Marcel J. Hernandez, ND
As a holistic physician, I have always tried to attune to the same mantra I repeat in various forms to my patients: knowledge and prevention. Knowledge in the sense that the biochemical information derived through periodic laboratory blood, urine, and saliva testing provides confirmation of disease-preventing lifestyle choices. So as a baby boomer male, as I entered midlife, I began running biannual PSA tests on myself to monitor any fluctuations that might indicate changes in my prostate health.
In 2001, my PSA was a respectable 1.1. In 2009, it had risen to a surprising 4.9. Most laboratories regard 4.0 as the upper range of “normal.” Moreover, my free PSA, a more reliable screen for prostate cancer, was abnormally very low where it should have been high. Still, all we had was lab indices, not a definitive diagnosis, and as an aging male, a rising PSA was not outside the range of normal.
From my letters to friends and relatives
The usefulness and interpretation of the prostate-specific antigen (PSA) test are under debate by the medical community. In fact, it is trendy to disregard the test entirely. The truth is that the PSA test is extremely useful as a screen that may point the way to the next step in prostate care.
The PSA measurement is a blood test. If you are a man older than 50 years, chances are your physician has already checked your PSA level during a routine examination to determine the potential for prostate cancer. First approved by the Food and Drug Administration in 1986 as a way to monitor treatment of prostate cancer, the PSA test is now widely used as a preliminary screen for the presence of prostate cancer.
Prostate-specific antigen is a glycoprotein that is normally secreted into ejaculate fluid by the healthy prostate. A glycoprotein is a molecule that consists of a carbohydrate bonded with a protein. Almost all key molecules involved in the immune response are glycoproteins.
Prostate-specific antigen is produced by prostate cells and is a normal component of semen. One of the functions of PSA is to aid sperm movement. Another function is to alkalinize the vagina, whose natural acidity is toxic to sperm.
Factors Affecting PSA Test Results
When prostate cancer, benign prostatic hypertrophy, or prostatitis occurs, the normal structure of prostate tissue is disrupted, and considerably more PSA leaks into the bloodstream, resulting in a measurable increase in the serum level of PSA, indicating a potential problem. Interpretation of any rise in serum level of PSA and the cause of the elevation is at the heart of the PSA test debate.
In addition to the aforementioned conditions, other factors may affect the results of a PSA test, including a temporary rise in the PSA level after bicycle riding. Some studies show that ejaculation 1 or 2 days before a PSA test may increase PSA levels in the blood. Consequently, men should abstain from sex (and bicycle riding) for 2 days before a PSA test.
Digital rectal examinations and biopsies of the prostate may also affect PSA levels, although the increase caused by a digital rectal examination is not thought to be significant enough to result in a false-positive test result. A biopsy, however, may elevate PSA levels for as long as 4 weeks.
High serum PSA levels pose no systemic health risks but are an indication that something has caused more PSA than usual to enter the bloodstream from the prostate. However, the PSA test is unable to identify the cause of the elevation. Further clouding the issue and providing fodder for controversy, the reference ranges of what constitute “normal” levels change as men age.
Most physicians agree that a man who has a PSA level exceeding 4.0 ng/mL should seek further testing. However, the prostate typically enlarges as men grow older, causing elevations in serum PSA levels. Age-based reference ranges (Table) are not widely accepted but are more indicative of whether a PSA test result is abnormal. These flexible age-specific PSA levels can assist in decreasing false-positive test results among older men and in increasing prostate cancer detection among younger men.
Interpreting PSA Test Results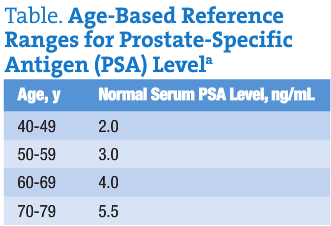
Although prostatitis, benign prostate hyperplasia, and prostate cancer cause the PSA level to rise, the PSA test is used almost exclusively to screen for prostate cancer. However, many men with elevated PSA levels do not have prostate cancer, and not all prostate cancers cause the PSA level to rise.
A study in the New England Journal of Medicine found that up to 15% of 3000 men with PSA levels at or below the established threshold (4.0 ng/mL) and with normal findings on digital rectal examination had prostate cancer. Furthermore, neither the PSA test nor any other test presently available can differentiate between slow-growing vs fast-growing aggressive prostate cancers.
