PANDAS2) is an acronym for Pediatric Acute-onset Neuropsychiatric Syndrome. This diagnosis is still controversial, yet is gaining support due to many publications illustrating a link between acute/febrile illnesses and an abrupt onset of obsessive-compulsive disorder (OCD), tics, and neuropsychiatric symptoms. The neuropsychiatric symptoms may include: anxiety, emotional lability and/or depression, irritability, aggression and/or severely oppositional behaviors, behavioral regression, deterioration in school performance, and somatic signs and symptoms, including sleep disturbances, enuresis or urinary frequency. A diagnosis of PANS is made when the symptoms cannot be better explained by known disorders such as Sydenham’s chorea, Tourette’s, lupus, etc.
The former acronym, PANDAS, referenced a subset of PANS patients with an abrupt onset of OCD and tics following a streptococcal bacterial infection; it was considered to be autoimmune3 in nature and affected similar areas of the brain, but to a less severe extent, as Sydenham’s chorea.4 The diagnosis has since been expanded to PANS to include a broader range of infectious triggers, as well as non-infectious etiologies if the criteria are met for “abrupt onset.”1
Current Treatments
Current treatments for PANS include long-term prophylactic antibiotics,5 short-term corticosteroids,6, 7 intravenous immunoglobulin (IVIG) and plasmaphoresis,8, 9 selective-serotonin reuptake inhibitors (SSRIs),10 and cognitive behavioral therapy.11 Alternative and naturopathic physicians treating PANS have proposed adding treatments such as curcumin,12 food allergy elimination, treating yeast and gastrointestinal infections, and additional immunosupportive treatments.13
Homœopathy
Homœopathy is safe, gentle, and effective in the treatment of PANS. Homœopathy can often help children who are suffering from PANS — as their symptoms are improved holistically, they are able to wean off many of their medications and discontinue prophylactic antimicrobial treatment.
Historically, the founder of homœopathy, Samuel Hahnemann, gained some initial fame and credibility for the homœopathic method by successfully treating deadly scarlet fever epidemics,14, 15 and there is historical evidence in the homœopathic literature of Sydenham’s chorea being treated homœopathically.16 Because scarlet fever and Sydenham’s chorea are both streptococcal sequelae, it is not entirely unexpected that we can apply safe, simple substances via the totality of characteristic symptoms homœopathically, according to the Law of Similars,*17 to help children suffering from PANDAS/PANS. Homœopathic treatment is most effective in helping the tics, OCD, and neuropsychiatric symptoms in PANS cases, and it also helps to reduce the frequency and intensity of episodic relapses over the course of long-term treatment.
Here I will present 3 cases from my practice that are being successfully treated with homœopathy.
Case Study 1
Jeb is an 11-year-old male who started to develop tics and OCD behaviors around age 7. His symptoms began as throat-clearing and head-rolling. It took several years to obtain an accurate diagnosis because PANS is still not well-recognized by many healthcare professionals. The odd thing about his symptoms were that they would episodically flair during and after streptococcal pharyngitis infections or streptococcal erysipelas eruptions on his face. The tics and OCD behaviors would remain elevated for about 2 months following a streptococcal infection, and would eventually diminish, though not go away.
He would also sometimes have an atypical strep pharyngitis presentation, with asthma-like symptoms and a cough during the episodes, which were worse from inhaling cold air. During these episodes, he tested positive for a strep infection with a throat culture. During a recent flair (January, 2014) of tics and OCD behaviors, his pediatrician ran Antistreptolysin O (ASO) titers that were positive (250 IU/mL; normal <150) and diagnosed him with PANDAS.
When Jeb first presented to me, his tics included a need to touch his knee to his head and an impulse to touch or nudge objects. According to Jeb, he would also feel the impulse to have to collect every coin in a certain video game, or “kill every character” and get “everything perfectly done” in the game before he could allow himself to move on to the next level of the video game. He was fastidious and became quite irritated if a lampshade was off-center or if a picture frame was tilted. He had a very strong fear of contagious disease. He would even throw away his lunch if another child touched his food, for fear of becoming sick. Unfortunately, the other kids would tease Jeb at school because of his fear of germs. He was very fidgety and had difficulty sitting still.
