Reversing Stage 3 Kidney Disease: A Case Study
Shawna Eischens, ND
Tolle Totum
Why is my urine frothy?
What can I do to help my kidneys from being damaged even further?
What is the cause of protein in my urine?
“John” had asked previous physicians these questions but had received no helpful or hopeful answers. This patient walked into my office on 8 medications, frustrated with his medical team, and scared that death was imminent.
“Is there anything you can do to help my kidneys and reverse my diabetes?” he asked.
“Of course there is!” I said with excitement, knowing the incredible power of the body to repair itself when provided with the proper conditions to do so. I was confident and hopeful for this particular patient because he had already shown a level of commitment by drastically changing his diet. When patients are invested in their health, I have more confidence and trust in the body’s ability to heal.
Background
This patient is one of the more than 30 million people in the United States diagnosed with type 2 diabetes mellitus (T2DM), which accounts for 90-95% of all types of diabetes.1 In 2015, according to the CDC, an estimated 1.5 million new cases of diabetes were diagnosed among US adults 18 years and older.1 The total estimated annual cost of diagnosed diabetes in the United States in 2012 was $245 billion, with medical expenditures being approximately 2.3 times higher than expenditures would be in the absence of diabetes.2 Diabetes has been listed as the seventh leading cause of death, yet the following statistics show that diabetes is strongly correlated with heart disease, the #1 leading cause of death:
- At least 68% of diabetics age 65 or older die from some form of heart disease3
- Adults with diabetes are 2-4 times more likely to die from heart disease than adults without diabetes3
- Diabetes is listed as the only cause of death for 79 535 people, yet more than triple that number of people (252 806) have diabetes listed as an underlying or contributing cause on their death certificates1
Regardless of these staggering statistics, we know that unregulated blood sugar levels have detrimental consequences for patients’ health and national healthcare costs. Medications can help decrease hyperglycemia, which is essential for overall health, but they tend to come with harmful and comprehensive side-effects. Medications are not curative, are not ideal for health restoration, and tend to instill a dependent, disempowering mentality based on a false sense of security. The road to curing or reversing T2DM requires more than medications alone. Reversal of any disease process requires an investment in personal health and a commitment to lifestyle changes. Foundations of health for people with diabetes include the following:
- Diet: Small changes can have profound effects. Patients may do best with drastic changes to their current routine, yet many patients report feeling overwhelmed at the thought of an overnight diet overhaul. Educating and inspiring patients to make multiple, small changes – versus scaring them that they can never enjoy a dessert again – can have a more beneficial effect long-term. People are often shocked to learn that milk, beans, bread, potatoes, tortillas, and fruit can have a detrimental effect on blood sugar levels. Encouraging consumption of low-carb, nutrient-rich foods with plentiful antioxidants can help heal the entire person. These include green, leafy and cruciferous vegetables; wild fish such as salmon; organic, grass-fed/finished meat; green tea; and turmeric. Eggs, walnuts, almond butter, flax seeds, pumpkin seeds, and cheese may also be beneficial for someone with hyperglycemia.
- Exercise: Daily movement is key! A vigorous walk after dinner, bouncing on a rebounder while watching TV, or strength-training alternating with jumping jacks or dynamic planks for high-intensity interval training, are just a few ideas. Resistance exercise is ideal, as it burns 19 times more glucose compared to aerobic exercise.4
- Sleep: Less than 5 hours of sleep per night has been shown to increase a person’s risk of obesity by 235%.4 Sleep deprivation leads to a decrease in both insulin sensitivity and fat cells’ sensitivity to insulin.4 The body’s natural response is to produce less leptin and more ghrelin, leading to increased hunger, especially for carbohydrates.4 Inadequate sleep also contributes to elevated cortisol,4 which can increase glucose and contribute to insulin resistance, all of which are counterproductive in patients with diabetes.
Case Study
John, a 62-year-old Caucasian male, presented in my office after being given a diagnosis of T2DM within the previous 12 months. Diagnosed as pre-diabetic in 2010, he likely had uncontrolled hyperglycemia for many months or even years. The typical concurrent diagnoses with T2DM of hyperlipidemia and hypertension were also part of his medical history. Without an ideal comparison of urine microalbumin levels, there wasn’t enough information for confirmation, but according to KDIGO (Kidney Disease: Improving Global Outcomes) guidelines, this patient appeared to be in the “high risk” G3bA1 or G3bA2 kidney disease category. Regardless of his specific diagnosis, the sequela of kidney disease the previous summer came as a worrisome shock to him, and he implemented a drastic dietary change immediately upon hearing these findings.
