Gil Winkelman, ND, MA
Abstract
Mild and unrecognized traumatic brain injuries can lead to chronic migraines, hormonal imbalance, cognitive decline, and mood disorders. Updated prevalence data, subtle diagnostic cues, and targeted patient history improve detection of these “invisible injuries.” An integrative approach using neurofeedback, nutritional therapy, and homeopathy supports neuronal repair, reduces symptoms, and restores cognitive and emotional balance. A clinical case demonstrates recovery with Low Energy Neurofeedback System sessions, vitamin and mineral repletion, and homeopathic support.
Introduction
Even mild or forgotten head injuries can cause lasting emotional, cognitive, and physical symptoms. This article explores how integrative therapies—like neurofeedback, nutrition, and homeopathy—can help uncover and heal the hidden impacts of TBI.
Even with greater awareness over the last decade, Traumatic Brain Injury (TBI) still remains a silent epidemic. Though often underdiagnosed, it can be the hidden cause behind a variety of physical, emotional, and cognitive symptoms, including chronic pain. A single head injury—sometimes without loss of consciousness or obvious trauma—can result in long-term complications that affect every aspect of a patient’s life.1 The older the patient, the greater the risk. As clinicians, understanding how to recognize and address TBI can be transformative for our patients.
The Prevalence and Complexity of TBI
The Centers for Disease Control and Prevention (CDC) estimates that at least 2.5 million TBIs occur annually in the U.S., with some experts suggesting the actual number is closer to 3 million.2,3 That means a TBI happens every 11 seconds. While the data is mostly accurate for severe TBIs because it leads to emergency room visits, mild ones are often overlooked in clinical settings.
Mild TBI (mTBI) does not always involve visible trauma or loss of consciousness. Often, even the patient doesn’t notice that anything is wrong. They continue with their activities without seeking medical attention. But the impacts can be significant. Symptoms can appear weeks or months after the incident, making it difficult to connect the injury to new-onset issues such as fatigue, anxiety, chronic pain, digestive problems, or memory loss.
The Emotional, Cognitive, and Physical Effects
TBI can produce a wide range of symptoms in the body. Let’s break these down into emotional, physical, and cognitive changes.
Emotional Changes:2
TBI can impair emotional regulation. A previously mild-mannered patient may suddenly exhibit aggression, inappropriate social behavior, or emotional lability, such as crying or laughing without reason. Common emotional symptoms include:
- Anxiety or depression
- Increased risk-taking or impulsivity
- Indifference to others’ needs
- Hypersexuality or poor judgment
- Changes in social etiquette or grooming habits
These behaviors often emerge subtly and progressively, so even close family members may not associate them with a brain injury.
Cognitive Decline:
TBI can mimic or exacerbate disorders like ADHD. Patients may struggle with attention, memory, or executive function. Remarkably, they may not even realize how much their cognitive capacity has declined. One patient described her pre-treatment state as “living in a fog,” which only became clear after effective therapy. Another factor with TBI in the elderly is that there appears to be a link between TBI and dementia. A 55-year-old with a moderate concussion and a 65-year-old with a mild TBI are more likely to develop dementia than a cohort without one.4
Physical Dysfunction:2
The physical consequences of TBI are often the most unexpected. Symptoms can affect virtually every system:
- Pituitary dysfunction (e.g., hypothyroidism, infertility, adrenal insufficiency)
- Sensory loss or exaggeration (e.g., vision, smell, hearing)
- Migraines, fatigue, or chronic pain
- Digestive dysfunction, often resembling IBS
- Bladder or bowel control issues
- Unexplained panic attacks or body temperature instability
These symptoms may appear unrelated unless one considers the unifying role of the brain.
Identifying the Invisible Injury
Asking, “Have you had a brain injury?” often results in a “no.” People minimize or forget past trauma, especially when it didn’t lead to hospitalization. Ask instead:
- Have you ever had a car accident?
- Have you ever played contact sports?
- Worked in a hazardous occupation?
- Ridden horses, skateboards, snowboards, motorcycles, or bicycles?
- Served in the military?
If a patient has emotional, cognitive, and physical complaints with no unifying diagnosis, suspect TBI—the odd thing about many TBIs that I’ve found in my practice. People don’t remember them until after they have been treated. I once had a patient who came in denying TBI until I did neurofeedback on him. He came back the next week and told me he remembered he fell off a ladder at a worksite and landed on his head! Fortunately, we have treatments for cases like these
A Case Study: Integrative Recovery Through Neurofeedback and Nutrition
Patient Profile:
A 60-year-old woman presented with fatigue, migraines, memory loss, insomnia, weight gain, constipation, and a history of infertility. She recalled a car accident during her first pregnancy decades earlier but had never connected it to her current symptoms. Her migraines started soon after that incident.
