Naturopathic Management of Arthralgias Associated with Aromatase Inhibitor Therapy
Daniel Lander, ND, FABNO and Katherine Neubauer, ND
Aromatase inhibitors (AIs) have been shown to be more effective than tamoxifen alone in preventing breast cancer recurrence in postmenopausal women.1 However patients often discontinue taking AIs because of musculoskeletal side effects.2,3 Tamoxifen acts as a selective estrogen receptor modulator, while AIs decrease circulating estrogen levels in postmenopausal women by blocking the conversion of adrenal androgens into estrogen. Compared with tamoxifen, AIs are associated with fewer thromboembolic events and endometrial abnormalities. However, AIs have been associated with decreased bone mineral density and fractures, as well as significant joint pain and stiffness.
AI-associated pain is actually more common than described in initial clinical trials.3 In fact, one study reported joint and/or bone pain in 61% of patients taking an AI and found that 20% of patients ultimately discontinued their AI therapy as a result.2 Risk factors for severe articular side effects include obesity, hormone receptor positivity, and prior chemotherapy.4 The incidence of arthralgias is equivalent among the 3 commonly prescribed AIs, however switching from one to another often reduces pain. In one trial, 71% of women with dose-limiting arthralgia from anastrozole were able to tolerate letrozole for at least 6 months.5 Interestingly, there is evidence that AI-induced arthralgias may not be all bad as their presence has been associated with increased effectiveness of treatment and a more favorable prognosis.6
Treating the Cause
Several mechanisms have been proposed to explain aromatase inhibitor-induced arthralgias.
Estrogen Deprivation
Estrogen has a well-known role in joint pain. Menopausal arthritis was first described in 1925 as the rapid development of hand and knee osteoarthritis coinciding with the cessation of menses.7 Since then studies have shown that hormone replacement therapy reduces the incidence of osteoarthritis and increases joint cartilage volume.8,9 Estrogen blockade may also directly increase pain perception and decrease pain tolerance.
Estrogen may also interact with melatonin, and exposure to full spectrum light in the mornings has been proposed as a treatment for AI-induced arthralgias.10 The hypothesis is that decreased estrogen inhibits daylight suppression of melatonin. This daylight benefit has also been observed in patients with rheumatoid arthritis and may ameliorate morning stiffness.
Inflammation
The role of inflammation in AI-induced arthralgias is controversial. One small clinical study showed radiographic evidence of tenosynovitis in 12 women receiving letrozole or exemestane.11 A larger study found evidence of carpal tunnel syndrome on electromyogram, but no rise in multiple serum inflammatory markers.12
Some patients may benefit from natural anti-inflammatories such as fish oil, but clinically the effects are inconsistent. Colleagues Dr. Jacob Schor and Dr. Davis Lamson have observed that botanical anti-inflammatories are rarely effective for AI-induced arthralgias.3,13
Changes in Joint Structural Integrity
Since AIs increase the incidence of osteopenia and fracture, therapies targeting connective tissue integrity are well indicated to treat the whole person. Furthermore, therapies targeted at increasing bone density may improve AI-induced arthralgias. A recent clinical trial studied the supplementation of 50,000 IU of vitamin D3 weekly for 12 weeks in 50 breast cancer patients taking letrozole. Only 20% of the women had baseline serum 25-hydroxyvitamin D levels >40 ng/mL, which is considered necessary for optimal musculoskeletal functioning.14 Although it did not reach statistical significance, clinical relief of joint pain was seen in 23% of patients. Patients whose vitamin D levels rose above 66 ng/mL were more likely to report complete resolution of joint pain.14 This continues to be an area of interest among researchers and there are currently 3 ongoing trials studying the effect of vitamin D on AI-related arthralgias.15-17
