Botanical and Nutrient Therapies
By Alexandra Mele, ND
This article explores the case of a 76-year-old patient with treatment-resistant paroxysmal atrial fibrillation. It highlights how botanical medicines and nutrient therapies complement conventional care, including managing atrial fibrillation episodes, hypertension, and related cardiovascular concerns.
Introduction to the Case
Atrial fibrillation (AF) is a common complaint for naturopathic physicians practicing preventative or primary care. Often, patients are on multiple medications and remain symptomatic. This is the case of a 76-year-old female experiencing dizziness, insomnia, tachycardia with regular pulses at the rate of 122 bpm and blood pressure of 123/79 mmHg.
Patient Presentation and History
The patient had a prior history of Wolff-Parkinson-White (WPW) syndrome many years ago, with no reported episodes in the past 15-20 years. She also had a history of rectal cancer and hypothyroidism. Current medications included:
- Atenolol 25mg and telmisartan 80mg for hypertension
- Desiccated thyroid extract 45mg
- Enteric-coated peppermint oil for intermittent IBS.
Cardiology Interventions
This patient deferred an initial recommendation to present to the emergency room for presumed atrial fibrillation or a potential recurrence of WPW. However, she agreed to visit urgent care for a stat ECG. ECG demonstrated atrial flutter, and the patient was sent to the emergency department for immediate cardioversion. She was started on apixaban 5mg twice daily and advised to see cardiology. Was in and out of the emergency department several more times for uncontrolled episodes of atrial flutter, put on sotalol 80mg twice daily for rate and rhythm control, underwent second cardioversion, stress test, and echocardiogram with no findings suggestive of causation of chronic atrial flutter. The patient was very frustrated as she likes to travel with her husband and did not feel safe doing so with ongoing episodes. The patient sought my advice on adjunctive therapeutics to help manage episodes and more recent onset of treatment-resistant hypertension. Cardiology urged the patient to move forward with cardiac ablation for paroxysmal episodes, which she was hesitant towards but agreed to.
Adjunctive Therapies for Atrial Fibrillation
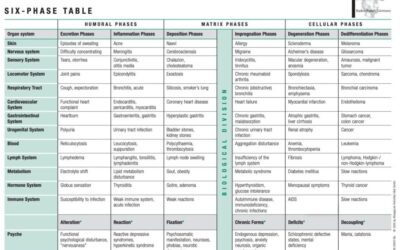
I discussed the trial of ablation and monitoring subsequent AFIB episodes with the patient, and she agreed to try supportive supplementation for atrial fibrillation. The patient was also taking strontium in a multi-nutrient supplement for osteoporosis, and this was debated due to the role of strontium in thromboembolic disease. Some evidence supports that strontium ranelate contributes explicitly to an increased risk of thromboembolic events or diseases, but this is discussed in the literature.4 Hypothyroidism did not seem to be a trigger for episodes as it remained controlled throughout, and hyperthyroidism is known to be more widely associated with the risk of atrial fibrillation episodes6. We discussed a trial of low-dose herbs if ablation did not manage arrhythmia. The patient had a CHADVASC score of 4, 4.8% stroke risk, and 6.7% risk of stroke/TIA/thromboembolism, categorizing her as moderately high risk for stroke.3 Magnesium taurate 250mg daily was prescribed to promote relaxation of cardiovascular muscle tissue, rate and rhythm control, and be more consistent with taking CoQ10 100mg daily. Magnesium also plays a vital role in coagulation regulation.5 Magnesium sulfate, particularly in IV form, has been studied more in patients with atrial fibrillation and has shown positive outcomes on HR during and after episodes.1 Magnesium taurate was chosen as it helps explicitly with mechanisms relating to HTN and is an integral part of the antioxidant defense system of the myocardial tissues.7
Herbal Support Post-Ablation
The patient underwent ablation and did well for around three months but was experiencing significant fatigue. I had the patient complete a blood pressure log, and blood pressure was averaging 150 systolic despite three medications to control. Her PCP trialed amlodipine as the fourth controller, but the patient experienced the common side effect of ankle edema and did not wish to continue. The patient also became increasingly concerned about apixaban use as she began to experience hematuria. Underwent a full work-up with nephrology and urology, and they determined this could be due to scarring from prior rectal cancer treatment. I urged the patient to speak with her cardiologist about lowering the dose of apixaban as she was also experiencing persistent epistaxis and nearly met the cut-off for weight and age to support a lower dose of anticoagulant for stroke prevention.2 ¼ teaspoon once daily of Crataegus spp. (hawthorn) solid extract was prescribed to help lower blood pressure and support the general tone of the cardiovascular system as, over time, this has become the central weakened system for this patient, exhibited by treatment-resistant hypertension despite four controller medications.
In about one month, the patient’s primary care physician weaned her off of sotalol, but HR began to fluctuate from 60 to 80 bpm. Her physician wanted to watch and wait before switching to another beta-blocker. Blood pressure had been slightly improving on hawthorn solid extract, so the dose was increased to ½ teaspoon twice daily.
It was well managed for several months until new episodes of afib recurred. She saw a cardiologist who wanted her to complete the WATCHMAN procedure instead of anticoagulants and to go back to taking sotalol. She deferred this as it helped her HR but not HTN. BP had been in good range with hawthorn with no readings over 150 systolic, apart from one or two isolated incidents. The only trigger she can think of for Afib was increased caffeine and minor alcohol use on a trip. I noticed constipation triggered transient episodes, more so at night when waking. Her PCP refused to prescribe anticoagulant once daily as she was 2kg below the weight requirement and 1.5 below the age requirement for once-daily dosing. I discussed extensively the use of low-dose botanicals to manage afib episodes with the patient, including risks, side effects, and dosing strategies.
Due to the patient’s age, a conservative approach was utilized with minimal low-dose botanicals to achieve the effect. Therapeutic goals for the formula were to regulate rate and rhythm, relax and tonify the cardiovascular system, decrease palpitations, and soothe the nervous system. Herb-drug interactions were taken into consideration, as no pharmaceuticals were prescribed that interfered with the QT interval; all herbs were safe to prescribe. Leonurus cardiaca is contraindicated with these medications.8 A two-ounce tincture was dispensed containing 23 milliliters of Tilia cordata leaf extract, 15 mL of Crataegus spp leaf and berry extract, 2 mL of Selenicereus grandifloras root extract (1:1.8; night-blooming cactus) and 21 mL of Leonurus cardiaca leaf extract. The prescribed dose was three dropperfuls (approximately 3 mL) at the onset of the episode and three additional dropperfuls up to two times daily as needed. When prescribing low-dose botanicals, it is important to provide a maximum dosage for patient safety and to calculate beforehand the maximum dose of low-dose herbs the patient will receive. The dose per day of Selenicereus given was 6.75 drops daily, whereas the maximum dosage for this plant at 1:1 is 60 drops per day. Gentle cardiovascular nervines and antiarrhythmics were chosen to support the low-dose botanical Selenicereus.
The patient’s HR was easier to maintain during the day, and she could more easily transition out of episodes after the first use. After subsequent use, the patient reported faster resolution of episodes and less bothersome episodes of atrial fibrillation. This case highlights the necessity and utility of low-dose botanicals in cardiovascular pathologies. With careful attention to herb-drug interactions, low-dose botanicals can make for excellent adjunctive care to treatment-resistant atrial fibrillation or atrial flutter. Naturopathic physicians should continue to expand and educate themselves on the proper usage of low-dose botanicals as we see more and more patients with treatment-resistant pathologies. Botanicals work synergistically with the body in ways medications simply cannot and offer more complex action to cover difficult-to-understand etiologies.

Dr. Mele is a graduate of Bastyr University in Seattle, WA where she earned a Doctorate of Naturopathic Medicine in 2021, completing two years as a Resident Physician at the Sonoran University Medical Center in 2023 where she now teaches Naturopathic Philosophy. Her undergraduate degree is in Environmental and Geological Sciences. Dr. Mele currently is a co-owner of Aspen Integrative Medical Center in Flagstaff, Arizona, with her husband and fellow ND, Dr. Paul Despres. Dr. Mele honors the vitalist traditions of naturopathic medicine while intertwining evidence-based clinical practice. She has a strong passion, interest and training in botanical medicine and enjoys working with patients to find their own herbal allies. Botanical medicine is the primary modality Dr. Mele treats with and is a Registered Herbalist with the American Herbalist Guild. Her other treasured modalities of practice are biotherapeutic drainage, complex homoepathy, craniosacral therapy, visceral manipulation and mind-body medicine. Dr. Mele has no disclosures at this time.
References
- Bhatti H, Mohmand B, Ojha N, P Carvounis C, L Carhart R. The Role of Magnesium in the Management of Atrial Fibrillation with Rapid Ventricular Rate. J Atr Fibrillation. 2020;13(4):2389. doi: 10.4022/jafib.2389. PMID: 34950320; PMCID: PMC8691303.
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019 Apr;67(4):674-694. doi: 10.1111/jgs.15767. Epub 2019. PMID: 30693946.
- Chen JY, Zhang AD, Lu HY, Guo J, Wang FF, Li ZC. CHADS2 versus CHA2DS2-VASc score in assessing the stroke and thromboembolism risk stratification in patients with atrial fibrillation: a systematic review and meta-analysis. J Geriatr Cardiol. 2013;10(3):258-66. doi: 10.3969/j.issn.1671-5411.2013.03.004. PMID: 24133514; PMCID: PMC3796700.
- Curtis EM, Cooper C, Harvey NC. Cardiovascular safety of calcium, magnesium and strontium: what does the evidence say? Aging Clin Exp Res. 2021;33(3):479-494. doi: 10.1007/s40520-021-01799-x. Epub 2021 Feb 9. PMID: 33565045; PMCID: PMC7943433.
- Kang WS, Yun HJ, Han SJ, Kim HY, Kim DK, Lim JA, Woo NS, Kim SH. The effects of magnesium on the course of atrial fibrillation and coagulation in patients with atrial fibrillation undergoing mitral valve annuloplasty. Korean J Anesthesiol. 2011;61(3):210-5. doi: 10.4097/kjae.2011.61.3.210. Epub 2011 Sep 23. PMID: 22025942; PMCID: PMC3198181.
- Kim EJ, Lyass A, Wang N, Massaro JM, Fox CS, Benjamin EJ, Magnani JW. Relation of hypothyroidism and incident atrial fibrillation (from the Framingham Heart Study). Am Heart J. 2014;167(1):123-6. doi: 10.1016/j.ahj.2013.10.012. Epub 2013 Oct 19. PMID: 24332151; PMCID: PMC3868014.
- Shrivastava P, Choudhary R, Nirmalkar U, Singh A, Shree J, Vishwakarma PK, Bodakhe SH. Magnesium taurate attenuates progression of hypertension and cardiotoxicity against cadmium chloride-induced hypertensive albino rats. J Tradit Complement Med. 2018; 9(2):119-123. doi: 10.1016/j.jtcme.2017.06.010. PMID: 30963046; PMCID: PMC6435948.
- Yarnell, Eric. Herbs for Atrial Fibrillation. Alternative and Complimentary Therapies. 2017 23(3): 102-111. DOI: 10.1089/act.2017.29114.eya