Chris D. Meletis, N.D.
Abstract
Long COVID and chronic fatigue syndrome (CFS) share overlapping pathophysiological mechanisms, with mitochondrial dysfunction emerging as a central driver of persistent fatigue, cognitive impairment, and multisystem dysregulation. Oxaloacetate, a key Krebs cycle intermediate, has gained attention for its ability to enhance mitochondrial biogenesis, restore NAD+/NADH balance, and reduce neuroinflammation. Clinical studies suggest that stabilized oxaloacetate supplementation can significantly reduce both physical and mental fatigue while improving cognition in patients with CFS and long COVID. Beyond energy metabolism, oxaloacetate demonstrates antioxidant and metabolic regulatory effects that may help counteract the cellular stress and impaired bioenergetics underlying post-viral syndromes. This article reviews the current evidence on oxaloacetate as a therapeutic adjunct, positioning it as a promising tool within integrative protocols to improve quality of life and clinical outcomes in patients struggling with long COVID and CFS.
Introduction
Long COVID is a chronic condition in which people suffer from an array of symptoms (Table 1) months or years after the acute phase of COVID. It has become common enough that practitioners frequently have to address this problem in their patients. According to 2024 statistics, an estimated 7% of adults in the United States (approximately 17 million people) were experiencing long COVID during that time.1 This latest data demonstrates that long COVID rates remained relatively consistent over the last year, suggesting that they may persist over time unless new forms of prevention or treatment are unveiled. Other statistics indicate that more than 70% of COVID survivors suffer from ongoing symptoms four months post-infection.2
Table 1: Common Symptoms of Long COVID
| General Symptoms | • Fatigue and post-exertional malaise• Tiredness that interferes with daily life• Fever |
| Respiratory and Heart Symptoms | • Difficulty breathing or shortness of breath• Coughing• Chest pain• Fast-beating or pounding heart (heart palpitations) |
| Neurological Symptoms | • Difficulty thinking or concentrating (sometimes referred to as “brain fog”)• Headaches• Sleep problems• Dizziness upon standing (lightheadedness)• Pins-and-needles feelings• Change in ability to smell or taste• Depression or anxiety |
| Digestive Symptoms | • Diarrhea• Stomach pain• Constipation |
| Other Symptoms | • Joint or muscle pain• Rash• Changes in menstrual cycles |
There are many functional medicine approaches for long COVID that seek to lower spike protein burden and/or may help mitigate symptoms. (Table 2). Many of these approaches have yielded notable clinical success. In this article, we will examine the research from the peer-reviewed literature regarding the addition of supplemental stabilized oxaloacetate to augment existing functional medicine protocols to support patients with long COVID. If oxaloacetate sounds familiar, it is, as it is a regenerated intermediate found in the citric acid/Krebs cycle.
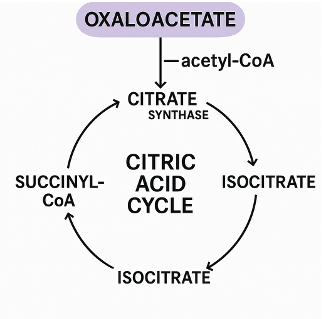
Table 2. A Select Sampling of Functional Medicine Approaches to Long COVID*
| Agent | Mechanism of Action |
| Bromelain | Proteolytic actions3 |
| Nattokinase | Proteolytic actions3 |
| Curcumin | Modulates inflammation, antiviral actions3 |
| N-Acetylcysteine (NAC) | Dissolves spike protein through the destruction of disulfide bonds and prevents binding at ACE2, works together with bromelain4-6 |
| Glutathione | Disrupts spike protein disulfide bonds6 |
| Quercetin | Binds and inhibits spike protein7 |
| Apigenin | Binds and inhibits spike protein7 |
| Nicotine | Disrupts glycosylation on spike protein and blocks possible spike protein-nicotinic cholinergic receptor interaction8,9 |
| Emodin | Blocks the spike protein-ACE2 interaction10 |
| Fisetin | Binds and inhibits spike protein11 |
| Rutin | Binds and inhibits spike protein12 |
| Silymarin | Binds and inhibits spike protein13 |
| Oxaloacetate | Rejuvenates the mitochondria to reduce fatigue |
*The following list is not intended to be exhaustive, rather a sampling of potential clinical considerations to add to your existing protocols, with individual consideration to each patient’s unique biochemistry and physiology.