John reported his previous health history to include excess weight since childhood, as well as rosacea, depression, anxiety, right-sided renal calculi, and acid reflux. His current health history included cataracts, bilateral hand tremors, leg cramps, insomnia, and some occasional mild, bilateral neuropathy that he described as “itching” or “like wearing socks” on his feet.
He claimed feeling like he was in good health until 2007, although he had some weight and reflux concerns before then. At his heaviest, he weighed 295 pounds (BMI of 43.6). He noticed his urine could appear foamy, and his bowel pattern tended to be soft or loose. His sleep was better than ever since improving his diet. He was sleeping 8-9 hours a night, and expressed a desire to continue using quetiapine, an antipsychotic, for the off-label use of insomnia.
His previous standard American diet, consisting of fast and fried food, candy, chocolate, soda, and cookies, had recently and drastically changed to exclude these foods, in addition to potatoes and grains. He began eating more salads, cheese, fish, steak, and vegetables, while sticking to his routine of 2 meals a day. He had lost 25 pounds, with little to no exercise in just over 2 months. He was monitoring his fasting blood sugars in the morning and in the evening after dinner. With his recent dietary improvements, his blood sugars were better than previous months, but still high ranging between 101-303 mg/dL in the weeks leading up to our appointment.
Medications prescribed by his MD’s:
- (H)(D)**50 mg Quetiapine fumarate 50 mg x 7 years for insomnia. Patient wanted to stay on this medication.
- (R)*10 mg Lisinopril for hypertension.
- (R)(D)**Ranitidine 150 mg x 2 at night x 31 years for acid reflux.
- (G)*Metformin HCL 1000 mg bid for T2DM.
- (R)*Glipizide XL 10 mg bid for T2DM.
- (R)*Januvia 50 mg for T2DM.
- (R)**Hydrochlorothiazide 25 mg for hypertension.
- (R)(D)*NA bicarbonate 650 mg x 2 weeks after low CO2/bicarbonate lab finding.
Key:
(R)*Caution with renal impairment
(D)*Caution with diabetes
(H)*Caution with hyperlipidemia
(G)* Contraindicated in people with eGFR <46
Note:*One week earlier, he had self-prescribed Tylenol for ear pain and within an hour he experienced vertigo, nausea, and gait disturbances.
**Various statins had been prescribed by multiple physicians over the years for hypercholesterolemia. Patient reported experiencing flank pain as a side effect and discontinued use.
Self-Prescribed Supplements
- Vitamin B1, B2, B6 (uncertain dosages)
- B12, 1000 µg
- Vitamin E, 1000 IU
- Turmeric, 400 mg
- Lutein, 20 mg
- Probiotic
PE Findings
- Blood pressure: 112/84 mm Hg
- O2 saturation: 98%
- Pulse: 84 bpm
- Weight: 260 lb
- Height: 5’9”
- Body mass index: 38.4
Although labs from various physicians had been ordered, only those done consistently and with comparable units are included in this article for fair comparisons.
