Christopher Knee, ND, MSc
The prevalence of overweight and obesity has increased dramatically in recent decades. Currently, about 34% of adults in the United States are considered obese (body mass index; BMI > 30.0 kg/m2),1 with a combined estimate of 65% being overweight (BMI 25.0–29.9 kg/m2) or obese.2 Prolonged caloric restriction (CR), without malnutrition, and regardless of macronutrient ratio,3 is the most effective means for body weight reduction and maintenance, and has been associated with a myriad additional health benefits, including: extended mean and maximal life span; delayed onset of cancer; reduced cardiac risk factors; improved insulin sensitivity and lipid parameters; and improved mitochondrial function through reduced oxidative damage and enhanced cellular autophagy .4
However, long-term compliance for CR is notoriously poor for most individuals, as evidenced by an extremely high failure rate (95%) of most popular diets, perhaps due to an evolutionary mechanism to defend against body weight change.4 Only in more recent years have researchers begun to explore the physical, mental, and emotional factors involved in CR and other forms of food restriction or abstinence, such as intermittent fasting (IF). Additionally, emerging evidence has suggested that, especially in overweight and obese individuals, difficulty with CR may be explained by both physiological and psychological disturbances in food intake regulation and reward pathways, similar to that of substance abuse or addiction.5 Mindfulness interventions have been shown to be effective for a variety of disorders, such as depression, anxiety, stress, cravings, substance abuse, and more recently, “food addiction.”6 The purpose of this article is to briefly outline the metabolic, nutritional, and psychological factors involved with food intake behaviors, and explore the concept of food addiction in the context of CR, IF, and mindfulness-based interventions.
Physiological and Psychological Effects of Caloric Restriction
Food and eating are necessary for human survival; however, caloric consumption above daily requirements for energy has contributed significantly to the development of overweight and obesity.7 Given the low long-term compliance of traditional CR diets, alternative forms of CR, such as IF and alternate-day fasting (ADF), have become increasingly popular in the media and among researchers. While evolutionary demand for energy may motivate food intake, it has also been suggested that historical lack of food availability for brief periods may have allowed for adaptation to food restriction, which is relatively uncommon in the modern human diet involving regular meal intervals.8 A growing body of evidence indicates that fasting for brief periods may trigger similar mechanisms as CR, and may allow for improved compliance.1,4 Much of the research on IF has involved obese individuals, demonstrating an approximate 5-6% reduction in body weight after 8 to 12 weeks, as well as improved parameters of blood lipids and adipokine levels, with very high compliance rates (98%); however, recent evidence has shown both weight loss and cardioprotective effects of ADF in normal and overweight individuals as well.9
Classically, fasting has been defined as a partial or total abstention from all foods, or a select abstention from prohibited foods, but including energy-containing liquids, for a specified period of time.5 This has typically been achieved through ADF (alternating between 100% and 25% of energy intake needs each day, typical of a 2000 cal/d diet), or modified diets such as “5:2” (partially-reduced caloric intake – usually to 20% of energy needs – on 2 days per week)1 and “Eat Stop Eat” (complete caloric restriction for 24 hours, once or twice weekly).10
In the context of weight loss, the mechanism for CR and IF follow basic biochemical pathways: During periods of reduced energy intake, plasma glucose is utilized first for fuel, followed by liver glucose stores (through glycogenolysis), then mobilization of fatty acids from adipose tissue, and, finally, hepatic gluconeogenesis with concomitant ketone formation for essential organs such as the brain, in the event that glucose can no longer be produced.5 Contrary to popular belief, the intermediate phase of “starvation” (with onset of physiological ketosis), may not occur until 48-72 hours into a zero-calorie fast.5 Additionally, human growth hormone (HGH) has been shown to increase during fasting, and acts to inhibit insulin while directly stimulating lipolysis.5 Ultimately, it is this mobilization of fatty acids from adipose tissue, for utilization by skeletal muscle, the liver, and heart, that will allow for sustained weight loss.5 Since most individuals undertaking a CR diet cannot remain compliant, one may theorize that IF may allow for this similar degree of fatty acid mobilization, if performed for periods up to 48 hours. Of course, any CR or IF diet should revolve around quality, nutrient-dense food choices, and regular exercise.