Jeb had a past medical history of eczema that was strongly triggered by dairy. Jeb’s mother also reported that as a child he would bounce off the walls if he had candy, especially candy containing red dyes, like red licorice, which she made him avoid. He craved hot foods.
I prescribed Arsenicum album 30C, 3 pellets sublinqually QD. Figure 1 shows the repertorization of symptoms, utilizing the computer Programme version of George Dimitriadis’ 2nd edition English translation of Bönninghausen’s Therapeutic Pocketbook (TBR2).†18
Figure 1. Analysis – Case Study 1
At Jeb’s first monthly follow-up visit, he reported a significant reduction in both tics and OCD symptoms. For example, he no longer cared if another person touched his food at school and would happily eat it without fear of contagion. He had no new episodes of asthma or skin eruptions, and he no longer had to get up from dinner to reheat his food several times during a meal to make sure it was hot.
Over the course of the next several months, we went up in potency periodically as his symptoms plateaued or there were slight regressions in improvement. His symptoms are markedly reduced and continue to improve. He and his parents are very happy with the marked and speedy improvement because it has been a struggle for the prior 4 years. Jeb loves acting and he was very excited to tell me that he had been selected to be in 2 theater productions, which were now much easier to participate in because his tics were greatly reduced (Organon §9).
Ben is a 12-year-old male whose parents first brought him in for homœopathic treatment of PANDAS on January 31, 2014. He had been diagnosed with PANDAS by the leading PANDAS expert in Los Angeles about a year previously. That physician had prescribed long-term antibiotics (azithromycin, 250 mg BID), as well as several other medications and supplements that Ben had been on for the past year since obtaining the diagnosis. His parents had recently relocated to Phoenix and were looking for new treatment options because his OCD and tics were persisting despite the litany of medications and supplements he was taking. They were also concerned about the potential side effects of long-term antibiotic use.
During early childhood, Ben had undiagnosed asthma and was put on frequent rounds of antibiotics for respiratory infections. Ben’s parents noted that he was always sick with a croupy cough. He had long-standing nocturnal enuresis, as far back as his parents could remember, although those symptoms were suppressed by 2 medications: desmopressin and oxybutinin. At that time, between the ages of 4 and 5, his parents noted that his behaviors were “not right.” He was extremely hyperactive and wild, and his parents were starting to get complaints from teachers about his behaviors. Around age 5, Ben was diagnosed with ADHD and started on medication. They tried several medications, and methylphenidate, extended-release, was the one that worked for the longest period of time for his ADHD symptoms.
Ben’s tics began around 7 or 8 years old with eye-rolling, which was thought to be a side effect of the methylphenidate. His main tics were rapid head-twitching and grunting. Ben had chronic right neck pain and tension for the past several years due to his sudden head-jerking tics. At one point he developed a tic that caused his leg to spring up. At the age of 8 he was diagnosed with Tourette’s syndrome, due to the vocal and motor tics. In addition to the tics, Ben had several OCD behaviors.
Around age 8, his behaviors at home were becoming very problematic, due to hitting and anger outbursts. Ben’s parents reported that he was punching holes in the walls. He would get very angry at his younger brother if his brother called him a name or teased him. When Ben was younger, he would have uncontrollable anger and would hit and be violent or throw things. He was incredibly sensitive to insult and reprimand, which could set off the anger outbursts. Additionally, Ben noted that his tics were much worse when he became angry.
Although Ben fully expressed his anger at home, he bottled it up at school. His parents reported that if kids teased him at school, Ben would not show his anger to the other kids. Instead, he suppressed it and would go to the school bathroom where he would have an outburst of screaming. Sometimes, at the end of the school day, Ben would even run into his parents’ car and scream, just to let out the suppressed anger from the day. His parents recalled that he was badly bullied at school in third grade, prior to the onset of the tics and prior to the methylphenidate. They recalled that his teacher called Ben “stupid” in the hall, and he went into the bathroom and hit the toilet paper rolls to get his anger out.
