Orthopedics
Noel Peterson, ND, DAAPM
Samuel G. Oltman, ND
In Part 1 of our article, “Naturopathic Regenerative Orthopedics,” we explained the ever-increasing need for effective osteoarthritis treatments, we reviewed the current standard of care in conventional orthopedics, and we outlined a summary of naturopathic treatment modalities. Lastly, dextrose prolotherapy was introduced as the first Regenerative Injection Therapy (RIT) that can reverse the degeneration of osteoarthritis (OA) and effectively treat OA-associated pain.
Dextrose Prolotherapy
Dextrose prolotherapy, in summary, has the ability to regenerate cartilage in OA, repair tears in tendons, and strengthen/heal torn or lax ligaments – all of which reduce joint pain. It achieves these actions through attracting the body’s innate healing response to tissues that are hypovascular by nature and therefore more susceptible to suboptimal healing from chronic mechanical insults. Dextrose prolotherapy is a low-cost therapy that can easily be done in-office with minimal discomfort. One major misconception about this treatment is that is works by “scarring” the target tissue. This is not correct. The action, rather, is one of reorganization and regeneration through the work of macrophages, chondrocytes, and osteoblasts. It restores normal tissue histology and function, thereby reducing pain in a multitude of different musculoskeletal conditions.
We will now discuss the next two RITs on the treatment hierarchy: Platelet-Rich Plasma and Adult Autologous Adipose-Derived Stem Cells. Both are therapies that biochemically harness and concentrate the Vis Medicatrix Naturae into an elegant medicinal product that can be directed into nearly any joint that is suffering degeneration and/or connective tissue damage.
Platelet-Rich Plasma
Platelet-Rich Plasma (PRP) injection prolotherapy utilizes the growth factors in one’s own blood as the active ingredient via a method of extraction and concentration. Over 4100 PubMed articles have been published on PRP. The interest in PRP comes from the fact that platelets are packed with alpha granules, dense granules, and lysosomes. These are the blood’s storehouses for over 400 different cytokines and signaling molecules that are responsible for the repair and regeneration of tissues directly through mesenchymal stem cell proliferation and chondrocyte proliferation.1 Exposure of tissue to PRP growth factors has also been shown to be either inflammatory or anti-inflammatory, depending on the method of concentration/processing and how many white blood cells (WBCs) are present in the final injection solution.2
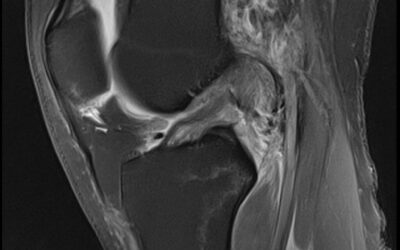
Especially relevant to knee osteoarthritis (KOA), PRP increases the expression of collagen-building proteins while reducing metalloproteinase-1 (MMP-1) expression, a hallmark of inflammatory and degenerative arthropathies.3 There have been over 150 PubMed studies published on the effect of PRP on KOA. In head-to-head clinical trials, PRP has been shown to be superior to corticosteroids, hyaluronate, non-steroidal anti-inflammatory drugs (NSAIDs), and placebo in relieving the pain and disability of KOA.4,5 Campbell et al (2015) found that PRP was especially effective in the early stages of KOA degeneration.6 In a randomized, placebo-controlled trial conducted by Smith et al (2016), PRP injections caused a decrease in WOMAC scores of 78%, as compared to 7% in the placebo group.7 Similar findings have been found repeatedly in subsequent studies, mostly for the knee but also for hip OA.8 No other treatment has matched the benefit of PRP in KOA.
In our clinic, we have observed that most chronic low back pain (CLBP) patients have MRI evidence of multifidi fatty atrophy. This fatty “marbling” of the muscles closest to the posterior vertebral body is both an effect and a cause of chronic low back pain. Hussein et al (2016) used MRI confirmation to show regeneration of the atrophied muscles after 3 weekly ultrasound-guided PRP injections (alone) into chronic CLBP patients, and they documented over 70% improvement in pain in patients suffering from CLBP.9
There have been studies done on fatty atrophy in rotator cuff muscle tears that show similar benefits as listed above, in terms of reduction of adipocytes and increases in myocytes after PRP injections into torn rotator cuff muscles.10 PRP has also been shown to be superior to corticosteroid injections for rotator cuff tears in both pain reduction and improvement in MRI-confirmed tissue damage after 12 weeks.11
Much of the discrepancy in current research within the field of PRP is likely due to the heterogeneity of the substances used. “PRP” is a non-specific term that does not have a standardized definition. Therefore, different studies on PRP may be testing substances with varying concentrations of platelets, WBCs, and/or RBCs – all of which modify the therapeutic effect. Much more research is needed in this area to determine optimal platelet concentrations, treatment frequency, and other parameters for maximal therapeutic benefit.
