David A. Tallman, DC, NMD
Abstract
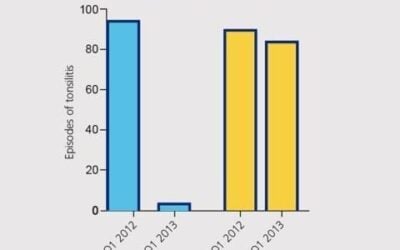
This article discusses three cases of acute traumatic complete anterior cruciate ligament (ACL) ruptures that were treated with regenerative injection therapy. The cases include before and after magnetic resonance (MR) scans demonstrating complete re-ligamentization of the ACLs. The patients were initially treated with autologous platelet-rich plasma (PRP), then followed up with dextrose injection therapy. All patients were released with a full and unrestricted function of the treated knee. Meniscus tearing was present on one of the patients’ MR scans, which was also subsequently restored to a symptom-free state. Five-year follow-up revealed unrestricted activity of the treated knees. A perusal of PubMed reveals several articles discussing the use of PRP in the treatment of ACL tears, with several forthcoming in the pipeline.
Introduction
The popularity of injection techniques may seem novel to the general population, but actually have a history spanning at least five millennia. Otzi (1991 Otzal Alps) was found to have had his joints treated with a metallic needle. Orthopedic regenerative techniques via a heated needle were described by Hippocrates’s On Joints (4th century BC), and finally brought into American mainstream medicine via the tireless work of Ross Hauser, MD. The word “regenerative” is now added to food and product labels to assist in sales. By 2025, myriad allographs, autographs, and even new peptide categories will be available for regenerative injection use. During my PubMed search, I noticed nearly all articles discussed the use of PRP to enhance arthroscopic procedures, while few were exclusive to injection-only conservative treatments. Noteworthy was a 2024 Cureus article, demonstrating that 10 out of 10 ACL tear patients made a full recovery and a return to sports at 16 weeks, treated by injection-only PRP. In my personal history of treating ACL tears, only one patient did not achieve complete ACL recovery but was symptom-free at 4-year follow-up.