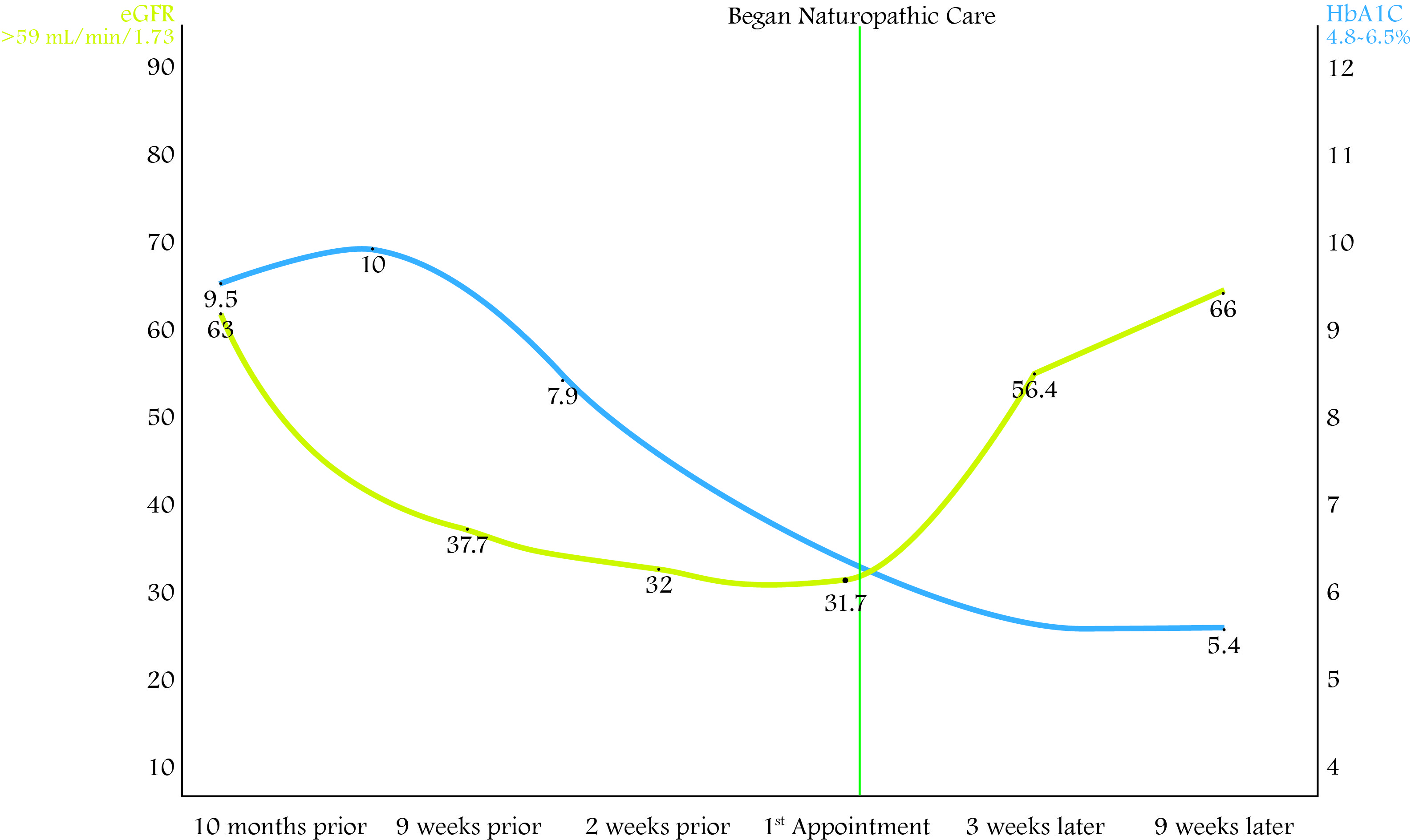
Two weeks before our appointment, his labs show clear cause for concern: his kidneys were not properly functioning, resulting in electrolyte imbalance (Table 1, Figure 1).
Treatment
Prioritizing cost-effective supplementation to produce beneficial results is a goal with all patients; however, this patient’s extreme financial concerns were expressed and a modest treatment plan was presented. I commended and encouraged him on his commitment to his recent dietary modifications and provided a dietary handout to further balance blood sugars.
Initial treatment recommendations included:
- 10-20 minutes of exercise each day
- Hot Epsom salt baths 3 times per week and/or sweating during exercise to balance elevated potassium levels. (Epsom salt baths were also indicated for his likely decreased magnesium levels, although we didn’t confirm this via lab testing until days later.)
- 5-10 drops per day of a liquid homeopathic combination product to promote healthy kidney, liver, and digestive function
- 6 caps per day of a proprietary product with kidney extract, to support and restore kidney function
- Supportive acupuncture and a lab draw were done in office
John’s lab results arrived days later showing his blood type (O) and a detrimental progression of his kidney dysfunction during the weeks prior to our appointment. We discussed the fact that hydrochlorothiazide (HCTZ) and ranitidine are not recommended for people with kidney disease or diabetes. HCTZ promotes insulin resistance and diabetes, depletes magnesium, lowers HDL-cholesterol, and raises LDL-C, all of which are antagonizing and create an obstacle-to-cure for this patient.
