Concussion Misinformation
MARK HEISIG, ND
A mild traumatic brain injury (mTBI), also known as a concussion, is an injury that has received growing attention from both the media and the public over the past few years. While awareness of public health concerns, like the potential long-term consequences of repetitive head injuries, is generally a good thing, some of the information I hear from patients and the media is often not in agreement with the biomedical consensus on mTBIs. This article will discuss concussion misinformation, how media coverage of chronic traumatic encephalopathy may be fueling concerns about subconcussive events, and how both this misinformation and these amplified concerns may be contributing to a societal level “nocebo” effect surrounding head injuries.
The Basics of a Concussion
There are approximately 3.8 million sport and recreation-related mTBIs per year in the US, with 1-1.8 million of those occurring in children.1 Among high school athletes, there are approximately 400 000 sport-related concussions per year.2 Based on data from the Centers for Disease Control and Prevention (CDC), it is estimated that a traumatic brain injury (TBI) occurs every 15 seconds in the United States.3 Other data estimates that approximately 50% of the global population will sustain at least one TBI in their lifetime, and 70-90% of those will be mild.4 This is a common issue. Add, “History of concussion or head injury?” to new patient intake paperwork and see the stories come forward.
What happens to the brain during an mTBI has been studied and elucidated as the “neurometabolic cascade of concussion,” which can be summarized as: neurons functionally stretch and shear, this deformity leads to excitotoxicity and neuroinflammation, this overstimulation and inflammation is followed by temporary energy and blood flow deficits.5,6 We know that the initial damage is functional because computed tomography (CT) imaging is unremarkable after concussive injuries.7 Furthermore, we know that during the excitatory phase, calcium and glutamate are central to excitotoxicity, and calcium plays a role in the subsequent energy deficit.5,6 Calcium, which has an affinity for mitochondria, floods the mitochondria and impairs oxidative phosphorylation at a time of hyper-glycolytic demand.5,6 Following concussion, research shows the impaired blood flow and impaired oxidative phosphorylation lead to a roughly 20% energy deficit in the first 3-5 days of recovery.8-12 This metabolic deficit takes roughly 22-45 days to normalize in most patients.9-12
Post-injury, a patient’s symptoms may peak after 3-5 days and begin to resolve after 5-10 days.2,9-15 In general, most patients will be ready to fully return to school or work within 2-4 weeks and return to sports within 3-8 weeks.2,9-15 If a patient’s symptoms persist beyond 14 days (adult) or 30 days (child), then they meet the criteria for Persistent Concussion Symptoms (PCS) put forth by the Concussion in Sports Group (CISG).13
Rest May Not Be Best
Concussions are very difficult for patients. There was usually a traumatic injury followed by physical, cognitive, and emotional symptoms that have pulled them from school, work, or teammates. Often there are no significant findings on diagnostic imaging, and many patients will simply be told they most likely sustained a concussion and to go home and rest until their symptoms improve. It can be confusing, and patients are often left to wonder how and when it will be safe for them to resume normal activities. Here is the problem with prescribing rest “until symptoms improve.” Despite this being the recommendation for decades, current evidence suggests that the opposite may be true.
Per the last three concussion consensus statements from 2016-2021, there is insufficient evidence for prescribing strict rest, and strict rest is now being shown to worsen or prolong symptoms after concussion in animal and human studies.2,9-15 “Dark room” and “cocoon therapy” are no longer recommended.2,13,14 An observational study from 2015 came to the slightly humorous conclusion that adolescents who did not listen to their doctor’s recommendations for rest recovered faster than those who adhered to a strict resting protocol.16
Current guidelines recommend 24-48 hours of relative rest before beginning symptom-limited activity, and a prescribed exercise program between days 3-7.2,13,14 There is newer evidence suggesting that during the first 24-48 hours of relative rest, screen time should be limited to facilitate faster symptom resolution.17
Impact Metrics
Not every head bump, jolt, or jostle results in a concussion. The recommendation for strict rest is often made from a place of good intention and concern for the long-term sequelae of overworking a “damaged” brain. However, this overabundance of caution is likely contributing to a societal nocebo effect regarding concussion, where every bump, jolt, and jostle is now a cause for serious concern.