Food Frequency and Meal Timing
Typically, resistance surrounding the acceptance of IF diets relates to widely-held beliefs about metabolism, glucose regulation, and factors driving food intake. The frequency and timing of food intake is greatly influenced by psychological, sociological, and cultural factors; however, evidence to date surrounding the ideal frequency of meal consumption for weight management is largely inconclusive.2 For example, increasing meal frequency (but not total caloric intake), does not appear to significantly improve body composition, nor does it enhance diet-induced thermogenesis, total energy expenditure, or resting metabolic rate.2 Further, skipping meals such as breakfast does not necessarily lead to overconsumption later in the day, as is commonly argued.11 In another study, obese adults limited energy intake to 25% of needs (500 cal/d) on alternate fasting days, while showing no hyperphagic response on feed days, and an overall net caloric reduction of 37%.1 Subjects in this study became habituated to the diet (felt very little hunger on fast days)after approximately 2 weeks, and were able to maintain daily physical activity level (as measured by pedometer) throughout the duration of the 8-week study.1 However, increased meal frequency may reduce hunger and improve appetite control, which may become relevant in the context of food addiction.
Following an IF diet may affect food frequency and meal timing, especially in the context of a 24-hour fast, during which traditional breakfast and lunch meals are skipped (for example, a fast that begins at 6:00 PM one evening, and is broken at 6:00 PM the next evening). There is a general consensus that breakfast is “the most important meal of the day” with regards to health, wellbeing, and cognition; however, evidence to date mostly fails to illustrate metabolic and nutritional specifics.12 This is further complicated by evidence suggesting that CR and IF, as a whole, over time, help to improve neuroprotection and cognition.12 In adults, deviation from habitual meals seems to – easily, in some cases – negatively affect mood; therefore, in the absence of metabolic proof that IF is physiologically harmful short-term, one may infer a more psychologically-dominant mechanism preventing sustainable CR.
It should be noted, however, that there is some evidence to suggest a negative effect of meal-skipping on glucose regulation.4 Intermittent fasts over a period of days have typically been shown to improve glucose tolerance; however, research comparing isocaloric diets of 1 meal per day (OMD) to 3 meals per day (TMD) have found OMD subjects to have higher morning fasting plasma glucose levels, and delayed insulin response on an oral glucose tolerance test (OGTT).13 To most clinicians, and in this author’s opinion, there appears to be an opportunity here, whereby, so long as glucose regulation is monitored throughout any dietary restriction regime, IF in the form of ADF or 24-hour fasts may be a safe and effective means for, at the very least, exploring the patient’s psychological relationship with food in an attempt to gather information and awareness in the form of “mindful fasting.”
Evidence for Food Addiction
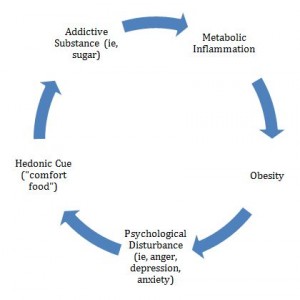
There is increasing evidence to suggest that food-intake behaviors, especially in the context of binge-eating disorder (BED), may be related to addiction and substance abuse via highly palatable components of modern food, namely sugar, salt, and food additives.14 Food intake is regulated by both homeostatic (motivation to eat from a sense of reduced energy stores) and hedonic (reward-based desire to eat) pathways.15 Eating in the absence of perceived hunger has been studied in both children and adults, and appears to result in increased body weight, regardless of whether subjects are exposed to a 1000 or 10 000-cal meal.16 The neurochemical changes seen in obesity and food addiction have been compared to those for cocaine and opioid addictions17; sugar, for example, has been shown to stimulate 2 classic neurotransmitters (dopamine and mu-opioids) involved with addiction, and may be at