Adipose-Derived Stem Cell Therapy
The most recent addition to the landscape of RIT is Adipose-derived Stem Cell therapy (ASC). ASC prolotherapy utilizes the autologous mesenchymal stem cells (MSCs) and other pluripotent cells that are present in all adults. MSCs are able to differentiate into cartilage, muscle, tendon, ligament, or bone. Harvesting from adipose tissue is preferable due to the higher concentration of MSCs in adipose tissue as compared to other harvest tissues, including bone marrow.12 While stem cells’ ability to differentiate into various cell types is the most well-known characteristic of these cells, their action in exosomal and paracrine signaling likely contributes more to their observed clinical benefits. Additional reparative effects are achieved through MSC secretion of paracrine growth factors and cytokines, direct cell-cell interactions through tunneling nanotubes, and release of extracellular vesicles containing peptides, mRNA, and microRNAs that all combine to reduce inflammation and induce repair processes.13 The body of research supporting ASC therapy for various orthopedic conditions has grown very quickly, and the results are compelling for OA, meniscal tears, chondromalacia patellae, osteonecrosis, tendinopathy, and ligamentous tears.14
The clinical research is very new for stem cell therapies, and there is a lack of standardization between the studies that do exist, making large reviews of evidence difficult at this time. There is, however, a growing number of molecular-mechanism studies and small clinical trials that continue to produce favorable results for stem cell procedures.
Autologous stem cells can be harvested from 2 main areas: adipose or bone marrow. We believe that adipose is superior for several reasons. First, harvesting from adipose is less traumatic to the patient than harvesting from bone marrow. Second, adipose tissue has up to a 300-times higher concentration of MSCs compared to the same volume of bone marrow aspirate.12 Third, basic research indicates that adipose-derived mesenchymal stem cells (AD-MSC) have a stronger anti-inflammatory effect and a stronger chondrogenic effect in OA tissue than bone-marrow-derived MSCs.15
A small study recently published in the American Journal of Sports Medicine found that adipose-derived mesenchymal stem cell injections into the intra-articular space of the knee improved symptoms (per WOMAC score) and MRI findings over a 2-year follow-up period for patients with knee OA. This effect was found to be dose-dependent, with the patients receiving higher volumes of stem cells having a more durable effect, improving for up to 2 years before plateauing.16 The lower-dose group saw improvement for 1 year before plateauing.
A recent in-vitro study published in Cell Immunology showed that AD-MSCs promote T-regulatory cell activity and inhibit TNF-alpha secretion in rheumatoid arthritis models, opening up the possibility of addressing the autoimmune process in the joint with RIT.17
At our clinic, we add a small amount of PRP into the stem-cell injection solution. In-vitro studies by Lang et al demonstrate that PRP in combination with mesenchymal stem cells increases stem cell proliferation through platelet-derived growth-factor stimulation.18
Summary
OA is a debilitating condition, the morbidity of which will only increase in coming years. Regenerative orthopedics and the associated injection therapies are effective, safe, and utilize the body’s own healing power to accomplish the restoration of natural function. Movement is a primary need for the human body and mind. Therefore, restoring the ability to be physically active by reducing pain and joint dysfunction should be a priority for every physician with every patient. Dextrose prolotherapy, PRP, and adult stem cell therapies are all techniques that should be top of mind when evaluating patients for joint pain and musculoskeletal dysfunction. Movement is the key to health, and naturopathic regenerative orthopedics is the Vis Medicatrix Naturae at work. It can be a crucial piece of keeping patients moving throughout their lives.
References:
- Drengk A, Zapf A, Stürmer EK, et al. Influence of platelet-rich plasma on chondrogenic differentiation and proliferation of chondrocytes and mesenchymal stem cells. Cells Tissues Organs. 2009;189(5):317-326.
- Tohidnezhad M, Bayer A, Rasuo B, et al. Platelet-Released Growth Factors Modulate the Secretion of Cytokines in Synoviocytes under Inflammatory Joint Disease. Mediators Inflamm. 2017;2017:1046438.
- Rubio-Azpeitia E, Bilbao AM, Sánchez P, et al. The Properties of 3 Different Plasma Formulations and Their Effects on Tendinopathic Cells. Am J Sports Med. 2016;44(8):1952-1961.
- Meheux CJ, Mcculloch PC, Lintner DM, et al. Efficacy of Intra-articular Platelet-Rich Plasma Injections in Knee Osteoarthritis: A Systematic Review. Arthroscopy. 2016;32(3):495-505.
- Forogh B, Mianehsaz E, Shoaee S, et al. Effect of single injection of platelet-rich plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trial. J Sports Med Phys Fitness. 2016;56(7-8):901-908.
- Campbell KA, Saltzman BM, Mascarenhas R, et al. Does Intra-articular Platelet-Rich Plasma Injection Provide Clinically Superior Outcomes Compared With Other Therapies in the Treatment of Knee Osteoarthritis? A Systematic Review of Overlapping Meta-analyses. Arthroscopy. 2015;31(11):2213-2221.
- Smith PA. Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Efficacious Treatment for Knee Osteoarthritis: An FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial. Am J Sports Med. 2016;44(4):884-891.