What is the impact threshold for sustaining a concussion? The research is not clear-cut on this threshold, but generally speaking, it is likely between 70-160g of linear acceleration (1g = 1 unit of gravity).18,19 For perspective, an open-mouth sneeze is 3g and cervical strain/sprain (ie, whiplash) is 4-5g.20 On paper, based solely on reported symptoms, distinguishing concussion from whiplash is nearly impossible.21 However, the linear acceleration of a concussion is 14-32 times greater than that needed to sustain whiplash. Not every head bump, jolt, or jostle results in a concussion.
Subconcussion, CTE, and the Nocebo Effect
Chronic traumatic encephalopathy is the “elephant in the room” when it comes to the discussion of concussions. One cannot disregard the severity of this condition, which has been associated with structural changes in the brain due to repeated head trauma.22 Every head bump, jolt, or jostle may not result in a concussion, but it must count for something right?
The concerns about CTE are valid; however, it is also important to continue to evaluate the data surrounding subconcussive events and repetitive head impacts (RHI). The average high school or college football player will sustain 586-661 head impacts during a season.23 The average youth or college hockey player will sustain 297-552 head impacts during a season.23 While these numbers sound alarming, conclusions from the research are less than definitive. A 2018 systemic review of subconcussive events found consistent evidence that microstructural changes to the brain were associated with RHI.24 However, it is uncertain if these changes were also associated with previous concussions or drug use, how long these changes last (some changes normalized within months), or how these RHI subjects compared to non-contact control groups.24 Additionally, there was insufficient evidence (90% of investigated outcomes) to link RHI to neurocognitive deficits.24 The authors further concluded, “Concussion is diagnosed by signs and symptoms, and subconcussion is recognized by the absence of a concussion diagnosis. Defining subconcussion by what it is not does not tell us what it is. At best, the term is a fuzzy conceptualization.”24
Researchers investigating the long-term consequences of RHI and its potential to cause CTE primarily advocate for awareness of the potential dangers of head impacts and suggest strategies for keeping athletes safe.24 Media coverage of the issue can be misleading; however, which may also contribute to a possible societal level nocebo effect.25 One study, for example, found that from 2012-2019, 82% of press releases regarding mTBI had a form of spin that perpetuated misinformation about concussions (misleading title, misleading reporting, misleading claims, and inappropriate extrapolation).26
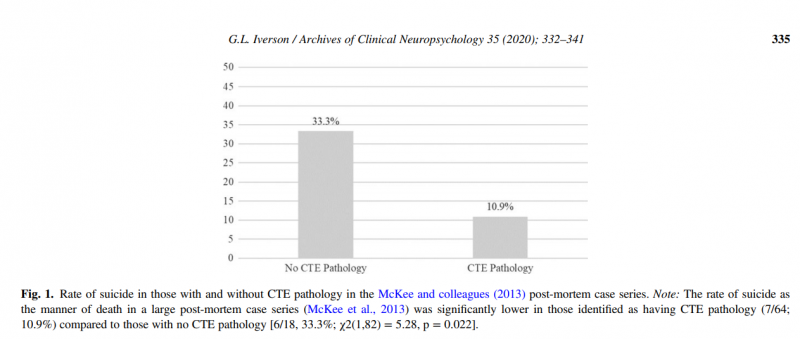
While some studies on CTE pathology report a prevalence of 84-99% in retired male football players, newer evidence in both elite male football and ice hockey players found a much lower prevalence of 48.6%.27 This prevalence was independent of playing position, the number of penalties or fights, or retirement age, and 68.6% of these cases had other neuropathologies present on autopsy.27 CTE pathology has been found in individuals with no known history of contact sport or mTBI.28 CTE pathology is also found in individuals with a history of “substance abuse, temporal lobe epilepsy, amyotrophic lateral sclerosis, multiple systems atrophy, and other neurodegenerative diseases.”29 Additionally, it should be noted that retired NFL players have a decreased risk of suicide compared to the general population (less than half the risk according to some studies).30 Other evidence suggests potential protection against mental health disorders and suicide in professional soccer and American football players.31 In a retrospective cohort study of suicides among active or retired NFL players, there were 15 deaths by suicide recorded from 1920 to 2008, and 11 deaths by suicide recorded from 2009-2015,32 which seems concurrent with increased media coverage of CTE. While this is not direct evidence of a nocebo effect contributing to increased suicidality in athletes, it is important to consider that patient expectations about their illness (and potential for recovery) can affect outcomes. Whether it is increased fears of permanent brain damage in a young person, or the potential hopelessness of a perceived neurocognitive decline by an older athlete, clinicians must consider what information patients may have received before ever entering their office.