the forefront of the development of “glucolipotoxicity,” diabetes, and metabolic syndrome (Figure 1).5 Further, adults with BED show greater activation of brain-reward systems, including dopamine activity, when exposed to food stimuli (seeing, smelling, and tasting, without consuming),18 perhaps illustrating an opportunity to increase reward sensitivity through greater awareness of the entire food intake process. Additionally, psychological stress can promote overeating and lead to abdominal obesity through increased cortisol secretion,19 as well as elevated glucose and insulin, and increased inflammatory and oxidative stress processes.20
Figure 1. Proposed Cycle of Weight Gain and Food Addiction
(Adapted from Shriner, 2013)5
While there is currently no medically recognized “food addiction”15 (only a subset of symptoms that can closely yet indirectly be compared to the Diagnostic and Statistics Manual, DSM), and prevalence rates are lacking, it appears that food addiction exists among all weight categories (Table 1),14 though higher in obese individuals, especially women.21 In clinical practice, common subjective symptoms of food addiction may include: persistent desire or repeated unsuccessful attempts to limit food intake; continued intake despite awareness of significant disturbance; or excessive time spent to obtain food, eat, or recover from eating.14 Interested clinicians may wish to peruse the Eating Behaviors Questionnaire (EBQ),14 Yale Food Addiction Scale (YFAS),and Mindful Eating Questionnaire (MEQ),22for additional guidance.
Table 1. Prevalence of Food Addiction by Weight Category
| Weight Category | BMI (kg/m2) | Diagnoses (%) |
| Underweight | < 18.50 | 10.0 |
| Normal-weight | 18.50 – 24.99 | 6.3 |
| Overweight | 25.0 – 29.99 | 14.0 |
| Obese | ≥ 30.00 | 37.5 |
(Data diagnosed by the Yale Food Addiction Scale; from Meule, 2011)14
Mindfulness-Based Interventions
Mindfulness is the deliberate, nonjudgmental awareness of one’s internal processes and external environments.23 Mindful eating, therefore, involves paying close attention to one’s ongoing sensory, cognitive, emotional, and physical experiences throughout the entire act of food consumption.6 Several studies have shown that mindful attention helps prevent impulsive eating behaviors. One recent study19 examined the effects of a mindfulness program for stress eating in 47 overweight and obese women, compared to waitlisted control subjects, over 4 months. Subjects in the mindfulness group experienced reduced anxiety, cortisol, and unchanged body weight (obese individuals only), while obese controls gained weight.19 It should be noted that weight loss was not a primary objective of this study, as there were no instructions given for active caloric restriction; further, the authors stated that the improvements in mindful eating practices may lead to improved weight control and maintenance later on. Mindful eating programs also appear to improve energy intake and glycemic load in type 2 diabetic adults.24
Overall, studies to date suggest that mindfulness exercises involving awareness of hunger cues, selection and portion of food choices, attention to food taste and texture, and the act of eating, are helpful in improving the self-control of food intake.25 Interested readers can find additional resources at The Center for Mindful Eating website (www.thecenterformindfuleating.org), and are encouraged to research the University of Florida’s “Living with Food” program.5
Conclusions
While there are still many uncertainties surrounding the true metabolic, nutritional, and psychological consequences of caloric restriction, intermittent fasting, and food addiction, the intention of this article was to briefly outline the context, and ensure clinicians that short-term (up to 24-hour) food abstinence may be a relatively safe and arguably effective tool for exploring the emotions and behavior surrounding food intake. Mindful eating programs appear to be effective in controlling food addiction and binge-eating-like behavior, and should ultimately be combined with group support or recovery programs, for long-term, sustainable weight management.