All three patients discussed in this article were treated within 2 weeks of the date of injury. Complete and anatomic religamentization was achieved on all patients by 16 weeks of tear. All other knee ligaments were evaluated by ultrasound at each visit. All sprained or strained tissue was treated by a combination of a needling technique and simultaneous deposition of PRP, hypertonic dextrose, or a 40% dilution of dextrose, glycerin, and phenol (DGP 25%, 25%, 2.5%). Regenerative injection should be the first-line treatment of choice for an acute complete or partial thickness ACL tear. Bedside autologous grafts have been the only injection modality I have ever used to treat ACL tears within 6 weeks of injury. Patient D had three treatments in between the MR scans, patient C had four, and patient P only one.
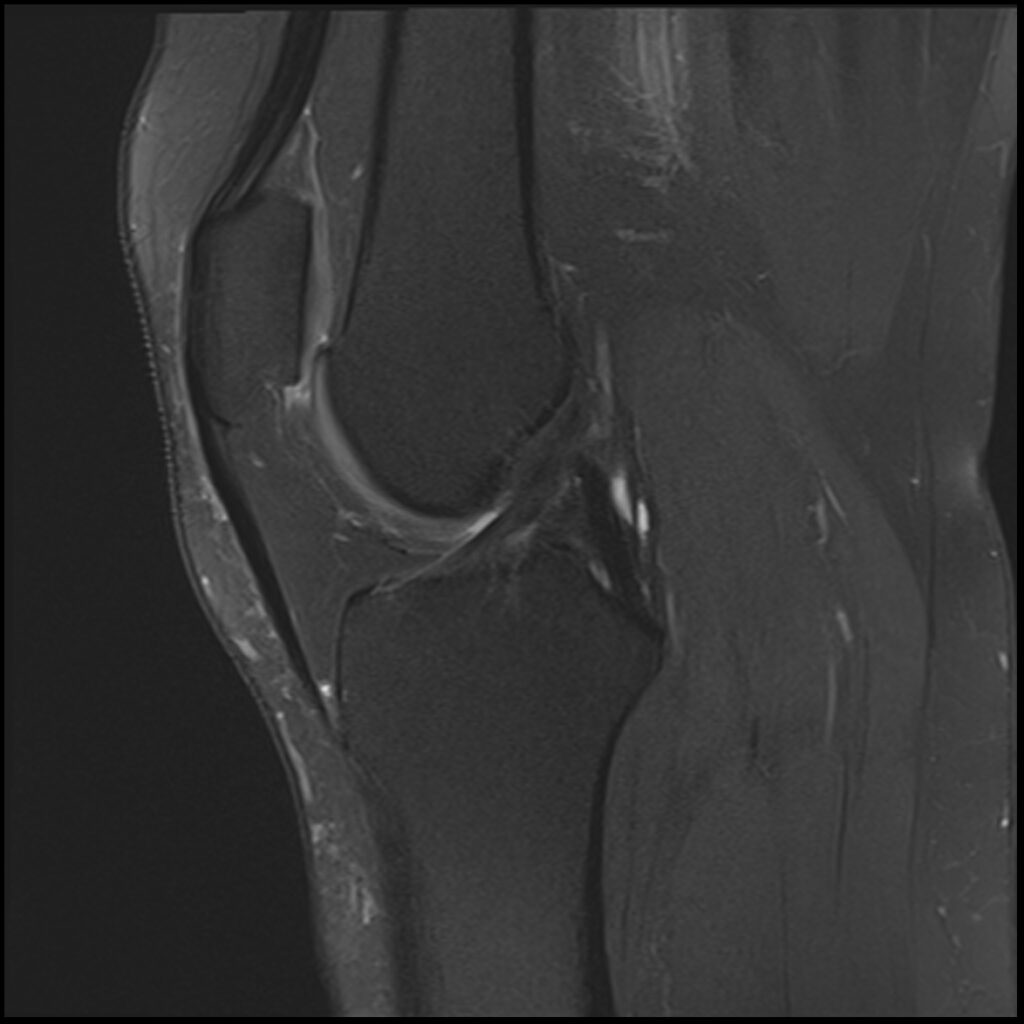
Patient D, age 19, sustained a competitive tumbling injury that involved a hard landing with the pathognomonic plant and pivot that directly tractions the ACL along