A retrospective review of 316 women receiving AIs found that arthralgias were positively correlated with baseline osteopenia. This study also showed that the use of calcium with a bisphosphonate decreased the prevalence of reported joint pain.18
Exercise is another well-known intervention used to maintain bone density and has been described in anecdotal reports and small prospective studies to also benefit AI-induced arthalgias.19 A cross-sectional survey showed that 46% of women with AI-related joint pain used some form of exercise to relieve their symptoms.3
Another study reported that glucosamine was helpful in relieving pain in 15% of patients interviewed regarding their arthralgia after starting AI therapy.2
Autoimmunity
Case reports have associated AI therapy with the onset of autoimmune disorders such as rheumatoid arthritis and Sjögren’s syndrome.20,21 However, this has not been confirmed in larger studies.22 Nevertheless, immune balancing may be an effective treatment approach for AI-induced arthralgias. A recent pilot study showed an improvement in pain, stiffness, and functioning in women with AI-related joint symptoms treated with a subcutaneous injection of a specific thymus peptide component, Thymosin alpha-1. This symptomatic improvement was also correlated with a balancing of cell-mediated (TH1) and humoral (TH2) immunity in these patients.23
Balancing the Vis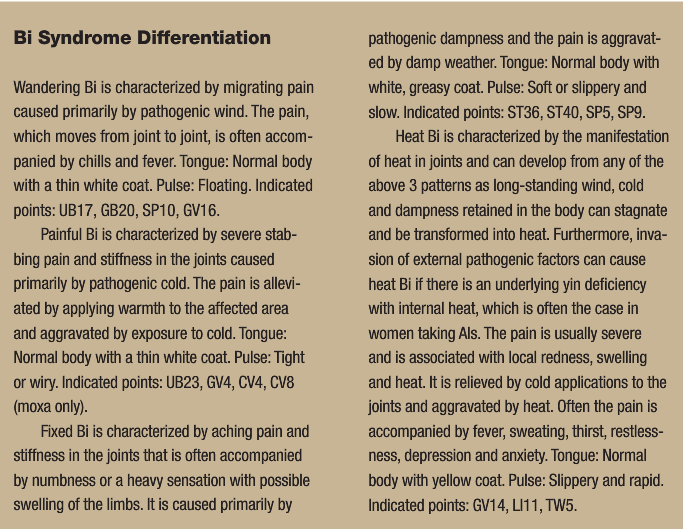
Naturopathic medicine may offer additional support for treating these arthralgias though treatment modalities that do not rely on the biomedical etiology of the condition to determine appropriate treatment, but instead focus on the patient’s individual expression of the imbalance within the system.
Traditional Chinese Medicine
In Traditional Chinese Medicine (TCM), arthralgias are described as “Bi syndromes.” Bi, which means stagnancy in Chinese, manifests as pain, stiffness, numbness, and/or swelling of joints, tendons, vessels or muscles. It is the result of an invasion of the meridians and collaterals by external pathogenic factors (wind, cold, and dampness) and the subsequent impairment of qi and blood circulation. When qi and blood are not able to flow naturally, they stagnate, causing pain, heat, and other symptoms of illness. Acupuncture and herbal therapy help to open the blockages, balance the energy, and harmonize qi and blood.
Scientifically proving the validity of these ancient concepts is challenging, but increasing numbers of well-designed clinical trials support the use of acupuncture in osteoarthritis.24-26 A recent randomized, blinded, sham-controlled trial examined the use of acupuncture for arthralgias specifically in women with early stage breast cancer taking an AI. Patients received acupuncture treatments twice weekly for 6 weeks. Those who received the true acupuncture had a significant improvement in joint pain and stiffness and a decreased analgesic usage that was not seen in the sham acupuncture group.27 Another small pilot study using electro-acupuncture found similar results with regards to joint pain and stiffness and also saw a significant improvement in associated fatigue and anxiety.28
In addition to acupuncture, TCM frequently employs herbs to treat joint pain, usually in the form of traditional patent formulae. A study looking at the incidence of AI-associated arthralgias described 2 cases where Keishi-ka-nijutsuto relieved joint pain and ultimately allowed these patients to complete their AI therapy.29
Homeopathy
Homeopathy continues to be a challenging therapy to study within the constraints of randomized, controlled trials. An observational study was able to show a trend towards improvement in joint pain and stiffness related to estrogen withdrawal with the use of homeopathy, but the numbers did not reach statistical significance and this remains an area in need of further study.30 Clinically, the authors have found homeopathy to be an effective method for treating aromatase-induced arthralgias when the remedy is chosen constitutionally based on the totality of symptoms. Several remedies have been used successfully, but we have found Sepia in particular is often indicated in these patients.
Conclusion
While AIs can be beneficial for prevention of breast cancer recurrence, the musculoskeletal side effects are often dose limiting. Naturopathic therapies can improve tolerance of AI therapy while also strengthening overall health.
Acknowledgements
The authors would like to thank Dr. Davis Lamson and Dr. Jacob Schor for gathering the preliminary research for this article in their OncANP research review on the same topic.13
 Daniel Lander, ND, FABNO received his premedical training and earned a Bachelor of Science degree with honors in nutritional and nutraceutical sciences from the University of Guelph in Ontario, Canada. Dr. Lander graduated from CCNM in 2006 and completed a two-year hospital-based residency at Cancer Treatment Centers of America in Tulsa, Okla., where he continues to practice as a staff naturopathic physician. He is board-certified in naturopathic oncology as a fellow of the American Board of Naturopathic Oncology. Dr. Lander currently serves on the Board of Directors of the Oncology Academy of Naturopathic Physicians and is the president of the Oklahoma Association of Naturopathic Physicians.
Daniel Lander, ND, FABNO received his premedical training and earned a Bachelor of Science degree with honors in nutritional and nutraceutical sciences from the University of Guelph in Ontario, Canada. Dr. Lander graduated from CCNM in 2006 and completed a two-year hospital-based residency at Cancer Treatment Centers of America in Tulsa, Okla., where he continues to practice as a staff naturopathic physician. He is board-certified in naturopathic oncology as a fellow of the American Board of Naturopathic Oncology. Dr. Lander currently serves on the Board of Directors of the Oncology Academy of Naturopathic Physicians and is the president of the Oklahoma Association of Naturopathic Physicians.
 Katherine Neubauer, N.D. received her doctorate at SCNM. She practices in Tulsa, Okla., where she is completing a residency in naturopathic oncology. Contact: [email protected].
Katherine Neubauer, N.D. received her doctorate at SCNM. She practices in Tulsa, Okla., where she is completing a residency in naturopathic oncology. Contact: [email protected].
References
- Baum M, Buzdar AU, Cuzick J, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet. 2002;359(9324):2131-2139.
- Presant CA, Bosserman L, Young T, et al. Aromatase inhibitor-associated arthralgia and/or bone pain: frequency and characterization in non-clinical trial patients. Clin Breast Cancer. 2007;7(10):775-778.
- Crew KD, Greenlee H, Capodice J, et al. Prevalence of joint symptoms in postmenopausal women taking aromatase inhibitors for early-stage breast cancer. J Clin Oncol. 2007;25(25):3877-3883.
- Sestak I, Cuzick J, Sapunar F, et al. Risk factors for joint symptoms in patients enrolled in the ATAC trial: a retrospective, exploratory analysis. Lancet Oncol. 2008;9(9):866-872.
- Briot K, Tubiana-Hulin M, Bastit L, Kloos I, Roux C. Effect of a switch of aromatase inhibitors on musculoskeletal symptoms in postmenopausal women with hormone-receptor-positive breast cancer: the ATOLL (articular tolerance of letrozole) study. Breast Cancer Res Treat. 2010;120(1):127-134.
- Cuzick J, Sestak I, Cella D, Fallowfield L, ATAC Trialists’ Group. Treatment-emergent endocrine symptoms and the risk of breast cancer recurrence: a retrospective analysis of the ATAC trial. Lancet Oncol. 2008;9(12):1143-1148.
- Cecil RL, Archer BH. Arthritis of the menopause. J Am Med Assoc. 1925;84(2):75-79.
- Hart DJ, Doyle DV, Spector TD. Incidence and risk factors for radiographic knee osteoarthritis in middle-aged women: the Chigford Study. Arthritis Rheum. 1999;42(1):17-24.