Eventually, the family came across the specialist in LA who ran blood work in January, 2013, due to his frequent infections, OCD, and tics. His strep titers were extremely elevated (see Table 1) and he was diagnosed with PANDAS. Ben’s tics began to improve with IVIG treatments, which clinically supported the PANDAS diagnosis and autoimmune etiology. However, his white blood cell count dropped too low on the IVIG and antibiotic treatments, so the IVIG was stopped. His anger outbursts had not improved with the antibiotics and IVIG treatments. Additionally, his strep titers had not gone down significantly on repeat labs after being on antibiotics and IVIG treatments (see Table 1). Antibiotics were continued, even though the IVIG was stopped.
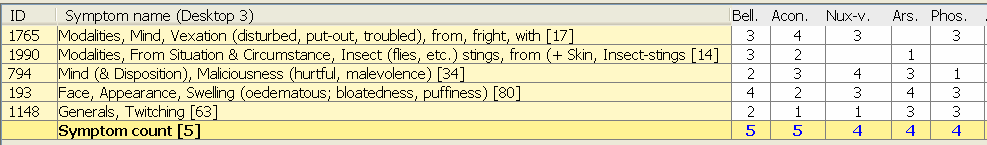
I prescribed Staphisagria 30C, 3 pellets sublingually QD, based on repertorization of the symptoms listed in Figure 2. I kept all other medications and supplements the same, so as to only change 1 variable in the case at a time.
Ben had a tendency to get frequent infections since early childhood, which likely predisposed him to the PANDAS autoimmune process. Since he is susceptible to tics, they may have been exacerbated by other factors, such as the methyphenidate, since tics are a known side effect of stimulant ADHD medications. Thus, the tics may be multifactorial. Regardless of the cause, the symptoms indicating Staphisagria predated the later, more progressed, expression of the disease. Staphisagria matched the most characteristic symptoms, in this case Ben’s suppressed anger and his sensitivity to insult and reprimand, which are triggering modalities of the chief complaints,‡19 ie, the anger outbursts and tics.
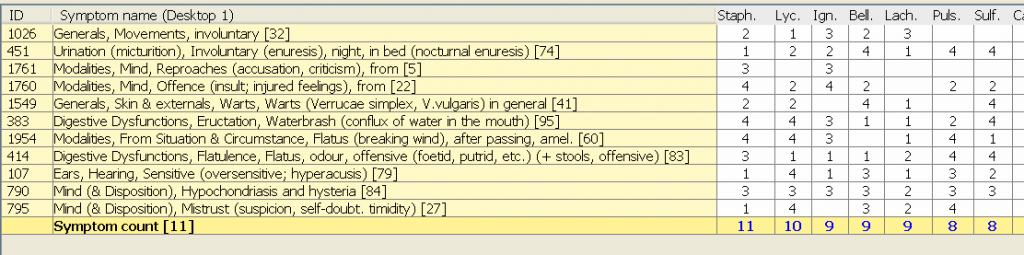
Figure 2. Case Study 2 – Analysis
(Repertorization using the computer version of George Dimitriadis’ translation of Bönninghausen’s Therapeutic Pocketbook, TBR2)18
Within 3 months of being on Staphisagria, Ben reported that his anger was much improved. He still had a predisposition to become angry, but he was more able to control his anger without it bothering him as much. For example, he was not yelling back or hitting his brother as much when teased. He no longer needed to run to the car to scream after getting out of school for the day. He reported that his tics were, “Way less! I almost never have them.” His neck pain from the tics was also gone.
We ran strep titers prior to his 3-month follow-up appointment. Ben’s mother was happy because although his strep titers were still elevated, they were reduced (see Table 1). It is impossible to attribute the decreased strep titers to the homœopathic treatment because it is possible that they would have declined gradually over time on their own, since he was being treated with long-term antibiotics (thereby reducing the risk of relapse with a new strep infection). Despite this, it is a good sign that his immune system is settling down, and it follows the timeline of the improvement in his tics since starting homœopathy. His parents are happy that within 3 months of starting homœopathic treatment, they have seen a marked reduction in behavior outbursts and tics. Because his OCD symptoms have not improved significantly from the first prescription, Ben may require subsequent homœopathic prescriptions after the initial main problems (aggravation from vexation and anger, tics) are no longer problematic. Long-standing chronic diseases often require a sequence of prescriptions over the course of an extended period of time to cure the case (Organon §162 to 184). Over time, we plan to slowly and carefully wean him from his allopathic medications as he continues to improve with homœopathic treatment.
