Radiofrequency Mole Removal
Aesthetic Medicine or Minor Surgery?
Hilary Costello, ND
In the age of rapidly growing statistics for skin cancers internationally, it is our duty as naturopathic physicians to educate our patients on appropriate techniques for the removal and potential biopsy of skin lesions. The clinical decision-making process to appropriately decipher between a growth that should be evaluated by a pathologist versus a lesion that can simply be removed without biopsy, may prove to be quite challenging, especially in the case of a seemingly simple mole.
When to Biopsy?
Is it essential to biopsy absolutely everything that is removed surgically? Most dermatologists and pathologists will agree that all skin lesions, especially of a papular or pigmented nature, should be biopsied without question when removed. However, in the world of aesthetic medicine, skin growths such as skin tags, actinic and seborrheic keratoses, sebaceous hyperplasia, syringoma, xanthelasma, and areas of hyperpigmentation are not always biopsied. Many of these types of lesions are destroyed in the process of removal. For example, a basic cryotherapy treatment freezes the tissue, causing cellular death with an eventual sloughing-off of the entire lesion in the form of a scab. The end goal of removal is achieved, but with this type of destruction procedure, a biopsy cannot be performed.
In the case of multiple skin tag removal, should every skin tag be individually biopsied? Should every verruca vulgaris be biopsied? Is cryotherapy sufficient despite the fact that several possible diagnoses may exist for similarly appearing lesions? Clinically experienced practitioners and pathologists may disagree about this. How many seborrheic keratoses need to be visualized and diagnosed via biopsy before being able to make a confident clinical judgment that it is unlikely to be melanoma or another type of concerning lesion? These clinical decisions are somewhat controversial, yet important to consider when doing this type of work.
Advantages of Radiofrequency Surgery
Fortunately, a great option does exist within our scope of practice in states licensed for minor surgery. It is called radiofrequency surgery and it truly offers the best of outcomes in all categories. It provides exceptional cosmetic results with minimal to no scarring, fast healing, and the potential to acquire a skin biopsy for clear diagnosis. It can be performed safely on any part of the skin or mucosa, and is an effective treatment for people of all ages including children. Removal of a lesion only requires 1 office visit and the results are immediate.
In the case of the removal of a pigmented lesion, destruction techniques can potentially lead to an inappropriate distribution of melanocytes into deeper layers of the skin during the process of healing. Congenital compound melanocytic nevi are known to have the potential for return, especially after destruction techniques. If any cellular portion of the lesion remains after destruction, the nevus can readily grow back. The regrowth may appear as a small pigmented macule or freckle.
In the case of cryotherapy or electrocautery, it is very difficult to visualize during the procedure whether the entire lesion has been treated to its full depth. If a biopsy is indicated at a later time, for example if the lesion partially returns, inappropriate distribution of melanocytes during the initial procedure may result in an abnormal biopsy that cannot be clearly distinguished from melanoma upon pathological review. This lesion may then require a large, full-skin-thickness biopsy with 3-5 mm margins. In this example scenario, the patient that was hoping for a simple cosmetically pleasing mole removal may end up with a large scar and a large financial bill for the procedure, especially if a referral to a specialist was needed or if the patient is uninsured or under-insured for this type of procedure. Overall, pigmented lesions require extra caution when considering removal. As our principles inform us, Primum Non Nocere – first do no harm.
The 2 most common adverse effects associated with all dermatological skin surgeries are risk of infection and scarring. Not all procedural techniques for lesion removal are created equal. The larger excisions and punch biopsies requiring multiple sutures or larger shave or curette techniques do not maximize scar prevention. Unfortunately, these types of techniques are some of the most common that a patient may experience in a standard dermatology practice. In addition, post-operative care may be less than optimal. Oftentimes, petroleum jelly is recommended as the treatment of choice for topical application without any mention of medicines that encourage the skin to regenerate and heal. As part of our standard scope of naturopathic medicine and the Vis Medicatrix Naturae – the healing power of nature – we have many therapeutic options to help with tissue regeneration, scar prevention, and antimicrobial activity. For example, Calendula officiinalis (calendula) succus, tinctures of Centella asiatica (gotu kola), Hydrastis canadensis (goldenseal), Mahonia aquifolium (Oregon grape), Aloe vera juice, tamanu oil, vitamin A, lavender, and Helichrysum italicum essential oil, to name a few.
Standard biopsy techniques will be ideal, in the sense of clear margins and skin-depth visibility, but the patient may heal with a larger than ideal scar. There is always the option of plastic surgery; however, for many patients this is cost-prohibitive and seemingly excessive for a simple mole removal. Techniques including advanced suturing styles, such as running subcuticular stitches, and the use of very thin suturing material, such as 6-0 silk, will improve the final outcome in comparison to standard nylon 4-0 simple interrupted or vertical or horizontal mattress stitches.
Radiofrequency surgery is an option that is quickly gaining popularity for its precision-cutting ability, minimal to no scarring, and immediate results for the patient. Over the last several years, radiofrequency surgery for mole removal has been written about in fashion magazines after celebrities have chosen this technique to be the most desirable way of removing moles in the entertainment industry.
Over the last 10 years of practice, I have removed thousands of lesions via radiofrequency surgery, ranging from skin tags, verruca of all types and locations including the genitals and tongue, simple benign nevus, keratoses of all shapes and sizes, and melanomas diagnosed upon biopsy. Many times I have found myself in the face of the ever-looming question of whether to biopsy or not to biopsy, especially in patient cases that are purely driven by aesthetics.
How to Use Radiofrequency in Your Practice
It is ultimately in the best interest of our patients to be prudent and conservative with respect to the removal of skin lesions. When the option to biopsy exists, it is best to take the tissue sample and send for the pathology report. Definitive diagnosis exemplifies Tolle Causam – identify and treat the cause. This guarantees the best outcome for the patient and provides the practitioner with peace of mind.