its doubly obliqued path. The first MR scan was done the day after the trauma. She was initially treated 5 days post-injury. Her knee effusion was completely aspirated, then replaced with 3cc of autologous platelet-rich plasma and 5cc of platelet-poor plasma. Using ultrasound guidance, the ACL origin at the posterior femur was treated after carefully avoiding the vasculature and nerves. She was then instructed not to bear weight for 3 days, then use crutches/assisted weight bearing for 2 weeks. She was then to use a compression knee sleeve during sports or exercise. At her follow-up visit at 4 weeks, she was still having some instability at times and lateral knee pain. Her knee was evaluated with an ultrasound, and any areas of pathology seen were treated with hypertonic dextrose injection and needling technique. This included her medial and lateral collateral ligaments, and the patellar tendon and ligament. At 12-week follow-up, she continued to have some minor issues with her knee, so another evaluation and treatment were performed with hypertonic dextrose to the injured ligament and tendon areas found on the ultrasound examination. We obtained a new MR for her 16-week follow-up and noticed the ACL had re-ligamentized, and she reported full function and return to exercise. At 5-year follow-up, she claimed she was fully active, pain-free, but no longer tumbling.
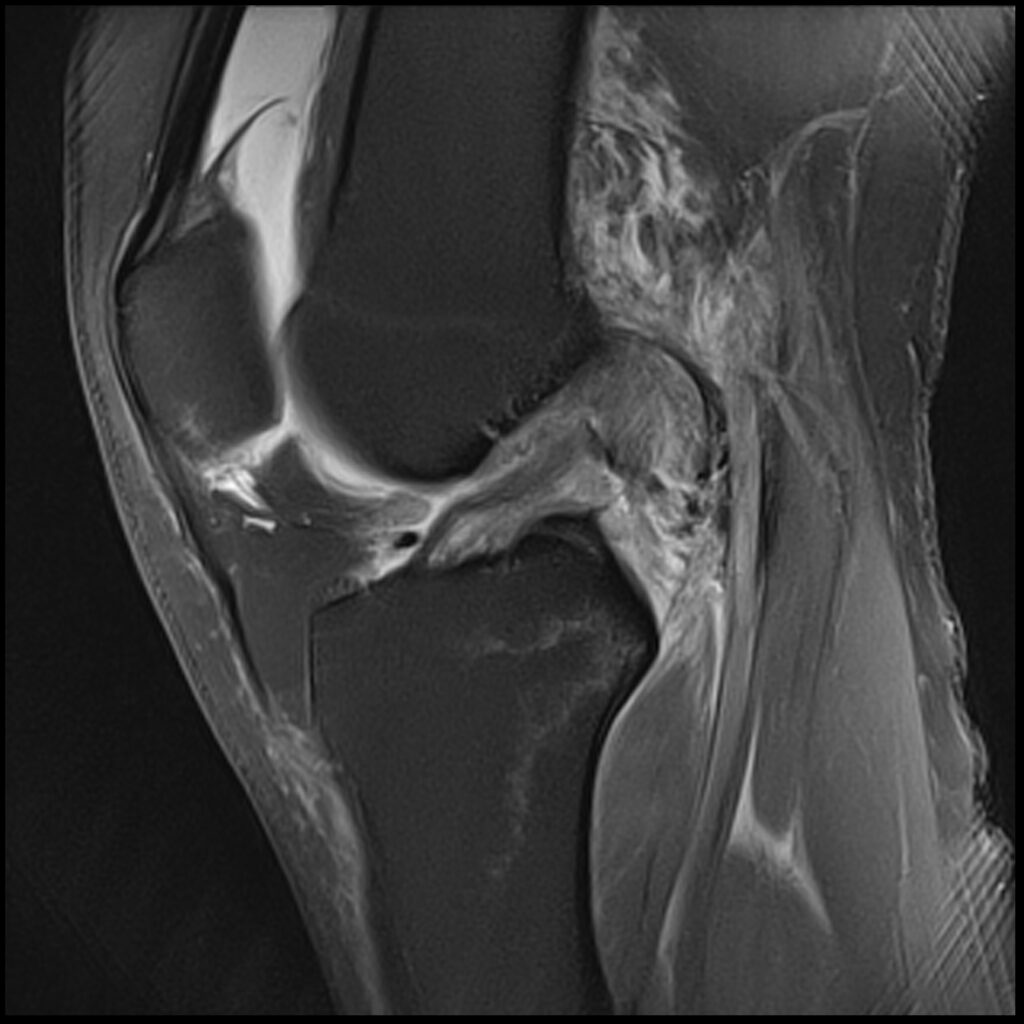
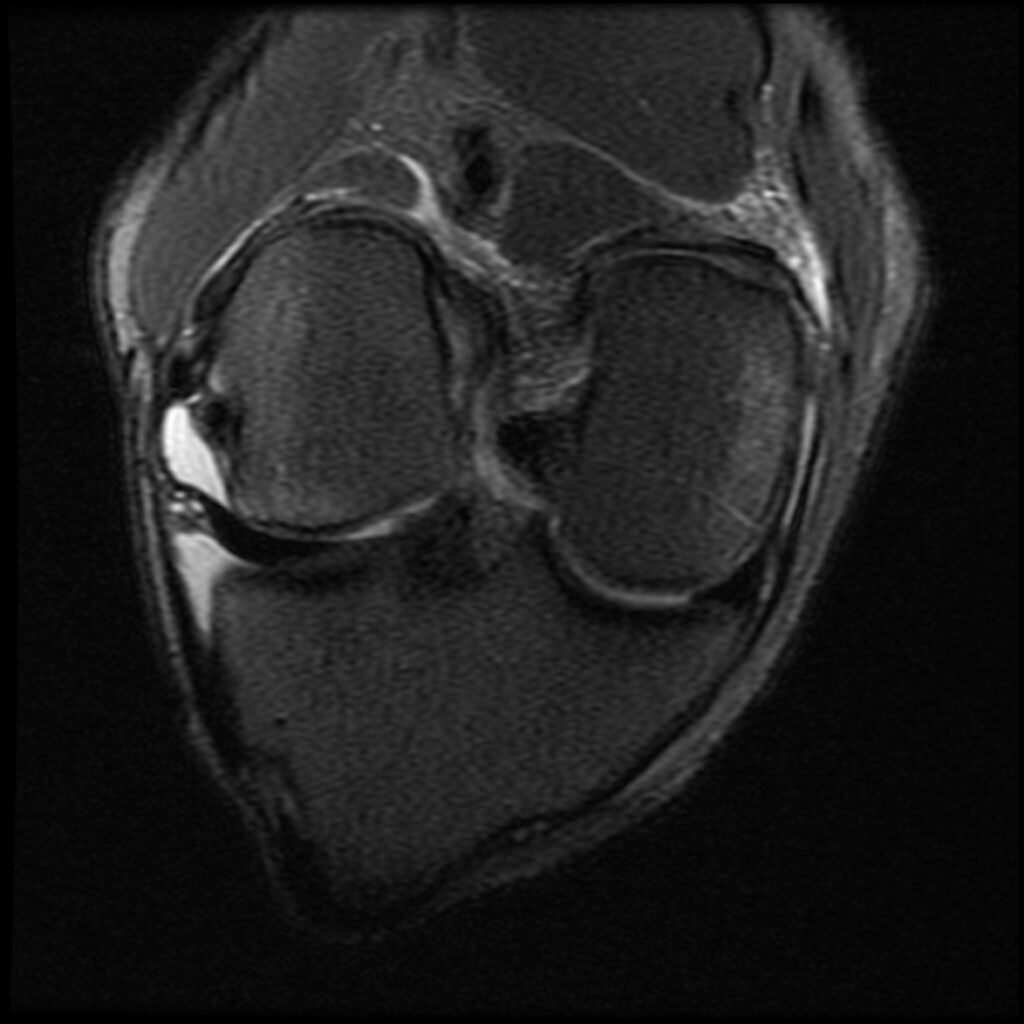
Patient D Before

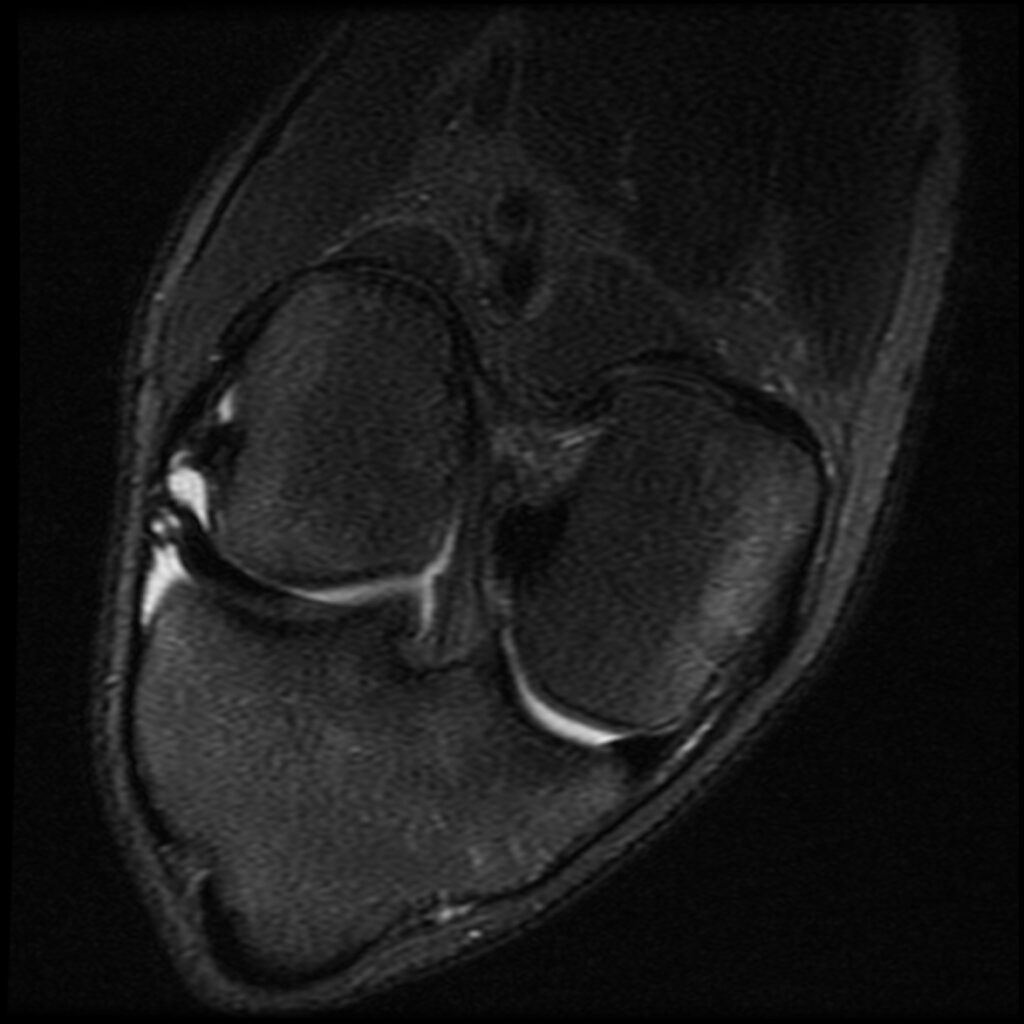
Patient D After
Patient D Before

Patient D After
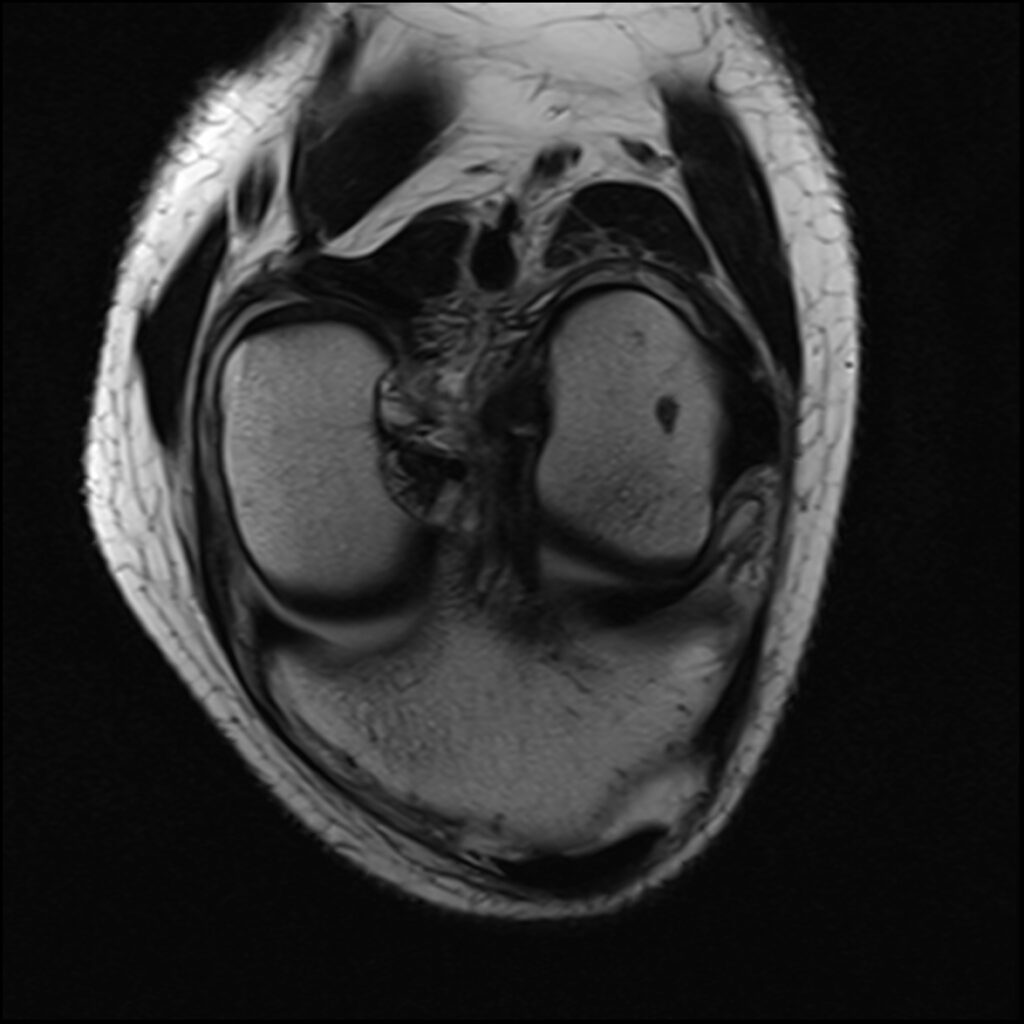
Patient C, age 44, was jumping on a trampoline when her foot got caught during rebound landing and forced the knee to extend and twist, tearing her ACL and medial meniscus and causing a Segond’s fracture, a posterolateral compression injury seen on the T2 sagittal MR images. Immediately upon becoming aware of her ACL injury, she asked my staff if she could put her “before & after” MR scans on my practice’s website after it healed. The initial