Emily Chan , ND
Taking into account musical, physical, and emotional factors unique to each patient is instrumental in changing the medical approach from reactive to proactive when dealing with autoimmune diseases.
Act 1: Music
She steps home and notices the achy muscles, the throbbing behind her eyes, and fatigue. She wishes to sleep but can’t because of the many unfinished things to do, a troubling personal life, and a racing mind. As the music plays in the background, she hears the tune, “Happy is the heart that still feels pain. Darkness drains and light will come again. Swing open your chest and let it in. Just let the love begin.”1 In that moment everything lifts, a smile grows on her face, and she feels better.
Act 2: Physical Integration
“Everybody hold hands,” says our gym Yogates coach as he gathers us after class. As we shyly grab our neighbor’s hand he goes on, “I need you to stop. Stop rushing through your daily business. Be aware every time you move, keep your chest lifted, breathe, and use your core to move your body. The way you feel grounded and centered now can be achieved more frequently if you take the time to be mindful of your body.”
Act 3: Emotion
“You guys need to get this together. It is three days before the concert and there is no passion or emotion. Do you know that when Beethoven was writing his Second Symphony, he was struggling with the idea of ending his life because of the frustration as a composer going deaf, and the isolation from the world?” says music director of the San Francisco Symphony Youth Orchestra. He sits on a stool and gently reads us Beethoven’s 1802 Heiligenstadt Testament. “…What a humiliation for me when someone standing next to me heard a flute in the distance and I heard nothing. Such incidents drove me almost to despair; a little more of that and I would have ended my life. It was only my art that held me back. Oh, it seemed to me impossible to leave the world, until I had brought forth all that I felt within me. So I endured this wretched existence…”2
Introduction
Naturopathic practitioners are familiar with and often use nutritional supplements and diet as therapies for autoimmune conditions. However, incorporating mind/body medicine is crucial, especially when a type of disease such as autoimmunity metaphorically can be paralleled to rejecting tissue belonging to self. If social or emotional issues are present, healing in these areas is equally important to physical healing. This article will discuss how the following affect autoimmune disease: (1) music, (2) physical integration, and (3) emotion.
Music
Norman Cousins interviewed the renowned cellist Pablo Casals in 1966 at Casals’ home for his book Anatomy of an Illness, before the musician’s 90th birthday.3 Pablo Casals seemed very frail, needing assistance to get dressed due to rheumatoid arthritis and breathed heavily from emphysema. One would think that his swollen hands and clenched fingers would keep him from playing the music he loved. With physical difficulty, Casals sat himself down at the piano, playing Bach’s Das Wohltemperierte Klavier for his guest Norman Cousins, who was astonished that the supposed painful, sickly and deformed hands “raced across the keyboard with dazzling speed…it was no longer stiff and shrunken but supple and graceful, completely freed of its arthritic coils.”4 Casals’ physical state seemed to change observably once he started playing music.
How Does Music Affect the Body?
By observing this momentary increase in range of motion and alleged decrease in pain, what conclusions can be drawn about music in the life of Pablo Casals? There are many studies that show physiological and neuroanatomical benefits with playing a musical instrument, including an increase in the size of the corpus callosum, which connects the left and right brain.4 However, since many patients may not play musical instruments, studies below were chosen to show beneficial effects with mere listening.
A study in 2008 involving elderly patients suffering from osteoarthritis showed a statistically significant decrease in pain among experimental group participants. One group listened to music 20 minutes per day for 2 weeks while the control group sat in silence for 20 minutes per day, for the same duration. The group that listened to music reported less pain, assessed by the SF-MPQ (short form McGill Pain Questionnaire),5 showing the power of music in relation to pain management.
A 2004 study showed increased opiate receptor expression and decreased IL-6 after listening to music for 20 minutes.6 An increase in opiate receptors is associated with decreased pain and an increased sense of euphoria. Since IL-6 is an inflammatory cytokine, a decrease in IL-6 decreases the inflammatory process associated with autoimmunity. A study at Wilkes University showed a statistically significant increase in immunoglobulin A (IgA) in a group of college students who listened to 30 minutes of music compared to controls.7 Another study published by the Journal of Music Therapy demonstrated decreased cortisol levels in the blood of music listeners.8 If music changes levels of cortisol, IL-6, IgA and opiate receptors, how do these changes affect autoimmune disease?