Table 1. Ben’s History of Strep Titers
| Strep Titer Dates | Antistreptolysin O Ab Titers(normal range: 0-200 IU/mL) | Anti-DNase B Strep Ab Titers (normal range: 0-170 U/mL) |
| 01/16/2013 | 594.5 (H) | 774 (H) |
| 04/15/2013 | 532.3 (H) | 603 (H) |
| 05/06/2014 | 453.1 (H) | 308 (H) |
Case Study 3
Allison is an 8-year-old female who was adopted from Vietnam. When she first presented to me in January of 2014, she was suffering from a litany of concerns including: reactive attachment disorder, PTSD, Lyme’s, Marfan’s syndrome, developmental expressive language delays, and PANS. She was also positive for a 5-MTHFR gene mutation. She was being treated by one of the top PANS neurologists in town and was taking a regimen of 23 different long-term medications and supplements per day, including: 2 antibiotics, an antiviral medication, a non-stimulant ADHD medication, an SSRI, and an anti-histamine allergy medication.
Allison was badly neglected and abused in the orphanage prior to her adoption at the age of 5. She was not allowed to speak in the orphanage, so she had extreme expressive language delays, only knowing about 5 words in her native language when she was adopted. She was clearly malnourished at adoption, with a distended abdomen, visible ribs, and hair thinning. She also had bruises from suspected physical abuse. She was terrified after the adoption, and when the family brought her home to the United States, she sat in a corner rocking and screaming all weekend. Allison would also hit, scream, claw, and bite. On Monday morning, immediately after being brought to the United States, her adoptive parents took her to a pediatrician. She was put on diazepam, and referred for counseling and to a pediatric psychiatrist. The psychiatrist stopped the diazepam and put her on a longer-term psychotropic medication regimen.
She was referred to a neurologist at a prominent local children’s hospital who diagnosed her with PANS in December of 2012 after extensive neurological and laboratory work-up. She was initially prescribed azithromycin, which helped her PANS symptoms rather dramatically and helped confirm the diagnosis clinically. However, she relapsed in August, 2013, after a mosquito bite that caused her entire left leg and her face to swell. Within 2 days of the insect bite, she markedly relapsed with rages, uncontrollable tantrums, OCD behaviors, tics, and oppositional behaviors.
The nervous tics following the insect bite included shaking her leg a lot, shoulder twitching, and eye twitching. She also had a variety of other tics manifest from time to time, including trichotillomania, blinking, and touching her tongue to her nose. She also exhibited OCD behaviors, including a compulsive need to flick the light switches on and off in a rigid pattern. She would repeat to herself over and over and over again, even if her parents responded to her questions. She would get stuck and could not be redirected once her mind was fixated on a topic. She would have to obsessively hold a book all day long, or repetitively throw an object at the wall over and over without being able to be stopped. She would pick her fingers to the point of bleeding, and she was having chronic bed-wetting. She was very sensitive to loud noises and bright lights.
Allison’s parents reported terrible mood swings, with violent behaviors towards siblings, parents, teachers, and other children at school. She would hit, kick, spit, throw things, and run away from her teachers at school. She was easily frightened by unexpected loud noises. She was constantly moving; as her mother described, “there’s never a calm moment.” Unfortunately, since the mosquito bite that triggered the relapse of her PANS, the many medications and supplements were not easing her symptoms, and her mother was on the brink of exhaustion and desperation.
In a case this complex, I chose to divide the symptoms according to their timeline. The symptoms of developmental delay, hypotonia, developmental coordination disorder, reactive attachment disorder, and PTSD pre-dating the onset of the PANS seemed to be related, but were dissimilar disease (Organon §§40 to 42) compared to the new-onset symptoms after the PANS relapse in August, 2013. The sharp demarcation in symptoms following the mosquito bite helps delineate the separate disease processes. Figure 3 shows the repertorization of the most characteristic symptoms in the case.