treatment and aftercare were the same as patient D, aspirating any effusion and treating the posterolateral origin of the ACL. At 8-week follow-up, her knee was treated with hypertonic dextrose, with the collateral ligaments being treated with DGP. She was treated again at 16 weeks with another autologous PRP treatment of the knee joint, ligaments, and tendons. She was released to full sports and activities at 18 weeks post-injury. Subsequent MR scan revealed complete recovery of her ACL. Low grey signal replaced the original high signal intensity tear in the meniscus, appearing healed. Her knee was reported to be symptom-free at 5-year follow-up.
Patient C Before
Patient C After
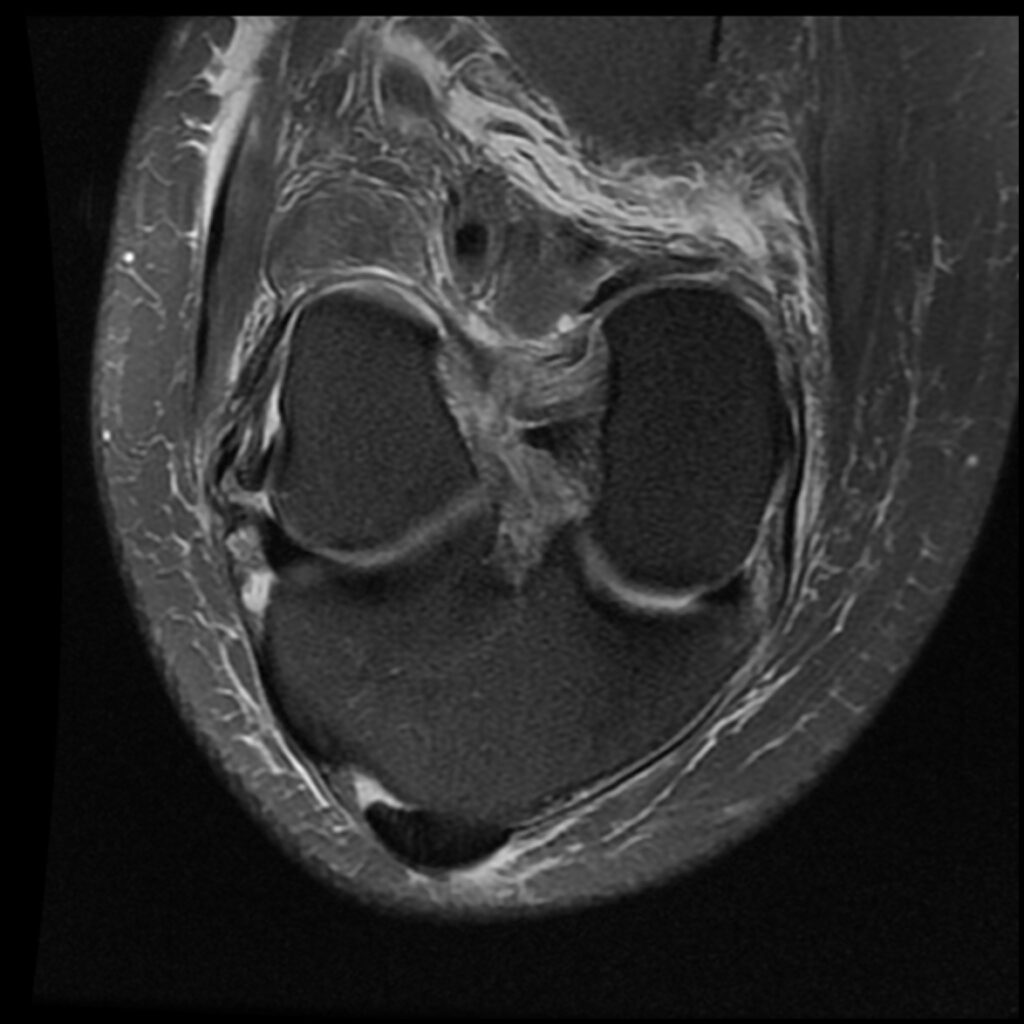
Patient C Before
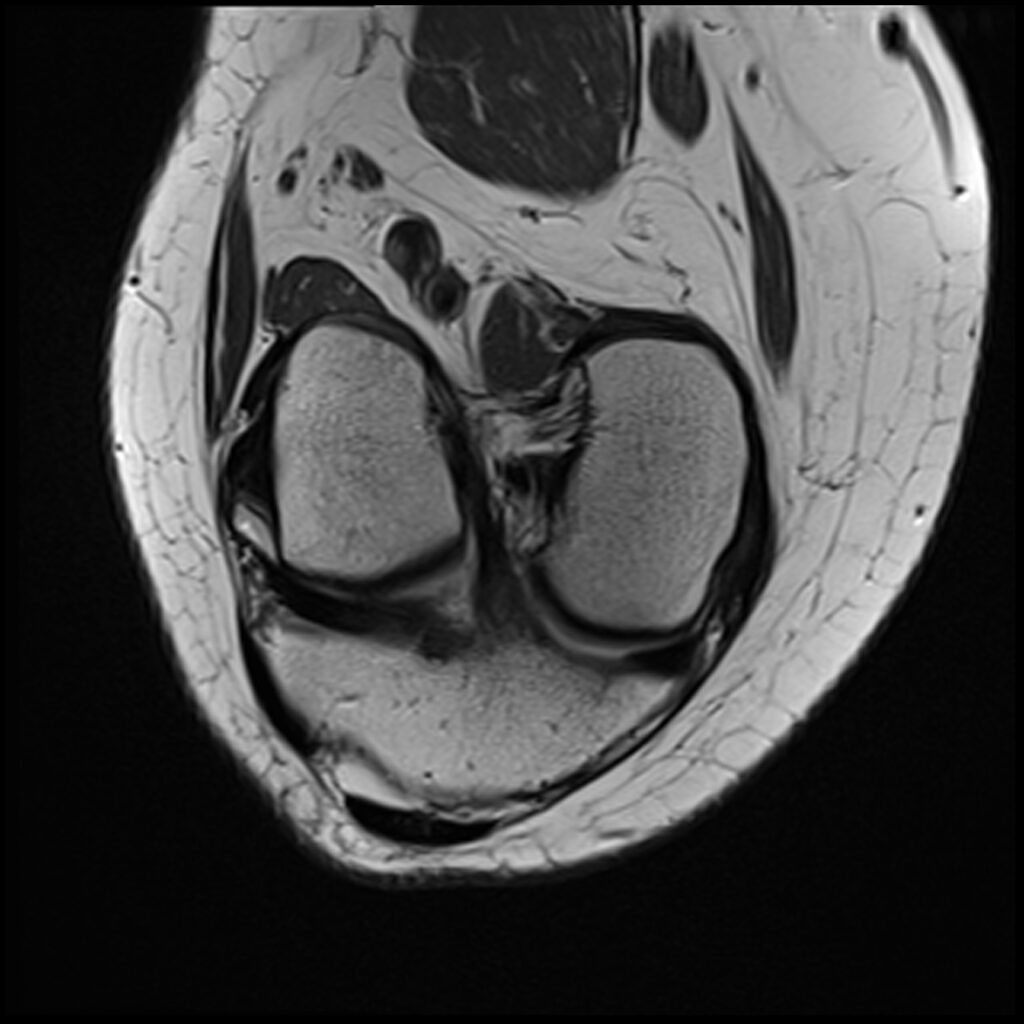
Patient C After
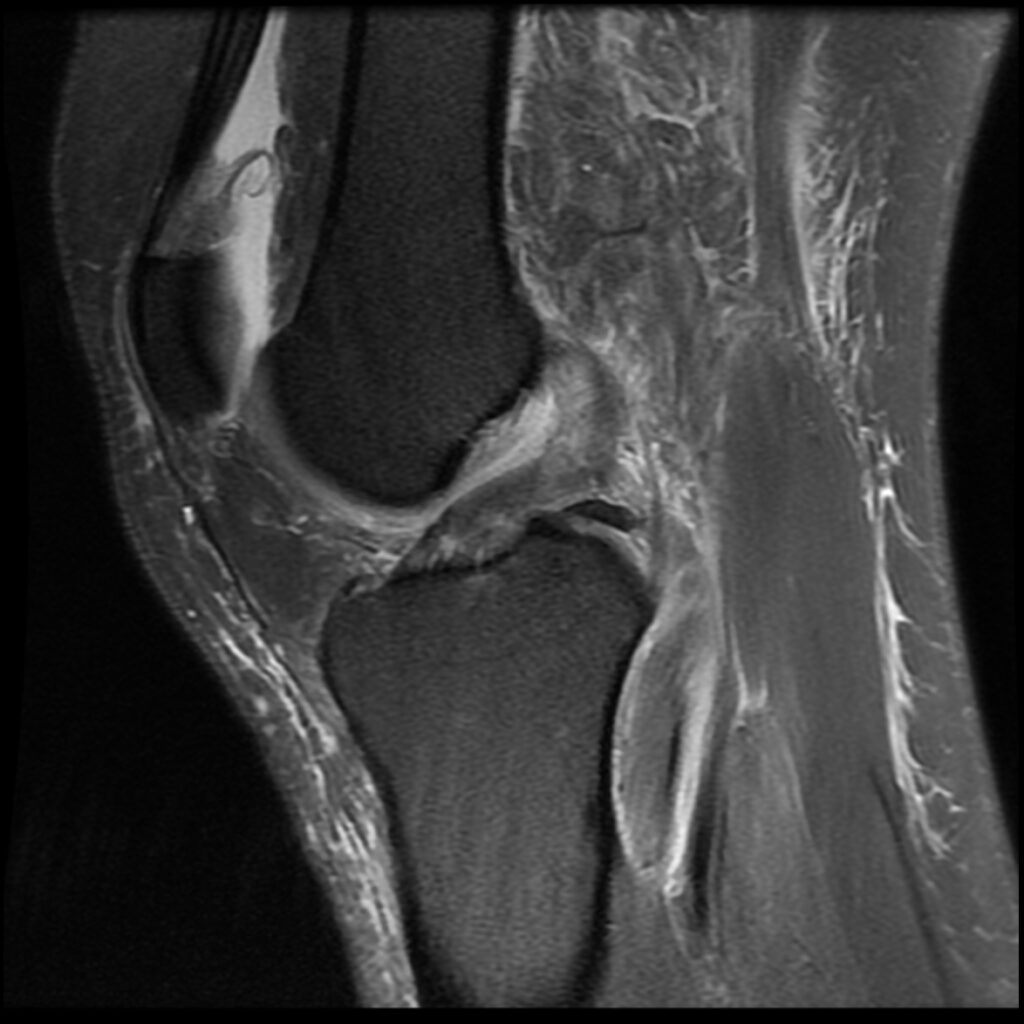
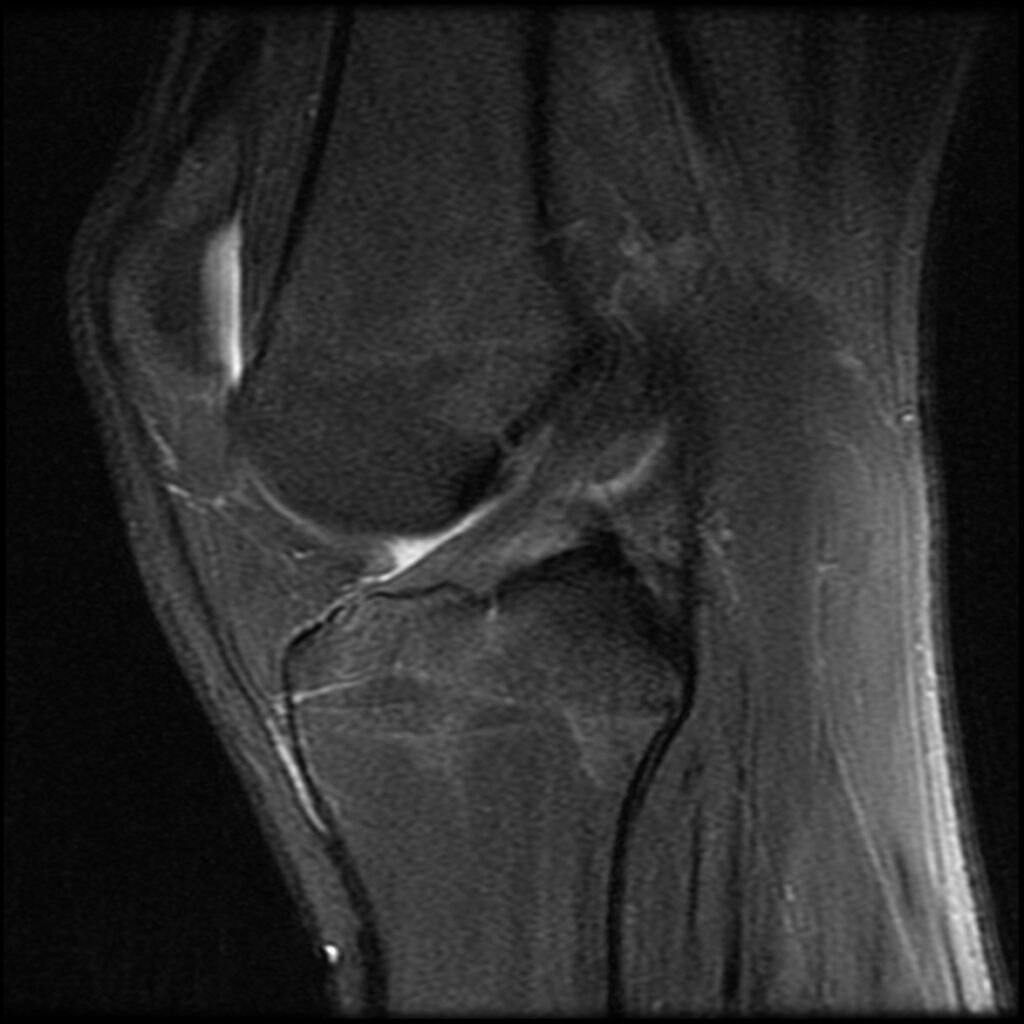