IgA and Autoimmunity
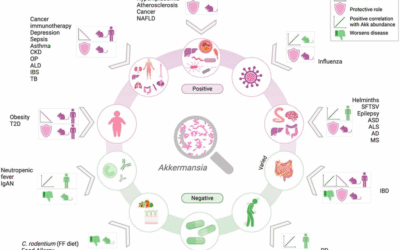
In the January 2010 issue of the Journal of Clinical Immunology, it was shown that IgA decreases the inflammatory response and plays a role in preventing development of autoantibodies.9 The same issue links recurrent respiratory and gastrointestinal infections, allergic disorders, and autoimmune conditions with IgA deficiency.10 Low IgA is associated with increased intestinal permeability. Intestinal permeability is one of the contributing factors to allergy and autoimmunity due to chains of amino acids being leaked into the bloodstream stimulating an immune response.
GALT (gut-associated lymphoid tissue) is one area that IgA is found within the intestinal mucosa.11 It functions in signaling macrophages and other WBCs to scavenge foreign particles. However in patients with “leaky gut syndrome,” IgA is depleted in the process of excessive immunological activity. Contrary to the popular belief that IgA deficiency cannot be corrected, recent studies show that music can increase IgA levels,7 as can bovine colostrum.12
What Role Do Endogenous Opioids Play in Mitigating Autoimmunity?
Ever since Candace Pert, PhD discovered the opiate receptor in 1972, there has been more attention on the psycho-neuro- immunological significance of opiates. Opiates, including morphine, have been used as a prescription drug, recreational drug, relaxant, painkiller, and as a way to induce euphoria. However, it was thought soon after the discovery of the opiate receptor that if these drugs bound to it, there must be a reason for the existence of the opiate receptor, namely that the body must produce a substance similar that binds to this receptor. In 1975 the endogenous opiate enkephalin was discovered. The researchers later named enkephalin “endorphin,” meaning endogenous morphine.13
A study published in the Journal of Dermatology in 2004 investigated patients with polymyositis/dermatomyositis, both autoimmune diseases. The study showed lower levels of beta-endorphins in the plasma of patients with polymyositis/dermatomyositis compared to controls.14 Another study done in Milan, Italy showed a correlation between low hypothalamic concentration of beta-endorphin with lupus and autoimmune thyroiditis.15
Low endorphin levels seem to be associated with autoimmunity, but how? The School of Physiology and Pharmacology at the University of New South Wales in Sydney, Australia, used rheumatoid arthritis patients as subjects and found 4 mechanisms by which opioids are anti-inflammatory and immunomodulating. Opioids (i) reduced adhesion molecule expression; (ii) inhibited cell trafficking; (iii) reduced TNF alpha release and expression; and (iv) altered mRNA expression and protein levels of substance P and CGRP (calcitonin gene related peptide) in synovial tissue.16
Research has shown that listening to music, exercise, stress reduction, and a positive attitude can increase endogenous opiates in the body, supporting an anti-inflammatory effect.
Physical Integration
“Perfect balance of Body and Mind is that quality in civilized man… which furnishes him with all the physical and mental powers that are indispensable for attaining the goal of Humankind- Health and Happiness.” Joseph Pilates17
Joseph Pilates was born in Germany in 1883. Being a sickly child suffering from asthma, rickets, and rheumatic fever, he set forth to develop methods to strengthen his body and health. Joseph Pilates was in England when the First World War broke out where British authorities assigned him to a camp on the Isle of Man. He worked with injured patients by attaching springs to hospital beds to support their limbs while he worked with them using Contrology, later named Pilates. Doctors noticed that patients who worked with Pilates had a decreased recovery time from their injuries. His patients and interns were in much better physical shape, allowing them to maintain their health through the influenza epidemic of 1918. After the war, Joseph moved back to Germany and trained the police and army. However he developed social and political differences with the German regime and moved to the United States in 1925. There he founded a studio in New York City and trained famous dancers such as Martha Graham and ballet choreographer George Balanchine.18
In his physical core muscle conditioning exercises, Joseph Pilates integrates breathing, posture, and mind/body.
He says that in this modern age, we must put more thought into developing physical fitness, especially “the uniform development of our bodies as a whole.” Contrology allows the body to be “freed from nervous tension and over-fatigue.” Pilates teaches that “the body is the ideal shelter provided by nature for housing a well balanced mind that is always fully capable of successfully meeting all the complex problems of modern living.”17
Mind/Body medicine is becoming a burgeoning field of medicine. A 2010 study showed that those who have practiced yoga for long periods of time have decreased inflammatory markers such as CRP and IL-6.19 Advanced conditioned people in mind/body medicine may have increased buffers against stressors contributing to lower levels of inflammatory markers. Another study performed in India showed that yoga statistically decreased blood levels of TBARS (thiobarbituric acid reactive substance), an indicator of oxidative stress that contributes to a variety of chronic degenerative diseases including autoimmunity.20
David Eisenberg, currently director of Harvard’s Division for Research and Education in Complementary and Integrative Medical Therapies, discusses his reflection on observing the Chinese perform Tai Chi:
They are trying to figure out where their center is, what is a balanced form, where right and left are. You might ask, what does that have to do with medicine? In the Chinese culture that defines health. If you can figure out where your center is and how to concentrate your mind, you’re healthy and once you lose that, you get sick. In order to maintain health, you have to have physical movement, but also meditative balance. And you have to control not only your physical body, but also your will, and intention and your thoughts.21
Pilates, yoga and Tai Chi all focus on using the mind/body connection, integrating the body as a whole. This integration has profound effects on the biochemical molecules known to influence autoimmunity.
Emotions
Ludwig van Beethoven expressed intense emotion in his Heiligenstadt Testament. The psychological state Beethoven was in at the time could have taken one of two turns, one detrimental to his existence, namely, ending his life. However, he worked through his personal crisis in the time period of his second symphony. Beethoven said, “For a while now, I have been gaining more than ever in physical strength and mental strength. Every day I come closer to my goal, which I can sense but don’t know how to describe.”22 His next symphony, the third, was about “a contest between emotion and reason, in a search of what it means to be human.”23 He reframed his view of life, choosing not to end it but to express his emotions through composing. Even though his physical condition that caused him much agony did not change, he channeled his frustrations in a healthier way. What if Beethoven hadn’t experienced such challenging emotions? There would not have been as much substance, passion, and process that enriched his life inspiring his 9 symphonies that have blessed many listeners.
How Does Emotion Affect Natural Killer Cells?
A surprising study done by Margaret Kemeny, assistant professor of the Department of Psychiatry and Behavioral Sciences at the University of California, Los Angeles studied the effects of shortterm emotions on the immune system using actors as subjects. When the actors got into a state of sadness for 20 minutes, there was a measured increase in the number of natural killer (NK) cells.21
NK cells have a dual potential for acting as either protective or pathogenic depending on the disease, making interpretation of data from studies difficult. In general, NK cells play a role in protecting against viral infections and cancer. Levels of NK cells in relation to autoimmune disease are varied. Some studies show that excessive activation of NK cells contribute to rheumatoid arthritis or atopic conditions,24 but deficiency in NK cells are associated with multiple sclerosis.25 Furthermore, it was found that NK cells are necessary for maintaining intestinal health.11 A healthy intestinal tract decreases autoimmunity by decreasing intestinal permeability.
The second part of the study showed that when actors elicited happiness for 20 minutes, NK cells increased.21 Therefore, whether actors induced happy or sad emotional states, NK cells increased. Experiencing transient emotions stimulated the immune system.
This raises the question of immunological consequences of people on antidepressants who report feeling a flattened affect, or those who suppress their emotions in response to trauma. Being able to experience sad or happy emotions increases NK cells. The complicating factor in interpreting this data involves mixed studies; some show that increased levels of NK cells improve outcomes of certain autoimmune diseases while others show lower levels of NK cells as protective of autoimmune disease.24,25 Perhaps the key is a proper balance of the number of cells and appropriate interaction with other immune signaling cells. The beneficial effects of being able to experience transient emotions must be separated from states of depression or chronic stress. Practitioners should consider guiding their patients, or directing patients to those who would guide them, to channel their emotional experiences into positive personal growth in a way that is healthful physically and psychologically.
How Does Stress Affect Autoimmunity?
Common observation and patient anecdotes point to increased stress either worsening or setting off autoimmune diseases. Cortisol is increased during times of stress. However, traditional treatment for many autoimmune diseases involves the use of glucocorticoids, such as prednisone. So why do the two seem contradictory? Shouldn’t stress then decrease autoimmunity?
There is a bell-shaped curve comparing stress and immune function. During the first hour of stress the immune system functions higher than baseline. Immune cells are released into circulation and B and T cells are signaled to proliferate. The stressors can be psychological, physical or infectious. Glucocorticoids and sympathetic stimulation are thought to be responsible for this immune activation during acute stress.26
After approximately one hour, sustained glucocorticoid and sympathetic activation start to cause immune suppression. Sustained glucocorticoid release results in higher levels of cortisol in the body.26 There is a dose-dependent effect of cortisol on the immune system. Steroids that are administered in the treatment of autoimmune diseases are of large enough dosage to cause immune suppression.
Under normal circumstances, the bell-shaped curve associated with the stimulation and return to baseline of the immune system in response to stress is protective. Slight increase in immune function with a physical stressor such as exposure to a microbe is beneficial to ward off infection. After a certain period the immune system returns to baseline.
If the immune system is constantly activated such as in chronic stress, it has been shown in experiments that the compensatory immune suppression following immune activation is blocked.26 One explanation for this phenomenon is lack of refractory period where the system lacks time to return to baseline. This results in the immune system becoming more and more active, until it reaches a state of pathological over activity such as autoimmunity.
Having a range of emotions is important in experiencing the full spectrum that accompanies living. The expectation of perpetual happiness is unrealistic. Rather, having self-awareness that allows one to work through feelings, instead of repressing them, gives room for allowing this process to occur with an underlying sense of peace, joy and hopefulness. Studies show that optimism is associated with lower health risks and lower obstacles to goal pursuit.27 Rather than mentally focusing on the past or future, or attempting to fill a void with distraction such as overworking, overeating, excessive media consumption, or avoidance, perhaps true optimism is living in the present.
Closing Remarks
Through my years of coming in contact with patients, I could not help but notice that patients who have social or emotional difficulties in life seem to experience more obstacles to cure. They get somewhat better, but may take longer to heal, or not reach the level of healing that someone with a similar condition without psychological or social difficulties would.
So I began to ask myself the question, “How exactly does our surrounding environment influence our physiology?” There have been studies on the physiological effects of cortisol, epinephrine, oxytocin, serotonin, etc., but I wanted to go beyond the biochemical pathways and try to make sense of how the sciences and humanities intersect through an anthropological perspective. There is so much more to be discovered in this field. One purpose of this article is to increase awareness towards modulating social factors in patients with autoimmune disease.
Since our bodies are a whole, and naturopathic principles stress “holism,” can we extend this concept beyond the body? Everything is interconnected. Everything affects something or someone. Since we exist in the world, can we exist without our physical, emotional, spiritual, and social environment having profound effects on our physiology?
 Emily Chan, ND graduated Summa Cum Laude from California State University Hayward, with a BS in biology and a minor in music. While a doctorate student at Bastyr University she interned at the Functional Medicine Research Center and ER at Evergreen Hospital. Dr. Chan’s interest in worldwide humanitarian efforts led her to Beijing, China where she worked with disabled children. Through her efforts to further education in others, Dr. Chan currently holds numerous speaking engagements throughout Massachusetts and Washington State. Dr. Chan performs with local orchestras and appears regularly on a local access television program titled “A Healer in Every Home.” She currently practices in Cambridge, Massachusetts.
Emily Chan, ND graduated Summa Cum Laude from California State University Hayward, with a BS in biology and a minor in music. While a doctorate student at Bastyr University she interned at the Functional Medicine Research Center and ER at Evergreen Hospital. Dr. Chan’s interest in worldwide humanitarian efforts led her to Beijing, China where she worked with disabled children. Through her efforts to further education in others, Dr. Chan currently holds numerous speaking engagements throughout Massachusetts and Washington State. Dr. Chan performs with local orchestras and appears regularly on a local access television program titled “A Healer in Every Home.” She currently practices in Cambridge, Massachusetts.
References
1. Michaelson I. Everybody [CD]. Cabin 24 Records; 2009.
2. Heiligenstadt Testament. Encyclopædia Britannica Web site. http://www.britannica.com/EBchecked/topic/259632/Heiligenstadt-Testament. Accessed February 9, 2010.
3. Cousins N. Anatomy of an Illness as Perceived by the Patient: Reflections on Healing and Regeneration. New York, NY: WW Norton & Co Inc; 1979.
4. Campbell D. The Mozart Effect: Tapping the Power of Music to Heal the Body, Strengthen the Mind and Unlock the Creative Spirit. New York, NY: William Morrow & Co; 1997.
5. McCaffrey R. Music listening: its effects in creating a healing environment. J Psychosoc Nurs Ment Health Serv.
2008;46(10):39-44.
6. Stefano GB, Zhu W, Cadet P, Salamon E, Mantione KJ. Music alters constitutively expressed opiate and cytokine processes in listeners. Med Sci Monit. 2004;10(6):MS18-27.
7. Charnetski CJ, Brennan FX Jr, Harrison JF. Effect of music and auditory stimuli on secretory immunoglobulin A (IgA). Percept Mot Skills. 1998;87(3 Pt 2):1163-1170.
8. Bartlett D, Kaufman D, Smeltekop R. The effects of music listening and perceived sensory experiences on the
immune system as measured by interleukin-1 and cortisol. J Music Ther. 1993;30(4):194-209.
9. Monteiro RC. Role of IgA and IgA fc receptors in inflammation. J Clin Immunol. 2010 Jan;30(1):1-9.
10. Yel L. Selective IgA deficiency. J Clin Immunol. 2010;Jan;30(1):10-6
11. Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol.
2008;153(suppl 1):3-6.
12. Brinkworth GD, Buckley JD. Concentrated bovine colostrums protein supplementation reduces the incidence of selfreported symptoms of upper respiratory tract infection in adult males. Eur J Nutr. 2003;42(4):228-232.
13. Pert CB. Molecules of Emotion: Why You Feel the Way You Feel. New York, NY: Scribner Book Co; 1997.
14. Liu J, Li J, Zhai N, Geng L, Song F. Detection of the levels of neuropeptides, ACTH and cortisol in the blood of patients with polymyositis/dermatomyositis and their significance. J Dermatol. 2004; 31(5):392-397.
15. Sacerdote P, Lechner O, Sidman C, Wick G, Panerai AE. Hypothalamic beta-endorphin concentrations are
decreased in animal[s] models of autoimmune disease. J Neuroimmunol. 1999;97(1-2):129-133.
16. Walker JS. Anti-inflammatory effects of opioids. Adv Exp Med Biol. 2003;521:148-160.
17. Pilates J, Miller WJ. Return to Life. Boston, MA: Christopher Publishing House; 1945.
18. Siler B. The Pilates Body: The Ultimate At-Home Guide to Strengthening, Lengthening, and Toning Your Body—Without Machines. New York, NY: Broadway Books; 2000.
19. Kiecolt-Glaser JK, Christian L, Preston H, et al. Stress, inflammation, and yoga practice. Psychosom Med.
2010;72(2):113-121.
20. Yadav RK, Ray RB, Vempati R, Bijlani RL. Effect of a comprehensive yoga-based lifestyle modification program on lipid peroxidation. Indian J Physiol Pharmacol. 2005;49(3):358-362.
21. Moyers B. Healing and the Mind. New York, NY: Bantam Doubleday Dell Publishing Group; 1993.
22. Steinberg M. The Symphony: A Listener’s Guide. New York, NY: Oxford University Press; 1995.
23. Thomas MT. Keeping Score: Revolutions in Music – Beethoven’s Eroica [DVD]. San Francisco Symphony; 2006.
24. Miellot-Gafsou A, Biton J, Bourgeois E, Herbelin A, Boissier MC, Bessis N. Early activation of invariant natural killer T cells in a rheumatoid arthritis model and application to disease treatment. Immunology. 2010;[Epub ahead of print].
25. Yamamura T. Therapeutic strategy for multiple sclerosis targeting NK and NKT cells [in Japanese]. Rinsho Shinkeigaku. 2001;41(12):1162-1164.
26. Sapolsky RM. Why Zebras Don’t Get Ulcers, 2nd Edition: An Updated Guide to Stress, Stress Related Diseases, and Coping. New York, NY: WH Freeman; 1998.
27. Zhang Y, Fishbach A. Counteracting obstacles with optimistic predictions. J Exp Psychol Gen. 2010;139(1):16-31.