Mitochondrial Dysfunction’s Role in Long COVID
There are many approaches currently being utilized in functional medicine to support patients presenting signs and symptoms of long COVID, which, due to length, cannot be addressed in this article. Our focus will be more specifically related to mitochondrial dysfunction, which has been implicated in both the duration and the wide variety of long COVID symptoms.2 Mitochondrial dysfunction leads to cellular energy deficits, oxidative stress, immune dysregulation, metabolic disturbances, and endothelial dysfunction, all states that could play a role in long COVID.
Mitochondrial dysfunction is a key mediator in similar post-infectious states caused by other diseases.2 There is potential overlap between the symptoms of long COVID and the well-known negative results of mitochondrial dysfunction.14
Research has identified mitochondrial dysfunction in people suffering from long COVID.15,16,17
Scientists have found impaired mitochondrial respiration and bioenergetics and mitochondria-related gene expression in peripheral blood mononuclear cells (PBMCs) in this group of patients.
Oxaloacetate: An Important Addition to a Long COVID Protocol
Oxaloacetate is a key intermediate of the citric acid cycle and is therefore important to mitochondrial health. Oxaloacetate modulates cellular metabolism, enhances mitochondrial biogenesis, and reduces neuroinflammation in preclinical models.18,19,20 Consequently, scientists have studied its effects in long COVID, with promising results.
In a randomized, controlled clinical trial of oxaloacetate for symptoms of long COVID, 69 participants were randomized into a group who received either 2,000 mg/day of oxaloacetate or a placebo for 42 days.19 At day 21, participants taking oxaloacetate experienced statistically significant improvement in fatigue as measured by the DePaul Symptom Questionnaire Short Form (DSQ-SF). Total symptom burden improved at day 21. Oxaloacetate supplementation also significantly improved cognitive performance—the reduction in long COVID symptoms after oxaloacetate supplementation correlated with cognitive improvement.
In another study, researchers investigated the effects of oxaloacetate treatment for mental and physical fatigue caused by either myalgic encephalomyelitis, chronic fatigue syndrome, or long COVID.21 In a non-randomized, controlled, open-label, dose-escalating “proof-of-concept” study, participants were given oxaloacetate or a placebo for six weeks. ME/CFS groups were given 500 mg BID (n=23), 1000 mg BID (n=29), or 1000 mg TID (n=24); Long-COVID groups were given 500 mg BID (n=22) or 1000 mg BID (n=21).
At six weeks, 76 ME/CFS patients experienced an average reduction in fatigue. As measured by the Chalder Fatigue Questionnaire, both physical and mental fatigue were significantly improved over baseline and placebo. Fatigue reduction dose dependently increased in ME/CFS patients from 21.7% for 500 mg BID to 27.6% for 1000 mg Oxaloacetate BID to 33.3% for 1000 mg TID. Fatigue in long COVID patients significantly declined by up to 46.8% in 6 weeks.
The evidence suggests that oxaloacetate may counteract fatigue through mechanisms that improve mitochondrial health, including the restoration of NAD+/NADH balance, enhancement of mitochondrial biogenesis, antioxidant action, reduction of glycolysis and lactate production, decreased NF-κB activity, and increased glucose uptake via AMPK activation.
Conclusion
Long COVID causes an array of symptoms that interfere with patients’ activities of daily life. Mitochondrial dysfunction is implicated in the pathogenesis of long COVID. The addition of oxaloacetate to your existing long COVID protocol may potentiate outcomes, as it is a known promoter of mitochondrial biogenesis. Taking this approach can lead to enhanced energy, cognitive function, and vitality in patients suffering from this debilitating condition.
Note: Further scientific information on the science of oxaloacetate can be received from one of the co-authors of the REGAIN study and Long Covid Study, Alan Cash acash@benagene.org

Dr. Chris D. Meletis is an educator, international author, and lecturer. His mission is “Changing the World’s Health One Person at a Time.” He believes that when people become educated about their bodies, actual change and wellness begin.
He has written over 200 nationally published articles and over a dozen books to share his passion and amazement of the human body and what is required to maintain health. Dr. Meletis served as Dean of Naturopathic Medicine and Chief Medical Officer for seven years at NCNM, the oldest naturopathic university in North America. The American Association of Naturopathic Physicians awarded him the 2003 Physician of the Year.
References:
1. Burns A. As Recommendations for Isolation End, How Common is Long COVID? KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/as-recommendations-for-isolation-end-how-common-is-long-covid/. Published 2024. Accessed August 15, 2025.
2. Molnar T, Lehoczki A, Fekete M, et al. Mitochondrial dysfunction in long COVID: mechanisms, consequences, and potential therapeutic approaches. Geroscience. 2024;46(5):5267-5286.
3. Hulscher N, Procter BC, Wynn C, McCullough PA. Clinical Approach to Post-acute Sequelae After COVID-19 Infection and Vaccination. Cureus. 2023;15(11):e49204.
4. Akhter J, Quéromès G, Pillai K, et al. The Combination of Bromelain and Acetylcysteine (BromAc) Synergistically Inactivates SARS-CoV-2. Viruses. 2021;13(3).
5. Debnath U, Mitra A, Dewaker V, et al. Conformational perturbation of SARS-CoV-2 spike protein using N-acetyl cysteine: an exploration of probable mechanism of action to combat COVID-19. J Biomol Struct Dyn. 2024;42(10):5042-5052.
6. Murae M, Shimizu Y, Yamamoto Y, et al. The function of SARS-CoV-2 spike protein is impaired by disulfide-bond disruption with mutation at cysteine-488 and by thiol-reactive N-acetyl-cysteine and glutathione. Biochem Biophys Res Commun. 2022;597:30-36.
7. Tuli H. Molecular docking studies of apigenin, kaempferol, and quercetin as potential target against spike receptor protein of SARS CoV. J Exp Biol Agric Sci. 2022;10:144-149.
8. Engin AB, Engin ED, Engin A. Two important controversial risk factors in SARS-CoV-2 infection: Obesity and smoking. Environ Toxicol Pharmacol. 2020;78:103411.
9. Dormoy V, Perotin JM, Gosset P, Maskos U, Polette M, Deslée G. Nicotinic receptors as SARS-CoV-2 spike co-receptors? Med Hypotheses. 2022;158:110741.
10. Ho TY, Wu SL, Chen JC, Li CC, Hsiang CY. Emodin blocks the SARS coronavirus spike protein and angiotensin-converting enzyme 2 interaction. Antiviral Res. 2007;74(2):92-101.
11. Pandey P, Rane JS, Chatterjee A, et al. Targeting SARS-CoV-2 spike protein of COVID-19 with naturally occurring phytochemicals: an in silico study for drug development. J Biomol Struct Dyn. 2021;39(16):6306-6316.
12. Omoboyowa D. SARS-CoV-2 spike glycoprotein as inhibitory target for Insilico screening of natural compounds. Biointerface Res Appl Chem. 2021;11:14974-14985.
13. Speciale A, Muscarà C, Molonia MS, Cimino F, Saija A, Giofrè SV. Silibinin as potential tool against SARS-Cov-2: In silico spike receptor-binding domain and main protease molecular docking analysis, and in vitro endothelial protective effects. Phytother Res. 2021;35(8):4616-4625.
14. Chen TH, Chang CJ, Hung PH. Possible Pathogenesis and Prevention of Long COVID: SARS-CoV-2-Induced Mitochondrial Disorder. Int J Mol Sci. 2023;24(9).
15. Macnaughtan J. Chau KY, et. al Mitochondrial function is impaired in long COVID patients. Ann Med. 2025 Dec;57(1):2528167.
16. Komaroff AL, Dantzer R. Causes of symptoms and symptom persistence in long COVID and myalgic encephalomyelitis/chronic fatigue syndrome. Cell Rep Med. 2025; 19;6(8):102259.
17. Madsen HB, Durhuus JA, et al. Mitochondrial dysfunction in acute and post-acute phases of COVID-19 and risk of non-communicable diseases. NPJ Metab Health Dis.
2024;2(1):36.
18. Vernon SD, Rond C, Bell J, et al. REGAIN: a randomized controlled clinical trial of oxaloacetate for improving the symptoms of long COVID. Front Neurosci. 2025;19:1627462.
19. Wilkins HM, Harris JL, et al.Oxaloacetate activates brain mitochondrial biogenesis, enhances the insulin pathway, reduces inflammation and stimulates neurogenesis. Hum Mol Genet. 2014;23(24):6528–6541.
20. Onuki Y, Nanashima N, et al. Oxaloacetate and Ketone Bodies Synergistically Promote Myoblast Differentiation in L6 Cells. Molecules. 2025;30(10):2101.
21. Cash A, Kaufman DL. Oxaloacetate Treatment For Mental And Physical Fatigue In Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Long-COVID fatigue patients: a non-randomized controlled clinical trial. J Transl Med. 2022;20(1):295.