Key Takeaways
- A concussion (mTBI) is a functional and temporary injury in which 77-94% of individuals will recover within 4-8 weeks.15 Prescribing strict rest is no longer recommended as it may worsen or prolong symptoms. Symptom-limited activity is recommended as soon as 48-72 hours after injury, and prescribed sub-symptom-threshold aerobic exercise is recommended as soon as 5-7 days after injury.
- Providing patients and parents supportive information can lead to better clinical outcomes by avoiding nocebo effects and dispelling ideas from poor media representation. Not every bump, jolt, or jostle is a concussive injury, and not everyone who played contact sports is destined to a slow neurocognitive decline or death by suicide.
- Chronic traumatic encephalopathy is a complicated pathology and more research is required to fully understand this condition. With study complications of selection bias, small sample sizes, male football player bias, missing control groups, and overlapping comorbidities,33,34 more data is needed before firm conclusions can be made regarding RHI and their relationship to CTE.
- While past concussion(s) are potentially non-modifiable risk factors for CTE and neurodegeneration, modifiable risk factors like physical activity, sleep, and nutrition can improve quality of life and delay cognitive decline.35,36 These are useful messages to convey to patients concerned about their history of head injury; the foundations of health still matter.
As providers, we need to understand that what we and the media say about the risks of RHI, concussions, and CTE have an impact on our patients. Without examining the evidence closely, we may unwittingly further misinformation. Discussing patient fears and long-term concerns, as well as taking the time to provide well-informed answers about mTBI sequelae and expected recovery, can help decrease the probability of a nocebo effect. Head impacts can have serious consequences and should not be ignored; however, it is important to temper concerns based on the available data and to provide practical solutions to mitigate known risks.
Reference:
- Concussion and Mild Traumatic Brain Injury. In DynaMed [database online]. EBSCO Information Services. https://www.dynamed.com/condition/concussion-and-mild-traumatic-brain-injury. Updated March 5, 2021. Accessed July 9, 2021.
- Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53(4):213-225.
- Hiebert JB, Shen Q, Thimmesch AR, Pierce JD. Traumatic brain injury and mitochondrial dysfunction. Am J Med Sci. 2015;350(2):132-138.
- Voormolen DC, Cnossen MC, Spikman J, et al. Rating of pre-injury symptoms over time in patients with mild traumatic brain injury: the good-old-days bias revisited. Brain Inj. 2020;34(8):1001-1009.
- Giza CC, Hovda DA. The Neurometabolic Cascade of Concussion. J Athl Train. 2001;36(3):228-235.
- Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2014;75 Suppl 4:S24-S33.
- Moderate to Severe Traumatic Brain Injury. In DynaMed [database online]. EBSCO Information Services. https://www.dynamed.com/condition/moderate-to-severe-traumatic-brain-injury. Updated June 7, 2021. Accessed July 9, 2021.
- Len TK, Neary JP. Cerebrovascular pathophysiology following mild traumatic brain injury. Clin Physiol Funct Imaging. 2011;31(2):85-93.
- Vagnozzi R, Signoretti S, Cristofori L, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain. 2010;133(11):3232-3242.
- Vagnozzi R, Tavazzi B, Signoretti S, et al. Temporal window of metabolic brain vulnerability to concussions: mitochondrial-related impairment–part I. Neurosurgery. 2007;61(2):379-389.
- Tavazzi B, Vagnozzi R, Signoretti S, et al. Temporal window of metabolic brain vulnerability to concussions: oxidative and nitrosative stresses–part II. Neurosurgery. 2007;61(2):390-396.
- Signoretti S, Lazzarino G, Tavazzi B, Vagnozzi R. The pathophysiology of concussion. PM R. 2011;3(10 Suppl 2):S359-S368.
- McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847.
- Herring S, Kibler WB, Putukian M, et al. Selected issues in sport-related concussion (SRC|mild traumatic brain injury) for the team physician: a consensus statement [published online ahead of print]. Br J Sports Med. 2021;bjsports-2021-104235.
- Kara S, Crosswell H, Forch K, et al. Less Than Half of Patients Recover Within 2 Weeks of Injury After a Sports-Related Mild Traumatic Brain Injury: A 2-Year Prospective Study. Clin J Sport Med. 2020;30(2):96-101.