Patient P, age 20, was playing soccer when his running foot got planted and stayed in the same position while his body continued going forward and rotated around the knee. This is the pathognomonic soccer ACL injury players try to avoid when they “tuck & roll” rather than resist going horizontal. Soccer players tend to have longer careers than their American football counterparts because they never resist falling and going down. Tucking & rolling redirects the force rather than meeting the momentum head-on. The tucking part forces your bones and joints into optimal alignment and flexion, adding obstacles to injury if I may be so bold. P was given the same initial treatment and aftercare as patient D, aspirating any effusion and again treating the posterolateral origin of the ACL. His first follow-up was at 16 weeks. His MR demonstrated complete re-ligamentization of the ACL. He stated that he had already been symptom-free and back to playing soccer regularly, only wearing a neoprene sleeve to remind him to be careful.

Patient P Before
Patient P After
Patient P Before
Patient P After

David A. Tallman, DC, NMD continued a family tradition at the Ohio State University for his undergraduate education. He then attended Texas Chiropractic College with an internship focus on radiology. Since graduating from Southwest College of Naturopathic Medicine, the focus of the entire practice has been in corrective treatment of spine and joint conditions. He is a board-certified, licensed chiropractic physician (DC) and a licensed naturopathic medical doctor (NMD).
Dr. Tallman is a pioneer of regenerative injection therapy (RIT); his practice is devoted exclusively to prolotherapy / RIT. A unique and highly specialized method of needle manipulation over the years has evolved to maximize the effectiveness of the different medicines and biologics. He pursues state-of-the-art developments in orthopedics and musculoskeletal radiology (ultrasound, x-ray, CT, MRI) in the U.S. and Europe.
Reference
Conservative Treatment Using Platelet-Rich Plasma for Acute Anterior Cruciate Ligament Injuries in Highly Active Patients: A Retrospective Survey. Hada, Hada, Yoshida, et al. Cureus 2024 Jan 28;16(1):e53102