John was on the verge of stage 4 kidney disease. As a result, the following additional recommendations were made:
- Take 1 teaspoon 3x/day of an herbal combination tincture with nephroprotective/nephrorestorative benefits
- Increase kidney extract product to 9 caps per day
- Eat more wild/organic/free-range meat, fish, and/or eggs, and avoid gluten in accordance with his blood type
- Stop HCTZ (with no previous or current edema, this was possible without weaning); instead begin amlodipine 5 mg
Table 1. Lab Results Over Time; please note the shaded boxes
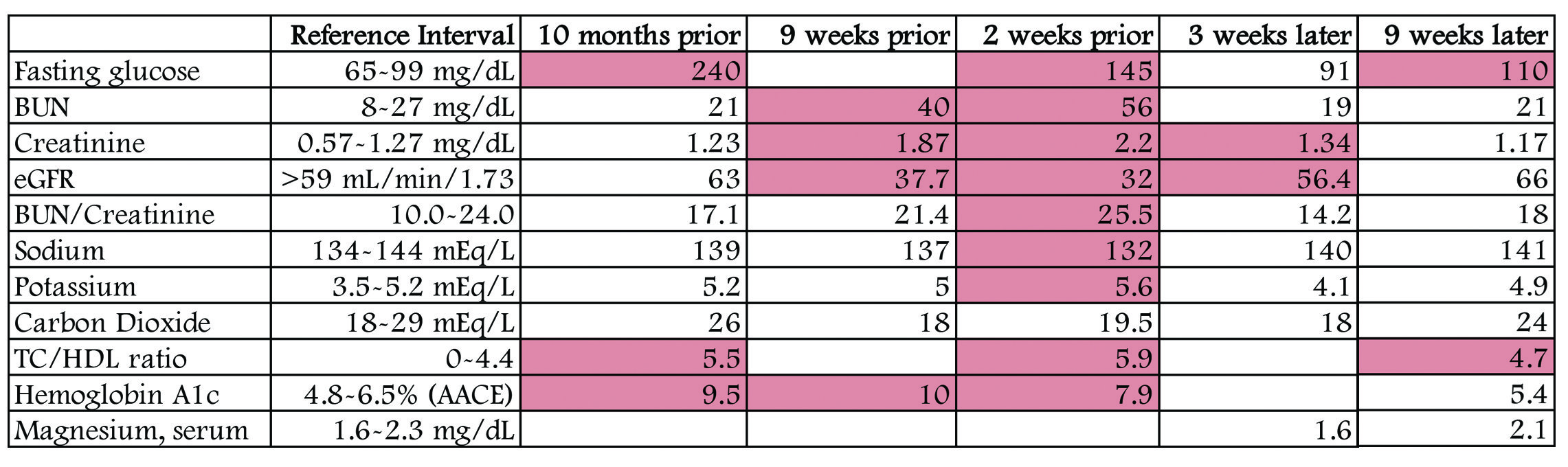
(BUN=blood urea nitrogen; eGFR=estimated glomerular filtration rate; TC=total cholesterol; HbA1C=hemoglobin A1C)
Figure 1. eGFR & HbA1C Over Time
First Follow-up, 3 Weeks Later
John reported that his leg cramps and loose stool had ceased and that he had lost a few pounds. His daily blood sugars improved, with a range of 86-206 mg/dL. Since starting amlodipine, his hand tremors had worsened. He expressed a desire to get off of his medications and reported that his primary care physicians did not plan to run labs or have an appointment for another 6 months. He was aware that discontinuing medication was not realistic without making lifestyle changes and supporting his body to help balance blood sugars, cholesterol levels, and blood pressure while also helping his kidneys repair with supportive treatments. With a recent loss of his job and health insurance, John was unable to afford cash pricing for sitagliptin or any equivalent. Sitagliptin was his most recent medication prescribed for T2DM, is not recommended for patients with a GFR between 30 and 50 mL/min, and does not clinically lower HbA1c levels as well as other medications.
PE Findings
- Blood pressure: 156/84 mm Hg
- Pulse: 73 bpm
- O2 saturation: 98%
- Weight: 258 lb
Remarkably, just a few weeks after beginning treatment, his labs showed a 78% increase in GFR, along with balanced electrolytes, BUN, and glucose.
Treatment
- Continue previous treatment, and add 1 scoop of a powder with glutamine and curcumin to encourage digestive healing. Experiment 1 week later with reducing ranitidine to every other day. If tolerated without reflux, take 1 ranitidine every third day the following week.