- Moor HM, Eisenhauer RC, Killian KD, et al. The relationship between adherence behaviors and recovery time in adolescents after a sports-related concussion: an observational study. Int J Sports Phys Ther. 2015;10(2):225-233.
- Macnow T, Curran T, Tolliday C, et al. Effect of Screen Time on Recovery From Concussion: A Randomized Clinical Trial [published online ahead of print]. JAMA Pediatr. 2021;e212782.
- Viano DC, Casson IR, Pellman EJ. Concussion in professional football: biomechanics of the struck player–part 14. Neurosurgery. 2007;61(2):313-328.
- Viano DC, Pellman EJ. Concussion in professional football: biomechanics of the striking player–part 8. Neurosurgery. 2005;56(2):266-280.
- Slade, S. Feel the G’s: The Science of Gravity and G-forces. Mankato, MN: Compass Point Books; 2009.
- Cheever K, Kawata K, Tierney R, Galgon A. Cervical Injury Assessments for Concussion Evaluation: A Review. J Athl Train. 2016;51(12):1037-1044.
- McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709-735.
- Nauman EA, Talvage TM. Subconcussive trauma. Handb Clin Neurol. 2018;158:245-255.
- Mainwaring L, Ferdinand Pennock KM, Mylabathula S, Alavie BZ. Subconcussive head impacts in sport: A systematic review of the evidence. Int J Psychophysiol. 2018;132(Pt A):39-54.
- Polich G, Iaccarino MA, Kaptchuk TJ, et al. Nocebo Effects in Concussion: Is All That Is Told Beneficial?. Am J Phys Med Rehabil. 2020;99(1):71-80.
- Choi AR, Feller ER. Misrepresentation of mild traumatic brain injury research in press releases [published online ahead of print]. PM R. 2021;10.1002/pmrj.12656.
- Schwab N, Wennberg R, Grenier K, et al. Association of Position Played and Career Duration and Chronic Traumatic Encephalopathy at Autopsy in Elite Football and Hockey Players. Neurology. 2021;96(14):e1835-e1843.
- Iverson GL, Luoto TM, Karhunen PJ, Castellani RJ. Mild Chronic Traumatic Encephalopathy Neuropathology in People With No Known Participation in Contact Sports or History of Repetitive Neurotrauma. J Neuropathol Exp Neurol. 2019;78(7):615-625.
- Iverson GL, Gardner AJ, Shultz SR, et al. Chronic traumatic encephalopathy neuropathology might not be inexorably progressive or unique to repetitive neurotrauma. Brain. 2019;142(12):3672-3693.
- Iverson, GL. Retired National Football League Players are Not at Greater Risk for Suicide. Arch Clin Neuropsychol. 2020;35(3):332-341.
- Morales JS, Castillo-García A, Valenzuela PL, et al. Mortality from mental disorders and suicide in male professional American football and soccer players: A meta-analysis [published online ahead of print]. Scand J Med Sci Sports. 2021;10.1111/sms.14038.
- Webner D, Iverson GL. Suicide in professional American football players in the past 95 years. Brain Inj. 2016;30(13-14):1718-1721.
- Schwab N, Hazrati LN. Assessing the Limitations and Biases in the Current Understanding of Chronic Traumatic Encephalopathy. J Alzheimers Dis. 2018;64(4):1067-1076.
- Maroon JC, Winkelman R, Bost J, et al. Chronic traumatic encephalopathy in contact sports: a systematic review of all reported pathological cases. PLoS One. 2015;10(2):e0117338.
- Desai P, Evans D, Dhana K, et al. Longitudinal Association of Total Tau Concentrations and Physical Activity With Cognitive Decline in a Population Sample. JAMA Netw Open. 2021;4(8):e2120398.
- Walton SR, Kerr ZY, Brett BL, et al. Health-promoting behaviours and concussion history are associated with cognitive function, mood-related symptoms and emotional-behavioural dyscontrol in former NFL players: an NFL-LONG Study. Br J Sports Med. 2021;55(12):683-690.

Mark Heisig, ND is a concussion specialist practicing in Scottsdale, AZ. Dr Mark strives to be a leader in integrative concussion recovery by inspiring athletes and motivated individuals with simplicity and innovation to achieve new levels of higher quality performance in sport and life. Dr. Mark lives with his wife and their newborn daughter in AZ, plays ice hockey when he can, runs recreationally, and pets all dogs.