 Christopher Knee, ND, MSc is from Ottawa, Ontario, and has a strong passion for health promotion and education. He currently practices in Toronto, Ontario, with a focus on physical medicine, acupuncture, nutritional supplementation, and intravenous (IV) therapy for chronic stress, pain and headaches, athletic performance, and gastrointestinal- and immune-related conditions. He is also a clinical research coordinator for the Canadian College of Naturopathic Medicine, a natural health product industry consultant, and enjoys giving public and corporate health and wellness seminars. Email: info@christopherkneend.com
Christopher Knee, ND, MSc is from Ottawa, Ontario, and has a strong passion for health promotion and education. He currently practices in Toronto, Ontario, with a focus on physical medicine, acupuncture, nutritional supplementation, and intravenous (IV) therapy for chronic stress, pain and headaches, athletic performance, and gastrointestinal- and immune-related conditions. He is also a clinical research coordinator for the Canadian College of Naturopathic Medicine, a natural health product industry consultant, and enjoys giving public and corporate health and wellness seminars. Email: info@christopherkneend.com
References
- Klempel MC, Bhutani S, Fitzgibbon M, et al. Dietary and physical activity adaptations to alternate day modified fasting: implications for optimal weight loss. Nutr J. 2010;9:35.
- La Bounty PM, Campbell BI, Wilson J, et al. International Society of Sports Nutrition position stand: meal frequency. J Int Soc Sports Nutr. 2011;8:4.
- Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859-873.
- Anton S, Leeuwenburgh C. Fasting or caloric restriction for healthy aging. Exp Gerontol. 2013;48:1003-1005.
- Shriner RL. Food addiction: detox and abstinence reinterpreted? Exp Gerontol. 2013;48:1068-1074.
- Papies EK, Barsalou LW, Custers R. Mindful attention prevents mindless impulses. Social Psychological and Personality Science. 2012;3(3):291-299.
- Papies EK. Tempting food words activate eating simulations. Front Psychol. 2013;4:838.
- Dixit VD, Yang H, Sayeed KS, et al. Controlled meal frequency without caloric restriction alters peripheral blood mononuclear cell cytokine production. J Inflamm. 2011;8:6.
- Varady KA, Bhutani S, Klempel MC, et al. Alternate day fasting for weight loss in normal weight and overweight subjects: a randomized controlled trial. Nutr J. 2013;12:146-153.
- Brad Pilon. Eat Stop Eat. Strength Works International Publishing, Inc. EatStopEat Web site. http://www.eatstopeat.com. Accessed February 3, 2014.
- Kral TV, Whiteford LM, Heo M, Faith MS. Effects of eating breakfast compared with skipping breakfast on ratings of appetite and intake at subsequent meals in 8- to 10-y-old children. Am J Clin Nutr. 2011;93:284-291.
- Zilberter T, Zilberter EY. Breakfast and cognition: sixteen effects in nine populations, no single recipe. Front Hum Neuroscie. 2013;7:631.
- Carlson O, Martin B, Stote KS, et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in health, normal weight middle-aged men and women. Metabolism. 2007;56(12):1729-1734.
- Meule A. How prevalent is “food addiction”? Front Psychiatry. 2011;2:61.
- Lutter M, Nestler EJ. Homeostatic and hedonic signals interact in the regulation of food intake. J Nutr. 2009;139:629-632.
- Shomaker LB, Tanofsky-Kraff M, Zocca JM, et al. Eating in the absence of hunger in adolescents: intake after a large-array meal compared with that after a standardized meal. Am J Clin Nutr. 2010;92:697-703.
- Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32(1):20-39.
- Avena NM, Murray S, Gold MS. Comparing the effects of food restriction and overeating on brain reward systems. Exp Gerontol. 2013;48:1062-1067.
- Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;2011:651936.
- Daubenmier J, Lin J, Blackburn E, et al. Changes in stress, eating, and metabolic factors are related to changes in telomerase activity in a randomized mindfulness intervention pilot study. Psychoneuroendocrinology. 2012;37(7):917-928.
- Pedram P, Wadden D, Amini P, et al. Food addiction: its prevalence and significant association with obesity in the general population. PLoS One. 2013;8(9):e74832.
- Framson C, Kristal AR, Schenk J, et al. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009;109(8):1429-1444.
- The principles of mindful eating. The Center for Mindful Eating (TCME) Web site. http://www.thecenterformindfuleating.org/principles. Accessed January 25, 2014.
- Miller CK, Kristeller JL, Headings A, et al. Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr Diet. 2012;112(11):1835-1842.
- Koithan M. Mind-body solutions for obesity. J Nurse Pract. 2009;5(7):536-537.