Treatment Plan:
She received weekly sessions of Low Energy Neurofeedback System (LENS), a gentle form of EEG-based biofeedback that uses low-level electromagnetic signals to stimulate dormant neurons. Treatment was augmented with:
- Vitamin D (5,000 IU/day) – Essential post-TBI, especially when fatigue is present (5,6)
- Magnesium (125 mg/day) – To support neurological recovery and reduce excitability (7.8)
- Homeopathic pituitary gland – To address hormonal imbalances
Results:
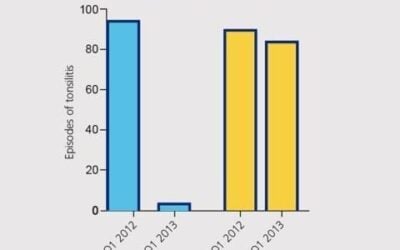
Her sleep improved almost immediately. Over 12 weeks, she experienced better memory, weight loss, normalized digestion, and increased energy. Before treatment, her brain map showed dominant delta waves (indicative of inappropriate “sleep” states during waking hours). After treatment, the map showed improved activity in alpha and low-beta ranges, typical of an alert, healthy adult brain. She also reported that migraines became less frequent in the first month. She had weekly migraines that only occurred monthly after initiating neurofeedback. She reported one more migraine in the next 2 months.
Her sleep-wake cycle shifted from 1 AM–6 AM to a healthier 10 PM–7 AM rhythm, suggesting not just improved sleep, but restored circadian balance.
Nutritional Support for Brain Recovery
Nutrition plays a vital role in mitigating inflammation, reducing oxidative stress, and supporting neuronal repair. For TBI, I find a few supplements that are much better than others.
1. Omega-3 Fatty Acids (EPA/DHA)
- Reduce neuroinflammation and support synaptic plasticity9,10.11
- Promote membrane stability and improve mood
- Suggested Dose: 3g/day
- Clinical studies show improved recovery rates and decreased depression symptoms when supplemented early.
2. Antioxidants
TBI increases oxidative stress, making antioxidant support essential.
- Vitamin C: Neuroprotective and anti-inflammatory
- Vitamin E: Prevents free radical damage
- CoQ10: Crucial for mitochondrial function; especially helpful in brain-related fatigue
- Blueberry Anthocyanins: Regulate BDNF and reduce inflammation12
3. Magnesium
- Commonly depleted after TBI
- Stabilizes neural activity, reduces headaches, and anxiety
- Supports ATP (energy) production6,7,8
- Dose: 125 mg/day
4. Curcumin
- Crosses the blood-brain barrier
- Anti-inflammatory and antioxidant13
- May help with neurogenesis and reduce amyloid plaque buildup
- Choose high-potency, bioavailable formulations
5. Vitamin D
- TBI depletes vitamin D stores5,6
- Low levels correlate with fatigue, depression, and poor recovery outcomes
- Recommended Dose: 3,000–5,000 IU/day, with monitoring for toxicity
6. B Vitamins
- Riboflavin (B2): Aids ATP production; 400 mg/day shown to improve TBI recovery in early studies
- B12: Prevents cognitive decline; essential for older adults whose absorption declines with age
- Consider B12 injections for those over 5515
7. Zinc Picolinate
- Supports the blood-brain barrier and neuronal repair21
- Deficiency worsens TBI outcomes
- Supplementation improves recovery, particularly if started early
Neurofeedback: Reawakening Dormant Neurons
One of the most promising therapies in the integrative toolbox is neurofeedback. While traditional EEG-based systems require more and longer sessions, LENS neurofeedback requires fewer sessions and uses significantly lower wattage, about a million times less than standard systems.
LENS “maps” the brain, tracking amplitude and frequency across 21 points. TBI patients often show:
- High delta wave activity (inappropriate for wakefulness)
- Irregular amplitudes in non-delta bands
The goal is not to force specific brainwave patterns but to “nudge” the brain out of dysfunctional states. Patients often report improved attention, memory, reduced anxiety, and better emotional regulation.
Research suggests an 80% success rate in symptom reduction using neurofeedback for TBI-related issues.3,17,18,19
Final Thoughts
TBI is an often-overlooked root cause of chronic, diffuse symptoms. When standard treatments fail, it’s worth revisiting the patient’s trauma history, no matter how long ago it occurred. Recovery is possible with a thoughtful, integrative approach that includes nutritional support, neurofeedback, homeopathy, and careful patient listening.
Each brain is unique, but the human capacity for healing is profound, especially when we treat not just symptoms, but the hidden injuries beneath them.