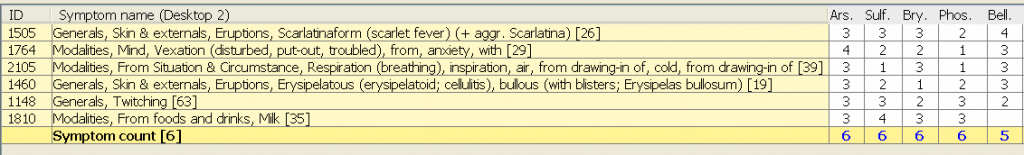
Figure 3. Case Study 3 – Analysis
(Repertorization using the computer version of George Dimitriadis’ translation of Bönninghausen’s Therapeutic Pocketbook, TBR2)18
In addition to the symptoms repertorized, the cognitive delay, bed-wetting, restlessness, carphologia (picking), sensitivity to noise, and photophobia were well-matched to Belladonna. I began the case with Belladonna 6C, 3 pellets sublingually QD, on January 9, 2014. Due to acute illnesses, we had to quickly change the potency several times within the first month of treatment.
On February 6, 2014, Allison had her first follow-up appointment, having been on Belladonna 200C QD. Her symptoms were improved: Her mother reported a 50 to 70% improvement in violent behaviors, she had not run away from her teachers, and her tics were 75% reduced. Her mother also noticed that her OCD behaviors were starting to lessen because her morning routine was not as challenging. She also was not complaining of photophobia or sensitivity to noises. Additionally, her running was a little more coordinated and she was not falling as much.
Allison had several fits and starts with relapses, which is typical of PANS due to the episodic nature of the condition. However, she responded markedly to daily doses of increasing potencies of Belladonna following each relapse. Her teacher was also impressed and sent home 2 notes because Allison’s handwriting had dramatically improved within a short time-frame. This is remarkable because it has been documented that children with PANS can have sudden regression in handwriting and drawing skills as a result of the disorder.1 Additionally, her school behavior reports improved, from average scores of around 30% prior to starting homœopathic treatment, to above 90% after homœopathic treatment. Her mother noted that they were shocked that she had 10 straight days of school behavior reports above 90%. Allison’s language was improving, and she could play outside on a sunny day without needing to wear sunglasses like she used to, since her photophobia was much less intense.
This third case is much more severe and complex than the first 2 cases. Because of the episodic nature of PANS, this case is not yet “out of the woods” and will require long-term persistence for a good prognosis. Educating parents with informed consent about what to expect in a more severe and challenging case such as Allison’s, is crucial to the long-term prognosis. The case can become more difficult to manage when all providers are not on the same page, or if the parents, when feeling desperate, quickly change medications without consulting the homœopath. These cases require more patience and perseverance from the family and the doctor, in order to reduce the chance of relapse, and will likely require several years of treatment with several remedy and potency changes along the way. Thankfully, with accurate prescriptions, Allison has responded very markedly and rapidly to homœopathic treatment and has been able to successfully wean off several of her long-term medications that had not been producing significant improvement in her symptoms. Her parents have been very happy with her progress since starting homœopathy.
Conclusion
Pediatric acute-onset, neuropsychiatric syndrome (PANS, formerly PANDAS) is a condition often triggered by infection and featuring an abrupt onset of OCD, tics, and various neuropsychiatric symptoms. This article constitutes an initial case series that document homœopathy as a safe, gentle, and effective system of medicine that can help in the treatment of children suffering from post-febrile OCD and tic behaviors due to this disorder.
* The homœopath applies the law of similars (Similia Similibus Curantur) when selecting a prescription according to the instructions Hahnemann gave in the Organon of Medicine (see aphorisms §24, §25, §153) by intentionally attempting to distinguish the remedy that is most similar (according to proving experiments of substances on healthy individuals) to the symptoms of the patient’s presenting case of disease. This process is void of all speculative reasoning (see aphorisms §6, §110). Hahnemannian prescribing differs from modern techniques, which incorrectly call themselves homœopathy, that utilize speculative theories, such as the doctrine of signatures, in order to select a medicinal substance.
† Dimitriadis’ Therapeutic Pocketbook Method is the most accurate English re-translation of Bönninghausen’s Therapeutisches Taschenbuch, carefully corrected with reference to his original manuscript.
‡ “The chief signs are those symptoms that are most constant, most striking, and most annoying to the patient. The physician marks them down as the strongest, the principal features of the picture. The most singular, most uncommon signs furnish the characteristic, the distinctive, the peculiar features.”