- Decrease daily amlodipine dose to 2.5 mg
- Begin a supplement that helps normalize blood pressure while supporting the cardiovascular system: 1 cap twice daily
- Monitor for any increase of blood sugars after discontinuing sitagliptin
Second Follow-up, 3 Weeks Later
John’s daily blood sugars ranged from 89-190 mg/dL, even after stopping sitagliptin 2 weeks prior. He had lost 2 more pounds. Mild heartburn was observed by the patient nights 3 and 4 of his wean from ranitidine; otherwise, he had experienced no symptoms of heartburn. Exercise was still minimal. He had never experienced any irregular heart rhythms, and his physical exam was consistent with regular heart sounds and rhythms. Emotionally, he felt more balanced.
PE Findings
- Blood pressure: 140/70 mm Hg
- O2 saturation: 97%
- Pulse: 54 bpm
- Weight: 256 lb
Treatment
- Continue with previous recommendations. Finish current digestive healing powder; don’t replenish.
- Begin a supplement that helps balance blood sugars: 1 cap twice daily
- If blood pressure readings are within range, discontinue amlodipine 2 days before next appointment
Third Follow-up, 3 Weeks Later
Home-monitored blood sugars ranged from 77-179 mg/dL. The patient reported better readings, except after eating pasta or desserts, which clearly correlated with higher readings. A total of 3.5 more pounds were shed. He stopped amlodipine 3 days prior, and reported no concerns or symptoms. He reported feeling better overall.
PE Findings
- Blood pressure: 145/80 mm Hg
- O2 saturation: 98%
- Pulse: 57 bpm
- Weight: 252.5 lb
John’s labs continued to improve, including the best TC/HDL ratio and A1c % he had achieved in years.
Treatment
- Continue treatment plan, minus Epsom salt baths
- Discontinue Na-bicarbonate
- Finish, and hold off on buying more self-prescribed supplements
- Increase exercise frequency and/or duration
Summary
Even with minor changes and a budget-conscious treatment plan, this patient’s healing was profoundly rapid. Within weeks of beginning treatment, he decreased his medication use by 50% and was more balanced physically, emotionally, and physiologically. Proper diet, sleep, and exercise patterns create a foundation for health, while eliminating obstacles to cure and supporting the body with restorative treatments potentiates healing.
As Dr Henry Lindlahr stated, “Chronic supposed-to-be-incurable diseases yield to the natural treatments, provided there is enough vitality in the system to respond to treatment and the destruction of vital parts and organs has not too far advanced.” I appreciate this patient’s motivation to heal and commitment to his health before his diseases were too far progressed. I am filled with gratitude to our miraculous body, this patient, and naturopathic medicine for continuing to amaze me with the incredible, innate ability of the body to heal.
References:
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Available at: https://cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.Accessed January 5, 2018.
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033-1046.
- American Heart Association. Cardiovascular Disease & Diabetes. Last reviewed August 2015. Available at: https://tinyurl.com/yb3f6sk4. Accessed January 5, 2018.
- Morstein M. Master Your Diabetes: A Comprehensive, Integrated Approach for Both Type 1 and Type 2 Diabetes. White River Junction, VT: Chelsea Green Publishing; 2017: 49, 50, 273.
Image Copyright: <a href=’https://www.123rf.com/profile_bschonewille’>bschonewille / 123RF Stock Photo</a>
 Shawna Eischens, ND, (“Dr. E”) is a 2012 graduate of SCNM who practices at Rockwood Natural Medicine Clinic in Scottsdale, AZ. As a primary-care physician who focuses on mental and digestive health, Dr E is passionate about helping people realize their greatness to achieve physical and emotional health. Outside of the office, she enjoys volunteering with Naturopathic Medicine Institute and Big Brothers Big Sisters, as well as exploring nature via foot, bike, car, or boat.
Shawna Eischens, ND, (“Dr. E”) is a 2012 graduate of SCNM who practices at Rockwood Natural Medicine Clinic in Scottsdale, AZ. As a primary-care physician who focuses on mental and digestive health, Dr E is passionate about helping people realize their greatness to achieve physical and emotional health. Outside of the office, she enjoys volunteering with Naturopathic Medicine Institute and Big Brothers Big Sisters, as well as exploring nature via foot, bike, car, or boat.