- Sánchez M, Guadilla J, Fiz N, Andia I. Ultrasound-guided platelet-rich plasma injections for the treatment of osteoarthritis of the hip. Rheumatology (Oxford). 2012;51(1):144-150.
- Hussein M, Hussein T. Effect of autologous platelet leukocyte rich plasma injections on atrophied lumbar multifidus muscle in low back pain patients with monosegmental degenerative disc disease. SICOT J. 2016;2:12.
- Takase F, Inui A, Mifune Y, et al. Effect of platelet-rich plasma on degeneration change of rotator cuff muscles: In vitro and in vivo evaluations. J Orthop Res. 2017;35(8):1806-1815.
- Shams A, El-sayed M, Gamal O, Ewes W. Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol. 2016;26(8):837-842.
- Fellows CR, Matta C, Zakany R, et al. Adipose, Bone Marrow and Synovial Joint-Derived Mesenchymal Stem Cells for Cartilage Repair. Front Genet. 2016;7:213.
- Jin R, Shen M, Yu L, Wang X, Lin X. Adipose-Derived Stem Cells Suppress Inflammation Induced by IL-1β through Down-Regulation of P2X7R Mediated by miR-373 in Chondrocytes of Osteoarthritis. Mol Cells. 2017;40(3):222-229.
- Pak J, Lee JH, Park KS, et al. Current use of autologous adipose tissue-derived stromal vascular fraction cells for orthopedic applications. J Biomed Sci. 2017;24(1):9.
- Pagani S, Borsari V, Veronesi F, et al. Increased Chondrogenic Potential of Mesenchymal Cells From Adipose Tissue Versus Bone Marrow-Derived Cells in Osteoarthritic In Vitro Models. J Cell Physiol. 2017;232(6):1478-1488.
- Jo CH, Chai JW, Jeong EC, et al. Intra-articular Injection of Mesenchymal Stem Cells for the Treatment of Osteoarthritis of the Knee: A 2-Year Follow-up Study. Am J Sports Med. 2017;45(12):2774-2783.
- Usha Shalini P, Vidyasagar JV, Kona LK, et al. In vitro allogeneic immune cell response to mesenchymal stromal cells derived from human adipose in patients with rheumatoid arthritis. Cell Immunol. 2017;314:18-25.
- Lang S, Herrmann M, Pfeifer C, et al. Leukocyte-reduced platelet-rich plasma stimulates the in vitro proliferation of adipose-tissue derived mesenchymal stem cells depending on PDGF signaling. Clin Hemorheol Microcirc. 2017;67(2):183-196.
Image Copyright: <a href=’https://www.123rf.com/profile_seoterra’>seoterra / 123RF Stock Photo</a>
 Noel Peterson, ND, DAAPM, has practiced in Lake Oswego, OR, since 1978, where he has provided decades of broad-based naturopathic medical care. Dr Peterson is the medical director of Oregon Regenerative Medicine, is certified in prolotherapy by the AAOM, and is a diplomat of the AAPM. He has extensive teaching experience in regenerative medicine, and serves as faculty for the American Association of Orthopaedic Medicine’s prolotherapy. Oregon Regenerative Medicine (ORM) has served as a CNME-accredited residency training site as well as a site for multi-discipline physicians learning to perform platelet-rich plasma prolotherapy and stem cell therapy protocols developed at ORM.
Noel Peterson, ND, DAAPM, has practiced in Lake Oswego, OR, since 1978, where he has provided decades of broad-based naturopathic medical care. Dr Peterson is the medical director of Oregon Regenerative Medicine, is certified in prolotherapy by the AAOM, and is a diplomat of the AAPM. He has extensive teaching experience in regenerative medicine, and serves as faculty for the American Association of Orthopaedic Medicine’s prolotherapy. Oregon Regenerative Medicine (ORM) has served as a CNME-accredited residency training site as well as a site for multi-discipline physicians learning to perform platelet-rich plasma prolotherapy and stem cell therapy protocols developed at ORM.
***
 Samuel G. Oltman, ND, is a naturopathic physician specializing in regenerative orthopedics at Oregon Regenerative Medicine in Lake Oswego, OR. After graduating in 2015, Dr Oltman completed a 2-year CNME-accredited residency in SE Portland, focused on family medicine. He has since received specialized training in regenerative injection therapies at ORM as well as musculoskeletal ultrasound training, and is working toward his RMSKUS certification. In addition to orthopedics, Dr Oltman specializes in TBI evaluation and treatment, offering unique regenerative medicine-based modalities for concussion recovery.
Samuel G. Oltman, ND, is a naturopathic physician specializing in regenerative orthopedics at Oregon Regenerative Medicine in Lake Oswego, OR. After graduating in 2015, Dr Oltman completed a 2-year CNME-accredited residency in SE Portland, focused on family medicine. He has since received specialized training in regenerative injection therapies at ORM as well as musculoskeletal ultrasound training, and is working toward his RMSKUS certification. In addition to orthopedics, Dr Oltman specializes in TBI evaluation and treatment, offering unique regenerative medicine-based modalities for concussion recovery.