Jamie Oskin, ND, is a naturopathic physician with a passion for homœopathy. He is focused on helping families overcome childhood developmental disorders. He is in private practice in Phoenix, AZ, and is adjunct faculty in the homœopathy department at Southwest College of Naturopathic Medicine. He completed a homœopathic selective residency at the Southwest Naturopathic Medical Center, which was fully funded by a generous gift from Standard Homeopathic Company. Read more at http://www.AzNaturalHealth.com.
References:
- Swedo SE, Leckman JF, Rose NR. From Research Subgroup to Clinical Syndrome: Modifying the PANDAS Criteria to Describe PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). Pediatr Therapeut. 2012;2(2):113.
- Swedo SE, Leonard HL, Garvey M, et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am J Psychiatry. 1998;155(2):264-271.
- Pavone P, Bianchini R, Parano E, et al. Anti-brain antibodies in PANDAS versus uncomplicated streptococcal infection. Pediatr Neurol. 2004;30(2):107-110.
- Kirvan CA, Swedo SE, Snider LA, Cunningham MW. Antibody-mediated neuronal cell signaling in behavior and movement disorders. J Neuroimmunol. 2006;179(1-2):173-179.
- Snider LA, Lougee L, Slattery M, et al. Antibiotics prophylaxis with azithromycin or penicillin for childhood-onset neuropsychiatric disorders. Biol Psychiatry. 2005;57(7):788-792.
- Kondo K, Kabasawa T. Improvement in Gilles de la Tourette syndrome after corticosteroid therapy. Ann Neurol. 1978;4(4):387.
- Matarazzo EB. Tourette’s Syndrome Treated with ACTH and Prednisone: Report of Two Cases. J Child Adolesc Psychopharmacol. 1992;2(3):215-226.
- Perlmutter SJ, Leitman SF, Garvey MA, et al. Therapeutic plasma exchange and intravenous immunoglobulin for obsessive-compulsive disorder and tic disorders in childhood. Lancet. 1999;354(9185):1153-1158.
- Garvey MA, Snider LA, Leitman SF, et al. Treatment of Sydenham’s chorea with intravenous immunoglobulin, plasma exchange, or prednisone. J Child Neurol. 2005;20(5):424-442.
- Pigott TA, Seay SM: A review of the efficacy of selective serotonin reuptake inhibitors in obsessive-compulsive disorder. J Clin Psychiatry. 1999;60(2):101-106.
- Storch EA, Murphy TK, Geffken GR, et al. Cognitive behavioral therapy for PANDAS-related obsessive compulsive disorder: findings from a preliminary waitlist controlled open trial. J Am Acad Child Adolesc Psychiatry. 2006;45(10):1171-1178.
- Aggarwal BB, Harikumar KB. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int J Biochem Cell Biol. 2009;41(1):40-59.
- Rondeau S. PANDAS: An Immune-Mediated Mental Illness. NDNR. 2010;6(12):1-4.
- Hahnemann S. Cure and Prevention of Scarlet Fever (1801). In: Dudgeon RE. The Lesser Writings of Samuel Hahnemann. New Delhi, India: B Jain Publishers; 1851: 369-385.
- Hahnemann S. Observations on the Scarlet-Fever (1808). In: Dudgeon RE. The Lesser Writings of Samuel Hahnemann. New Delhi, India: B Jain Publishers; 1851: 479-483.
- Hahnemann S. The Chronic Diseases, Their Peculiar Nature and Their Homoeopathic Cure. CK translation by Tafel LH;1895. Indian reprint edition: New Delhi: B Jain Publishers; 2007: 4,74.
- Hahnemann S. Organon of Medicine. Translated from the Fifth German edition by Dudgeon RE. London, England: W Headland; 1833. Translated by R.E. Dudgeon, §24, §25, §153.
- Dimitriadis G. The Bönninghausen Repertory (Therapeutic Pocketbook Method). 2nd ed. Sydney, Australia: Hahnemann Institute; 2010.
- Hahnemann S. The Medicine of Experience. In: Dudgeon RE. The Lesser Writings of Samuel Hahnemann. New Delhi, India: B Jain Publishers; 1851: