J.V. Wright, D.J. Zeoli, ND, LAc, and J. Sherman
A prospective study evaluating the effectiveness of vitamin B12 for acute and chronic bursitis and its surprising connection to low stomach acid
Abstract
The objective of this study is to evaluate the effect of using vitamin B12 injections on people with symptoms of joint pain and loss of function associated with acute and chronic bursitis. Also, the study was intended to identify any connection between bursitis and decreased stomach acid secretion, since proper vitamin B12 absorption depends so highly on the intrinsic factor secreted by the parietal cells of the gastric mucosa.
Forty patients with bursitis were recruited into the study, many of whom had been previously treated by conventional methods without success, and instructed on proper self-injection technique so that they could administer once daily vitamin B12 injections.
Outcome measures included the Arthritis Impact Measurement Scale, joint range of motion measurements, subjective reporting, erythrocyte sedimentation rate, C-reactive protein, uric acid, complete blood count, and general chemistry.
At the end of the study, participants were categorized into one of three groups depending on the objective and subjective measures of symptom relief. Twenty of the 37 individuals who had completed the study were considered “Greatly Improved” and had reported complete relief or near complete relief of all bursitis symptoms. Twelve of the 37 participants were considered “Moderately Improved” because the frequency and severity of their symptoms substantially decreased but did not entirely resolve. Finally, five out of the 37 participants were grouped as “No Change” since the therapy did not seem to affect either objective measures or subjective reporting of symptoms significantly. No one in the study reported worsening of symptoms—objective measures correlated with subjective reporting of symptom relief.
Arthritis Impact Measurement Scale values improved by 6-fold in the “Greatly Improved” group (p<0.005) and 3-fold in the “Moderately Improved” group as compared to the “No Change” group. Objective range-of-motion measurements improved by 100% in the “Greatly Improved” group (p<0.05) and 50% in the “Moderately Improved” group, as compared to those in the “No Change” group.
Results of Heidelberg testing showed that 55% of those in the “Greatly Improved” group had moderate to severe hypochlorhydria, 50% of those in the “Moderately Improved” group had moderate to severe hypochlorhydria, and none of those in the “No Change” group had moderate to severe hypochlorhydria.
This study demonstrates the effectiveness of intramuscular injections of vitamin B12 in the treatment of bursitis. Vitamin B12 decreased and eliminated the pain associated with bursitis, increased joint range of motion, reduced inflammation, and improved blood chemistry results. A connection was also established between hypochlorhydria and bursitis.
Introduction
The pain and loss of joint mobility associated with bursitis are common presenting symptoms in clinical practice. Inflammation of the fluid-filled bursae sacs, which surround the large joints, can be triggered by repetitive motions as well as traumatic injury. Symptoms include pain on movement, pain caused by pressure, pain lying on the affected joint, swelling, and stiffness. For many people, bursitis can be a recurring condition. After resolution of the initial acute event, the symptoms of bursitis can linger at a low level for years. Individuals with a tendency towards bursitis can have repeat attacks after vigorous exercise or overwork. Standard medical treatments include rest, ice, NSAIDS, and in some cases, cortisone injections or surgery.
In the 1950s, Dr. Klemes studied the effects of intramuscular injections of vitamin B12 on patients with acute subdeltoid bursitis. He published a research article in 1957 in which 40 patients with acute bursitis of the shoulder received injections of 1000 mcg vitamin B12 daily for seven to ten days, then three times per week for several weeks.1 Thirty-seven of the patients improved with rapid pain relief and decreased intensity of subjective symptoms. Many patients reported complete relief within a few days. Some individuals in the study with radiological evidence of calcification of the bursa showed decreased levels of calcium deposits on follow-up x-rays.
Dr. Jonathan Wright revived this simple and effective treatment for bursitis in the 1980s and has been in use at his clinic ever since. Patients at Dr. Wright’s Tahoma Clinic have responded to treatment in a way similar to those investigated in Dr. Klemes’ article.2 In addition to acute bursitis of the shoulder, vitamin B12 injections have been successful in treating chronic bursitis, as well as bursitis of the hip, elbow, and knee. The majority of patients respond to therapy within two weeks, but others may require injections for three or four weeks before noticing any improvements. Dr. Wright has made the additional discovery that individuals with bursitis who respond to vitamin B12 injections often have the co-morbid condition of hypochlorhydria or achlorhydria. Since the proper functioning of the parietal cells of the gastric mucosa is necessary for both the production of stomach acid and intrinsic factor, hypochlorhydria or achlorhydria can be a precursor to a vitamin B12 deficiency. This topic takes on additional relevance with the widespread use of proton pump inhibitor drugs.3,4
The current study was launched to investigate further the clinical results that have been observed by the relatively small number of doctors who have been using vitamin B12 injections as a treatment for all kinds of bursitis. To assess the effectiveness of daily intramuscular injections of vitamin B12 on the relief of bursitis symptoms, we have conducted this two-month study on newly recruited patients. Many of the subjects had been previously diagnosed with bursitis and had received conventional treatment without lasting effect. All of the subjects were treated, and there was no placebo group.
Materials & Methods
Forty patients were enrolled in our study, most of whom responded to our in-house flyers, website link, and radio show announcements. These were selected from a group of about sixty individuals who applied for entry. All of the subjects were screened for current symptoms of bursitis through medical interview and physical examination. Many of the participants were previously diagnosed with bursitis. All of the subjects had previously tried some type of conventional treatment without lasting effects. Our inclusion criteria were: 1) previous diagnosis of bursitis or new diagnosis based on clinical findings; 2) current symptoms of active bursitis; 3) bursitis of the shoulder, hip, elbow, or knee; 4) not currently taking vitamin B12 injections. Exclusion criteria were: 1) pregnant; 2) liver disease; 3) currently taking prednisone or corticosteroid medications; 4) joint symptoms which could be better classified under a different diagnosis.
Our two-month study included a total of five visits to our clinic and laboratory facility. The first visit was meant to identify potential candidates using a complete medical history, physical examination, joint range of motion measurements with a goniometer, and completion of the Arthritis Impact Measurement Scale version 2 (AIMS2). Those accepted into the study were invited back for a second visit in which a Heidelberg Test was performed to assess stomach acid production levels. A fasting SMAC blood test was drawn at this time, including complete blood count (CBC), electrolytes, iron panel, uric acid, erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), hemoglobin A1C, lipid panel, SGOT, SGPT, GGT, and glucose. Each participant was instructed on the proper method of self-injection before leaving the clinic and given two 30ml vials of cyanocobalamin and sixty syringes with needles.
During the third, fourth, and final visit, each subject was given a follow-up interview and examination. Range of motion measurements were repeated, and the AIMS2 was re-administered. At the final visit, a second identical SMAC blood test was drawn.
The dosage of cyanocobalamin was 1000 mcg, injected intramuscularly once per day for sixty consecutive days. Subjects were required to complete a log sheet noting the time of injection and to return their empty vials after the study. Subjects were allowed to continue any medications or supplements that they had been previously taking. There were three participants who did not comply with the injection frequency, and their results are not included in the study.
Results
The most dramatic result observed in the study was the subjective relief of bursitis symptoms reported by many of the participants. Figure 1 shows the number of subjects who subjectively reported that they had experienced some degree of symptom relief, such as decreased pain or increased joint mobility. Each participant was given a medical interview at every clinic visit and asked about any changes that they may have experienced regarding their bursitis symptoms. At the first visit, all participants were experiencing symptoms of bursitis. Two weeks later, 20 participants reported a decrease in their symptoms, ranging from mild improvement to complete relief. These participants reported the same or increased improvements at four weeks and eight weeks. An additional 7 participants noted improvements at the four-week interview date. These improvements lasted at least until the end of the study, four weeks later, bringing the total number of subjects reporting improvements to 27. On the final 8-week follow-up visit, five additional participants reported that their bursitis symptoms had decreased, for an overall total of 32. The number of participants who reported that their symptoms were greatly improved increased from 3 to 12 between the second and fourth week, and increased from 12 to 20 between the fourth and eighth week. The color coding in the figure illustrates these changes.
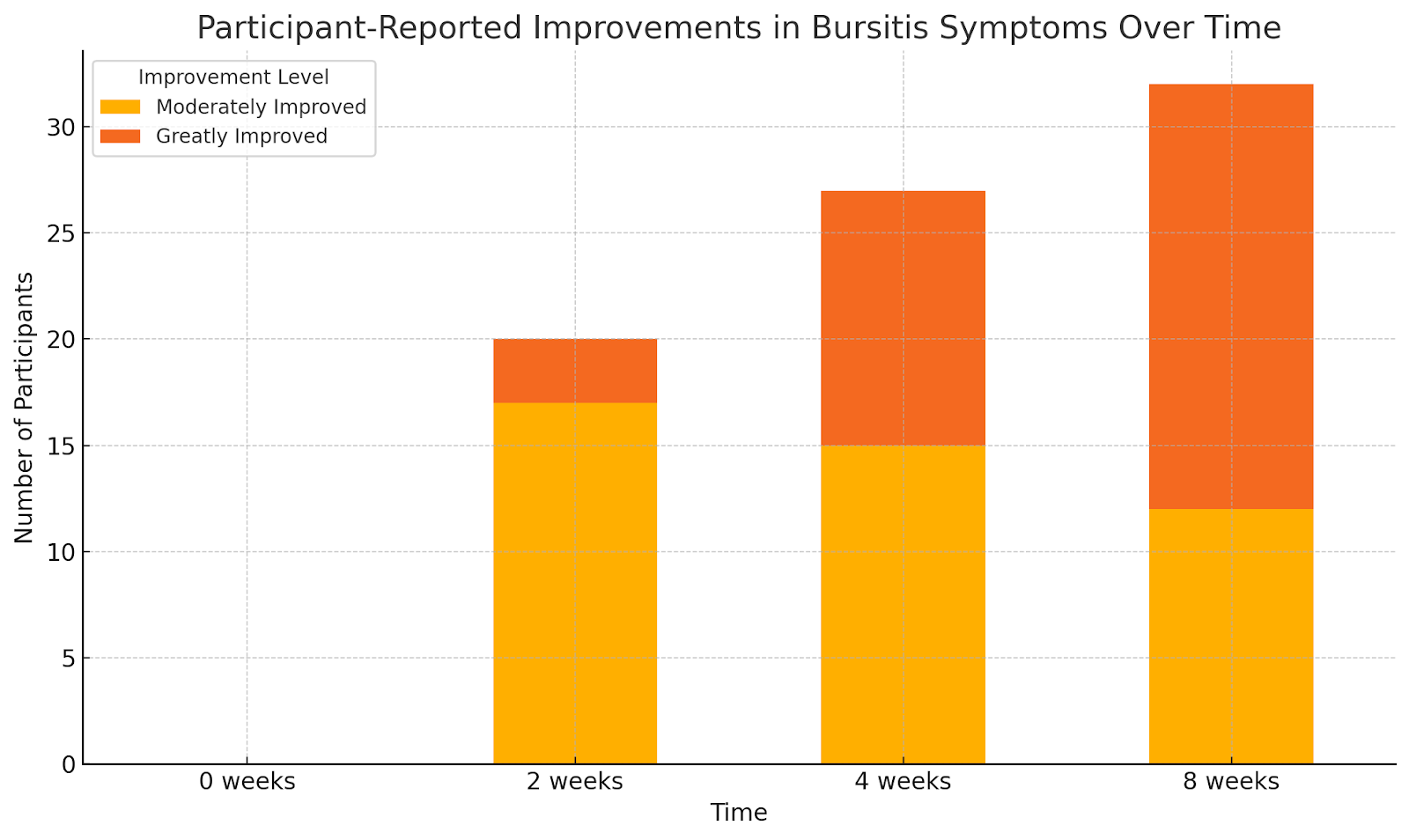
Figure 1: Number of participants reporting subjective improvements in bursitis symptoms at 0 weeks, 2 weeks, 4 weeks, and 8 weeks. Those reporting that they were greatly improved are shown in red, and those reporting mild to moderate improvements are shown in blue.
The second most important result is the significant objective improvements that were observed in the AIMS2 questionnaire values. Each participant was grouped into one category at the end of the study. The first group was labeled “Greatly Improved” and included those who reported that they had experienced great improvements in their bursitis symptoms.
Those who were considered “Greatly Improved” had complete relief or near complete relief of their bursitis symptoms. The second group was labeled “Moderately Improved” and included the participants who had experienced partial relief of symptoms. The people belonging to the “Moderately Improved” group had a considerable improvement in joint mobility and pain relief, but not a complete remission. Finally, some experienced no changes and were counted into the “No Change” group.
Figure 2 shows the average improvements in the AIMS2 questionnaire scores of each group, comparing the results at the final visit with those from the first visit. Participants in the “Greatly Improved” group increased their AIMS2 score by 50 points on average over baseline. Those in the “Moderately Improved” group increased their AIMS2 score by an average of 24 points over baseline. Subjects in the “No Change” group saw a 9-point average increase in AIMS2 scoring. Using a T-Test analysis, the difference between the improvement in the “Greatly Improved” group compared to the “No Change” group was shown to be statistically significant (p<0.005). However, the difference in improvement between the “moderately improved” and “No Change” groups was not statistically significant.
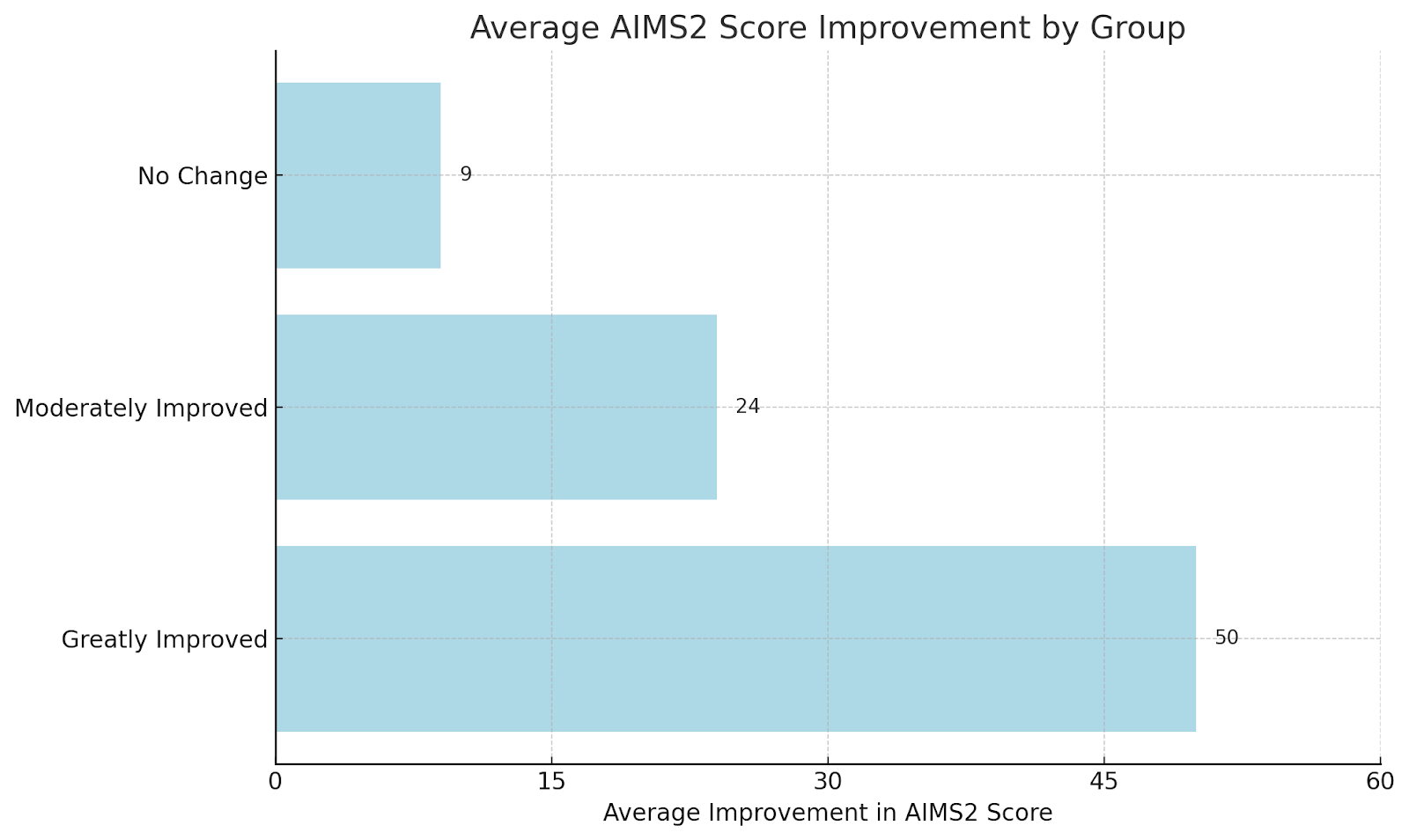
Figure 2: Average improvement in AIMS2 score for each group, comparing initial testing with final testing.
The third result that was observed in this study was a dramatic improvement in total joint range-of-motion measurements in those responding to the treatment. Joint range-of-motion measurements were obtained before treatment and at every subsequent visit during the treatment phase of the study. The joints measured included shoulders, hips, knees, neck rotation, wrists, and metacarpal-phalangeal joints for a total of twenty measurements.
Figure 3 shows the average improvements in total joint range-of-motion that were observed in all of the subjects. Those in the “Greatly Improved” group improved their range-of-motion measurements an average of 203 points over baseline. Subjects in the “Moderately Improved” group improved their range-of-motion measurements an average of 154 points over baseline. In the “No Change” group, the average improvement was 100 points. Using a T-Test analysis, the difference in improvement between the “Greatly Improved” group and “No Change” group was shown to be statistically significant (p<0.05). However, the difference between the “Moderately Improved” and “No Change” group was not statistically significant.
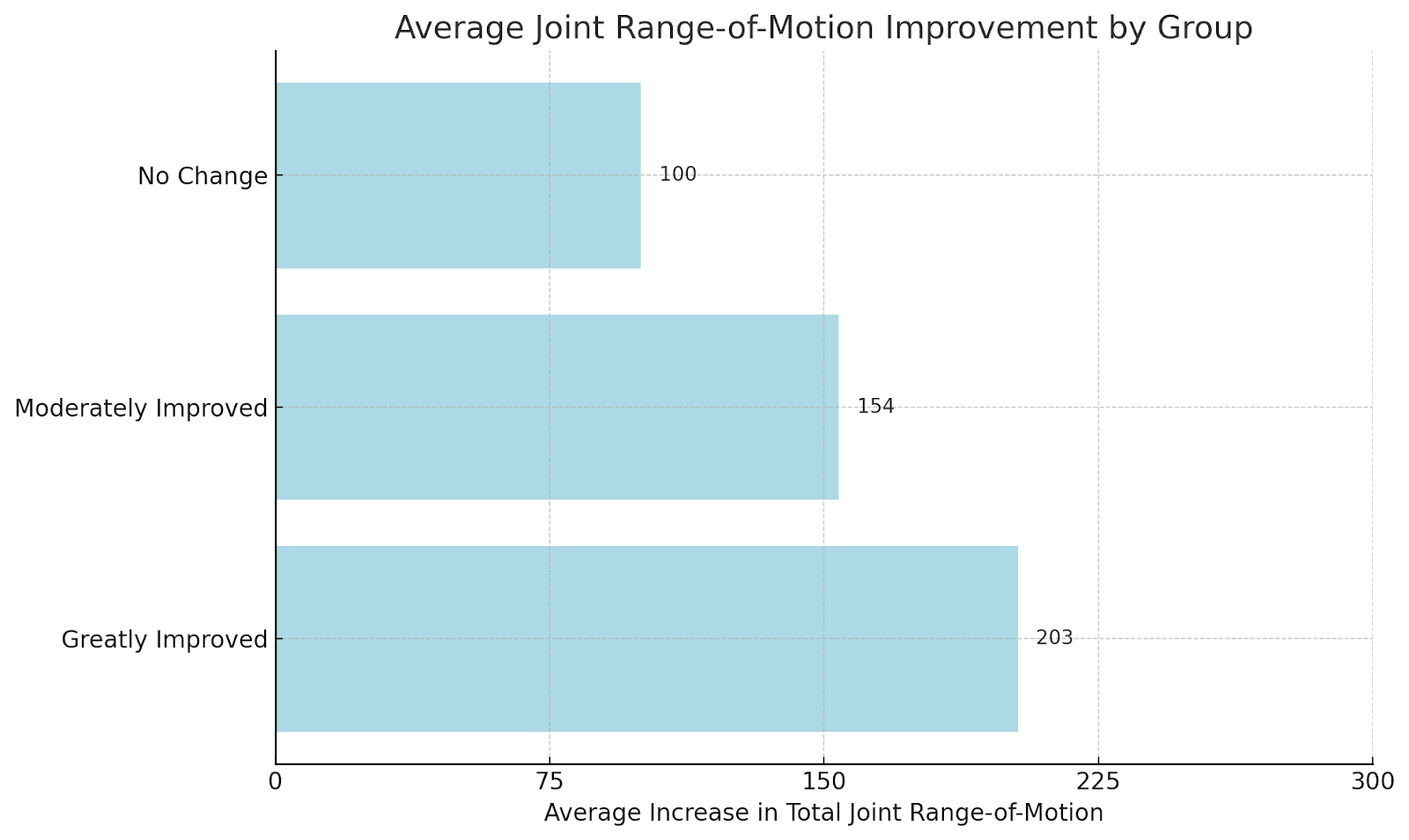
Figure 3: Average increase in total joint range-of-motion measurements, comparing initial evaluation with final evaluation
The fourth result that was observed in the study was a correlation between hypochlorhydria and symptoms of bursitis. A Heidelberg stomach acid evaluation was performed on each participant in the study. Those individuals who had improvements from taking the vitamin B12 injections also had the lowest stomach acid levels. In the Greatly Improved group, 55% of the participants had some degree of hypochlorhydria, including four people with moderate hypochlorhydria, six people with severe hypochlorhydria, and one person with achlorhydria. In the Moderately Improved group, 67% of the participants had some degree of hypochlorhydria, including two people with mild hypochlorhydria, two people with moderate hypochlorhydria, three people with severe hypochlorhydria, and one person with achlorhydria. In the No Change group, only one person had mild hypochlorhydria. Figure 4 shows a summary of these test results.
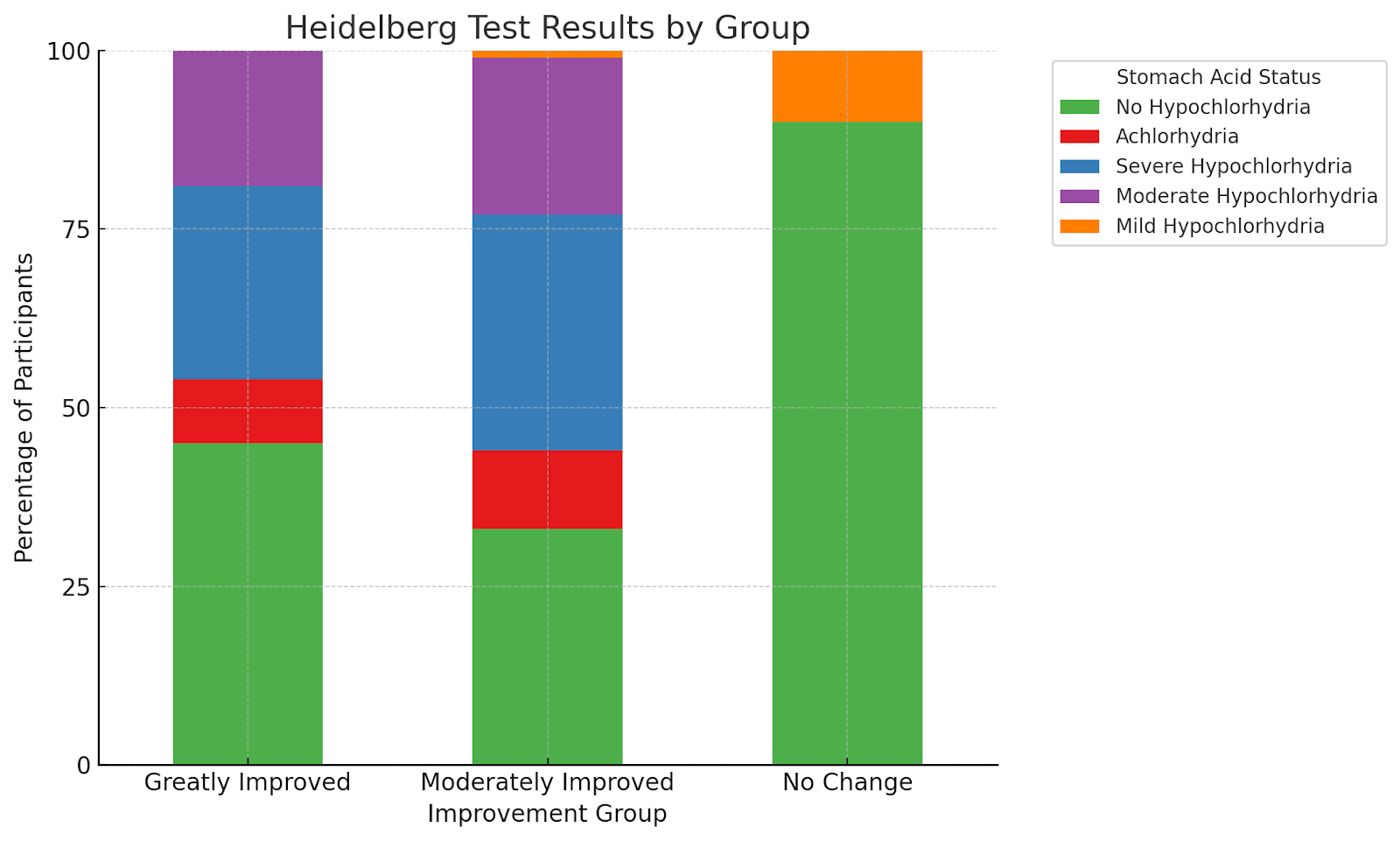
Figure 4: Summary of Heidelberg Test results arranged according to group.
Finally, we found two trends regarding changes in blood work. There were six individuals who began the study with elevated serum uric acid levels. On repeat testing after treatment with vitamin B12, these elevated levels returned to normal. However, there were also two people who began the study with normal serum uric acid levels who noticed an increase on repeat testing at the end of the study. There were two individuals with an elevated C-reactive protein at the beginning of the study. Both individuals had a normal reading on repeat testing at the end of the study. It is interesting to note that none of the participants had an elevated mean corpuscular volume (MCV) or mean corpuscular hemoglobin (MCH) at the beginning of the study.
Discussion
This study provides objective clinical evidence to support the previously observed results that daily intramuscular vitamin B12 injections are an effective and safe treatment against bursitis. More than half of the participants had complete relief of their bursitis symptoms by the end of the study, while an additional 25% of the subjects had noticed some degree of benefit from the therapy. Pain levels were significantly reduced and eliminated. Joint range of motion increased significantly according to both subjective and objective measures.
Inflammation was reduced, and proper functioning was restored. The results that are recorded in the present study are consistent with those first recorded by Dr. Klemes over 50 years ago. They are also consistent with the clinical experiences of Dr. Wright and other physicians at the Tahoma Clinic. Cyanocobalamin appears to be well tolerated at this dosage. There were no reports of any side effects other than temporary mild tenderness at the site of injection. Rather, participants tended to report “side benefits” such as increased energy, improved mood, a decrease in psoriasis rash, and a decrease in asthma symptoms.
Another important result of this study is the evidence connecting bursitis with low stomach acid levels. Half of the participants in the study had some degree of hypochlorhydria. The “Greatly Improved” group had the highest percentage of individuals with moderate to severe hypochlorhydria. It makes sense that low stomach acid can be a precursor to a vitamin B12 deficiency, since the acid-producing parietal cells of the gastric mucosa also produce intrinsic factor. However, the connection between hypochlorhydria and bursitis has not previously been demonstrated through research. A review of the literature revealed that prior studies have made a connection between vitamin B12 deficiency and loss of bone mineral density.5,6 This could possibly be explained through the common mechanism of hypochlorhydria, since another function of stomach acid is the preparation of dietary minerals for absorption. Still, it does not explain why treatment with vitamin B12 alleviates bursitis symptoms.
Acknowledgement
The authors would like to thank Melanie Grimes and the Knowledge Medical Research Charitable Trust for their generosity in funding this research study, and Dr. Irving S. Klemes for his work in discovering and promoting the use of vitamin B12 against bursitis.
Jonathan V. Wright, MD, is a Harvard- and University of Michigan–trained pioneer in natural medicine and bio-identical hormone therapy. Known as “The Father of Bio-Identical Hormone Replacement,” he introduced tri-estrogen cream and developed safety protocols now widely used. Since founding the Tahoma Clinic in 1973, he’s advanced treatments for asthma, macular degeneration, hearing loss, UTIs, and more. A prolific author and international lecturer, Dr. Wright has published extensively and helped shape integrative medicine policy following the 1992 FDA raid on his clinic. He was inducted into the Orthomolecular Hall of Fame in 2012 for his lifelong contributions.

Dr. David Zeoli graduated from the five year dual-degree program at the National College of Naturopathic Medicine in Portland, Oregon with a doctorate in naturopathic medicine and a master’s degree in Oriental Medicine. He has been in practice for over 25 years at various clinics. He currently practices in Chehalis, Washington.

Dr. John Sherman brings over 45 years of naturopathic experience to Tahoma Clinic, specializing in bio-identical hormone therapy, cardiovascular issues, autoimmunity, cancer support, and individualized nutrition. He formerly served as Clinic Director at Bastyr University and as an associate professor at both Bastyr and NUNM. Dr. Sherman co-authored Alternative Medicine: The Definitive Guide and authored The Complete Botanical Prescriber. He holds degrees in Human Biology and Business Administration from Carnegie Mellon. A former host of The Green Medicine Radio Show, he now edits the Green Medicine Newsletter. He consults for Meridian Valley Lab, advising physicians on functional lab analysis and patient care.
References
- Klemes, I.S. Vitamin B12 in acute subdeltoid bursitis. Ind Med Surg. 1957 Jun;26(6): 290-2.
- Wright, J.V. Erase Bursitis Pain in One Month or Less. Dr. Jonathan V. Wright’s Nutrition & Healing, Vol. 17, issue 3, May 2010
- Rozgony N.R., et al. Vitamin B(12) deficiency is linked with long-term use of proton pump inhibitors in institutionalized older adults: could a cyanocobalamin nasal spray be beneficial? J Nutr Elder. 2010 Jan;29(1):87-99.
- Dharmarajan T.S., et al. Do acid-lowering agents affect vitamin B12 status in older adults? J Am Med Dir Assoc. 2008 Mar;9(3):162-7.
- Dhonukshe-Rutten R.A., et al. Low bone mineral density and bone mineral content are associated with low cobalamin status in adolescents. Eur J Nutr. 2005 Sep;44(6):341-7.
- Dhonukshe-Rutten R.A., et al. Vitamin B-12 status is associated with bone mineral content and bone mineral density in frail elderly women but not in men. J Nutr. 2003 Mar; 133(3):801-7.