Another way to interpret PSA levels is to look at the rate at which the PSA level changes. H. Ballentine Carter, MD, professor of urology and oncology at the Medical University of South Carolina, Charleston, has published studies demonstrating that an individual’s personal prostate cancer screening program should be implemented according to baseline PSA levels obtained at an early age instead of using a “one size fits all” approach. Carter said that, although PSA levels vary in the presence of prostate cancer and benign prostatic hypertrophy, the “deviation between consecutive PSA measurements relative to elapsed time is distinctively different between the two conditions.”
“Less than 5% of men without prostate cancer have increases in PSA greater than 0.75 ng/mL per year; therefore, an increase greater than this should raise suspicion of prostate cancer,” Carter said. “Accurate interpretation requires at least three measurements at an interval of no less than 6 months and, ideally, 9 months to a year.” “That means it would take almost 2 years to accumulate a good PSA history,” he said, adding that “if more men start having PSA [test] at age 50, it will be reasonable and feasible to do this.”
The American Urological Association (AUA) issued new guidelines on prostate cancer screening and recommends that men 40 years or older should have a PSA test to establish a baseline reading. The AUA also recommends that PSA testing should be individualized, as recommended by Carter, rather than performed as a blanket annual test for any man 50 years or older. According to the AUA, testing at the much earlier age of 40 years instead of the standard 50 years allows more curable cancers to be found sooner. Earlier baseline testing may also allow for less frequent and more efficient testing thereafter.
Ratio of Free to Total PSA
There are other recent developments that seek to clarify the PSA test interpretation dilemma. A new test based on the ratio of free to total PSA has proved to be much more specific for detection of prostate cancer.
This test is based on the fact that most PSA in the blood is bound to protein (glycoprotein, as already discussed), including that produced by cancer cells. However, men with benign prostate enlargement have higher levels of free (unbound) PSA and a higher ratio of free to total PSA. If the total PSA level is abnormal, the ratio of free to total PSA will give an idea of whether the rise is due to benign disease or cancer. Cancer is more likely if the free to total percentage is below 10%. In simple language, the more free PSA a man has, the less likely it is that he has prostate cancer. Prostate biopsy is a likely next step if the free PSA is below 10%. The free to total PSA test is now available and is widely used throughout the United States.
Regardless of the controversy about interpretation of results, the clear benefits to PSA testing are several: (1) An elevated PSA level is the single best predictor of the possible presence of prostate cancer. (2) Prostate-specific antigen testing can detect the possibility of prostate cancer 5 to 10 years earlier than digital rectal examinations. (3) Most prostate cancers that are initially detected with PSA screening are curable.
The bottom line is that PSA levels can have different meanings in different circumstances. Relative to the presence of prostate cancer, the PSA test result by itself is not definitive. Some men with an elevated PSA level do not have prostate cancer, and some cancers detected by the PSA test are too small or too slow growing to be life threatening. A knee-jerk reaction to an elevated PSA level may lead to unnecessary biopsies and anxiety. In fact, a 2004 editorial in the British Medical Journal sized up the value of the PSA test with this comment: “At present the one certainty about PSA testing is that it causes harm.” It is not the test itself that causes harm, of course, but the reaction to the test result. In most cases, an elevated PSA level is not time to act, but it is time to be more cautious than ever.
The best use of the PSA test is as a screen indicating whether further diagnostic procedures, including a free to total PSA test and/or biopsy, are necessary. Risk factors for prostate cancer and previous PSA test results must be factored into the decision-making process.
 Marcel Hernandez, ND, graduated from Bastyr University in 1991. He specializes in men’s health and inflammatory bowel disease. After surgery for prostate cancer in 2009, he began collecting material for a new book, Prostate Cancer: The Definitive Guide for Making the Best Decisions, which is targeted for November 2010 publication. Dr Marcel and his naturopathic partner, Connie, spend their time between their Palo Alto, California, clinic and their Pacific Naturopathic Retreat Center in Honokaa, Hawaii.
Marcel Hernandez, ND, graduated from Bastyr University in 1991. He specializes in men’s health and inflammatory bowel disease. After surgery for prostate cancer in 2009, he began collecting material for a new book, Prostate Cancer: The Definitive Guide for Making the Best Decisions, which is targeted for November 2010 publication. Dr Marcel and his naturopathic partner, Connie, spend their time between their Palo Alto, California, clinic and their Pacific Naturopathic Retreat Center in Honokaa, Hawaii.
References
- Studies about ejaculation and PSA rise.
- New England Journal of Medicine study.
- Studies by Carter advocating baseline PSA measurement.
- AUA guidelines.
- 2004. British Medical Journal editorial.