- Wluka AE, Davis SR, Bailey M, Stuckey SL, Cicuttini FM. Users of oestrogen replacement therapy have more knee cartilage than non-users. Ann Rheum Dis. 2001;60(4):332-336.
- Burk R. Aromatase inhibitor-induced joint pain: melatonin’s role. Med Hypotheses. 2008;71(6):862-867.
- Morales L, Pans S, Paridaens R, et al. Debilitating musculoskeletal pain and stiffness with letrozole and exemestane: associated tenosynovial changes on magnetic resonance imaging. Breast Cancer Res Treat. 2007;104(1):87-91.
- Dizdar O, Ozçakar L, Malas FU, et al. Sonographic and electrodiagnostic evaluations in patients with aromatase inhibitor-related arthralgia. J Clin Oncol. 2009;27(30):4955-4960.
- Lamson D, Schor D. Oncology Association of Naturopathic Physicians Research Review. Electronic Publication. October 2009.
- Khan QJ, Reddy PS, Kimler BF, et al. Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat. 2010;119(1):111-118.
- US National Institutes of Health. High dose vit D musculoskeletal symptoms & bone density in anastrozole-treated breast cancer with marginal vit D status. ClinicalTrials.gov Web site. http://clinicaltrials.gov/show/NCT00263185. Published December 6, 2005. Updated February 18, 2009. Accessed March 9, 2010.
- US National Institutes of Health. Vitamin D deficiency and muscle pain and/or joint pain in postmenopausal women receiving letrozole for stage I, stage II, or stage III breast cancer. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct/show/NCT00416715. Published December 27, 2006. Updated February 25, 2010. Accessed March 9, 2010.
- US National Institutes of Health. Vitamin D3 for Aromatase Inhibitor Induced Arthralgias. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct/show/NCT00867217. Published March 20, 2009. Updated December 7, 2009. Accessed March 9, 2010.
- Muslimani AA, Spiro TP, Chaudhry AA, Taylor HC, Jaiyesimi I, Daw HA. Aromatase inhibitor-related musculoskeletal symptoms: is preventing osteoporosis the key to eliminating these symptoms? Clin Breast Cancer. 2009;9(1):34-38.
- Henry NL, Giles JT, Stearnes V. Aromatase inhibitor-associated musculoskeletal symptoms: etiology and strategies for management. Oncology. 2008;22(12):1-4.
- Laroche M, Borg S, Lassoued S, De Lafontan B, Roché H. Joint pain with aromatase inhibitors: abnormal frequency of Sjögren’s syndrome. J Rheumatol. 2007;34(11):2259-2263.
- Morel B, Marotte H, Miossec P. Will steroidal aromatase inhibitors induce rheumatoid arthritis? Ann Rheum Dis. 2007;66(4):557-558.
- Henry NL, Giles JT, Ang D, et al. Prospective characterization of musculoskeletal symptoms in early stage breast cancer patients treated with aromatase inhibitors. Breast Cancer Res Treat. 2008;111(2):365-372.
- Zhang Q, Tang D, Zhao H. Immunological therapies can relieve aromatase inhibitor-related joint symptoms in breast cancer survivors. Am J Clin Oncol. 2010;20(10):1-4.
- Vas J, Méndez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ. 2004;329(7476):1216.
- Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomized trial. Lancet. 2005;366(9480):136-143.
- Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141(12):901-910.
- Crew KD, Capodice JL, Greenlee H, et al. Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol. 2010;28(7):1154-1160.
- Mao JJ, Bruner DW, Stricker C, et al. Feasibility trial of electroacupuncture for aromatase inhibitor–related arthralgia in breast cancer survivors. Integr Cancer Ther. 2009;8(2):123-129.
- Ohsako T, Inoue K, Nagamoto N, et al. Joint symptoms: a practical problem of anastrozole. Breast Cancer. 2006;13(3):284-288.
- Thompson EA, Reilly D. The homeopathic approach to the treatment of symptoms of oestrogen withdrawal in breast cancer patients. a prospective observational study. Homeopathy. 2003;92(3):131-134.