Diagnostic holistic dermatology and aesthetic medicine can coexist, especially with the use of radiofrequency technologies. Dermatology becomes an art and science mirroring our systems of naturopathic medicine. Holistic naturopathic care addresses the whole person, from the diagnosis of the cellular types via biopsy, to encompassing and being thoughtful and intentional about the self-esteem concerns and aesthetic presentation of the patient’s body and mind. This is our principle of Tolle Totum – treat the whole person.
Procedure
Radiofrequency units operate on a household current and convert energy into a high-frequency, low-temperature waveform of approximately 4.0 MHz. This wavelength exists between that of a radio and television wavelength. Essentially, only the cells that come into contact with the radio wave detach, while the remaining skin cells are largely undamaged. The skin at the base of the lesion heals quickly without the skin needing to create significant scar or fibrotic tissue.
Initially, the skin can be anesthetized with a compounded BLT cream (benzocaine, lidocaine, tetracaine,), and then injected at the base with a 1% or 2% lidocaine or similar anesthetic with or without epinephrine (1:100 000). The removal is then generated by using a delicate stainless-steel electrode of varying shape and size, that delivers the energy to the skin. The fine radio-wave electrode glides with pressureless contact on the skin. It is an artistic process similar to watercolor painting with a fine brush.
There are a multitude of diverse electrode tips to select for each unique lesion. This gives the practitioner immense versatility. Radiofrequency units allow for selection of specific waveforms, and therefore a lesion can be excised with a low, pure cutting current without disrupting the histopathologic diagnosis. In addition, as another option for treatment, a shave biopsy may be taken initially and then followed by the use of the radiofrequency electrode to perfect the lesion base and address bleeding. There are specific waveforms that can be used to seal tiny capillaries without causing cauterization or burning of the skin.
Personal Experience
In my opinion, one of the greatest benefits of radiofrequency surgery is the ability to remove lesions that are challenging due to size or location on the body. Many patients that I have treated have seen multiple doctors for a “difficult to treat” lesion, most commonly near the edge of the eyelids, around the mouth or on the genitals.
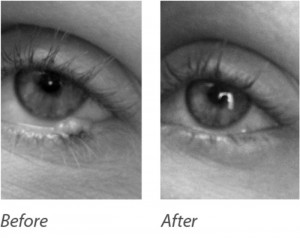
The “before and after” photos in Figure 1 present the case of a benign nevus on the lower eyelid border between the eyelashes and the eyeball. This 32-year-old female Caucasian patient presented to my office after visiting several physicians who were unable to surgically remove this lesion for her, for various precautionary reasons. Due to the precision-cutting nature of radiofrequency, we were able to remove this lesion simply and easily during a brief, single office visit. The “after” picture was taken immediately after the procedure, and the patient left feeling very happy and relieved. The lesion was beginning to affect her peripheral vision as she blinked, and she noticed people staring at it during conversations. In this case, the aesthetics and functionality were both addressed via removal.
The “before and after” photos in Figure 2, are of a 36-year-old Latino man with a large benign nevus on his face. He was mostly concerned with the aesthetics of the lesion, as it had grown to be quite large over the prior several years. It measured 9 mm. It had become challenging to shave on and around the lesion, and it was beginning to affect his self esteem. In this case, if a larger excision biopsy was chosen, the length of the incision, in order to be able to suture with properly approximated edges, would need to be nearly 2.5 cm. On the face, this is obviously not an aesthetically pleasing option. A punch biopsy would not be indicated either, due to the large diameter and the resulting dog ears that would form in the skin at the beginning and end of the incision line, due to the circular incision. After reviewing all of our options, we decided to remove the lesion via radiofrequency surgery. He was very pleased with the outcome.
Summary
For many reasons, radiofrequency surgery is an excellent technique for the removal of moles and other lesions. It is now used in surgical techniques of various types in the fields of dentistry, veterinary medicine, and even brain surgery because of its laser-like precision-cutting capabilities. Simple skin tags and moles, and skin growths that are considered higher risk due to location or potential for scarring, are perfect candidates for radiofrequency treatment. If choosing to perform aesthetic medicine skin procedures or dermatology surgery, it is essential to biopsy and inform patients of the potential risks involved in the removal of a seemingly simple mole. We must embody the principles of Docere – doctor as teacher – and teach about prevention and wellness by encouraging our patients to remember that the skin is the largest organ and a crucial part of a healthy body.
 Hilary Costello, ND, is a 2005 graduate of NCNM and practices medicine at Santé in NW Portland, Oregon. She received her bachelor of arts from Sarah Lawrence College in New York, where she studied fine arts painting and biology. She is the owner of LUCA Holistic Medicine, and is Board Chair of Jami Moja 501(c)(3), working in Kenya with Maasai communities in conjunction with the Girl Effect and Nike Foundation to empower the girl child through education and healthcare. Her work focuses on holistic dermatology, minor surgery, and art. She teaches naturopathic minor surgery seminars. For more information, visit LUCAholisticmedicine.com.
Hilary Costello, ND, is a 2005 graduate of NCNM and practices medicine at Santé in NW Portland, Oregon. She received her bachelor of arts from Sarah Lawrence College in New York, where she studied fine arts painting and biology. She is the owner of LUCA Holistic Medicine, and is Board Chair of Jami Moja 501(c)(3), working in Kenya with Maasai communities in conjunction with the Girl Effect and Nike Foundation to empower the girl child through education and healthcare. Her work focuses on holistic dermatology, minor surgery, and art. She teaches naturopathic minor surgery seminars. For more information, visit LUCAholisticmedicine.com.