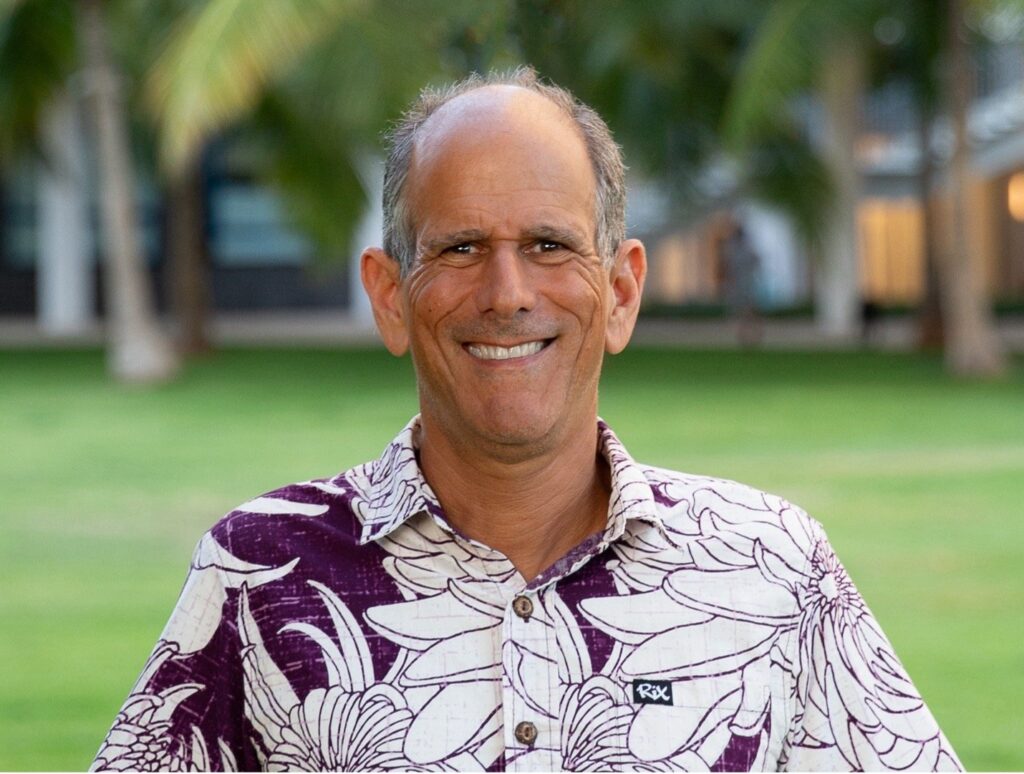
Dr. Gil Winkelman, ND, MA, is a Naturopathic Physician with over 25 years of experience treating physical, mental, and neurological issues. Dr. Gil authored several books, including Feel Well, Play Well: Amazing Golf through Whole Health. He is the creator of an online course, Why Folates Make Anxiety Worse, and the AskDrGil Podcast, where he speaks about various topics related to holistic health. He lives in Honolulu, Hawaii. www.askdrgil.com
References
- University of Pennsylvania School of Medicine. (2010). Mild traumatic brain injury, not so mild after all. Mild traumatic brain injury, not so mild after all. ScienceDaily. Retrieved from http://www.sciencedaily.com/releases/2010/02/100219204409.htm.
- Traumatic Brain Injury: A Roadmap for Accelrating Progress from NIH National Library https://www.ncbi.nlm.nih.gov/books/NBK580076/
- Hammond, D. C. (2003). Journal of Neurotherapy, 7(2), 25–52.
- JAMA Neurol. (2014). 71(12):1490-1497. doi:10.1001/jamaneurol.2014.2668
- . Schneiders, J. (2010). European Congress of Endocrinology.
- . Cekic, M., & Stein, D. G. (2009). Front Neuroendocrinol, 30(2), 158–172.
- McIntosh, T. K., et al. (1989). Brain Res, 482(2), 252–260.
- Nielsen, F. H. (2010). Nutr Rev, 68(6), 333–340.
- Barbagallo, M., & Dominguez, L. J. (2010). Curr Pharm Des, 16(7), 832–839.
- Wu, A., et al. (2007). J Neurotrauma, 24(10), 1587–1595.
- , A. C. (2008). J Neurotrauma, 25(12), 1499.
- Chang, C. Y., et al. (2009). Acta Neurol Taiwan, 18(4), 231–241.
- Maaouf, M., Rho, J. M., & Mattson, M. P. (2009). Brain Res Rev, 59(2), 293–315.
- Kossoff, E. H., & Rho, J. M. (2009). Neurotherapeutics, 6(2), 406–414.
- Improving treatments and outcomes: an emerging role for zinc in TBI. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4177718/
- Levesque, J., et al. (2006). Neurosci Lett, 394(3), 216–221.
- , M., et al. (2002). J Neurotherapy, 6(1), 23–38.
- Larsen, H. S. (2006). The Healing Power of Neurofeedback. Healing Arts Press.
- Sandberg-Lewis, K. (2010). Personal communication in Holistic Primary Care.
- Werner, C., & Engelhard, K. (2007). Br J Anaesth, 99(1), 4–9.