Dairy Removal in Kids: Rewards & Risks
Lindsay Self, BA (Hons), ND
Mary MacDonald, ND, BSc, BComm
Dairy is a well-known allergen for many children. Many naturopathic doctors choose an elimination diet as a first-line treatment for pediatric asthma, eczema, constipation, esophagitis, and chronic congestion, with particular attention being paid to removal of dairy. Anecdotal and experiential evidence suggests this is an effective treatment for many patients; however, given the rapid growth and change experienced by children, can this long-term removal of dairy have negative effects?
The emphasis on promoting dairy intake for children surrounds concern for adequate skeletal growth and development, protein energy intake, and prevention of deficiencies of calcium, vitamin D, phosphorus, and vitamin B.1,2 Calcium and vitamin D are of particular concern due to the direct impact on growth and development, as 80% of bone mass is produced from birth to adolescence.3 When it comes to dairy, 2-4 servings per day, based on age, have been recommended to ensure adequate intake that meets recommendations for these nutrients.4 An estimated 37% of bone mineralization occurs between puberty stages 2 and 4 in adolescent girls. Consequently, supportive nutrients are crucial at this stage, as bone mineral density (BMD) acquired here will be carried through to menopause when fracture risk becomes important.5 Dairy also directly increases insulin-like growth factor (IGF), which is a stimulus for bone production.
Milk and cheese should be discussed separately, as nutritional benefits and allergenic potential of both differ due to differences in whey and casein content. Both are good sources of protein at approximately 8 grams and provide approximately 25% of the daily intake of calcium per serving. Milk carries higher micronutrient value of magnesium, phosphorus, and potassium, and of vitamins D, B2, B12, B5, and B6. Both cheese and milk are good sources of vitamin A, zinc, and selenium. This represents a nutrient-dense food, thus removal of this source should be examined in light of potential deficiencies that could result.
Conditions That May Benefit from Dairy Removal
Iron Deficiency
A subset of children are at higher risk for iron deficiency. These children include premature and low birth-weight infants, children exposed to high levels of lead through ingestion via foods and water, and children with a high-dairy diet. Many well-done studies on human subjects show that calcium can inhibit iron absorption, regardless of whether calcium is given via food intake or supplementation.6- 8 Specifically of note are the findings that daily cow’s milk intake of more than 2 cups each day, longer breastfeeding duration, and a higher body mass index (BMI) are modifiable risk factors associated with iron deficiency.8 Separating calcium-rich foods and iron-rich foods to prevent iron deficiency can be practically difficult for parents and children, so guidance is required.
Atopic Conditions
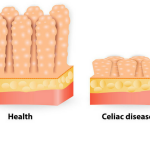
Atopy refers to the genetic tendency to develop allergic diseases such as allergic rhinitis, asthma, atopic dermatitis (eczema), and eosinophilic esophagitis. Atopy is typically associated with heightened immune responses to common allergens, especially inhaled allergens and food allergens. The immune reaction results in increased IgE antibody production and increased mast cell production. One of the most common allergens associated with atopic conditions is cow’s milk.6 Atopic children may independently be at risk for poor growth, and the contribution of dairy nutrients to their diet should be considered.6
While the manifestations of exposure to food allergens vary in terms of the underlying immunological reaction, clinical presentation, severity, and time course, it is clear that multiple food allergens may serve as triggers for dermatitis. In selected patients with atopic dermatitis, avoidance of specific dietary allergens has resulted in improvement of signs and symptoms of chronic dermatitis.9,10 In infants who are breastfed, avoidance of dairy by the mother results in decreasing prevalence in the development and severity of atopic dermatitis in the infant.11
Eosinophilic esophagitis is an underdiagnosed cause of infant and child gastroesophageal reflux disease. The pathophysiology of this condition results in increased eosinophil production as a result of an allergy. There is growing evidence to suggest that this condition is a subset of the atopic diathesis, and the underlying pathophysiology has been difficult to explain until now.12 One well-done study has shown that dietary therapy, specifically removing dairy from the pediatric patients’ diets, significantly increased the return to normal endoscopic appearance of the esophagus and led to complete remission in 59.3% of subjects in the study.12 For the vast majority of patients, all symptoms improved, including digestive (98.3%), cutaneous (80%), and respiratory (92.8%).
Constipation & Pediatric Inflammatory Bowel Disease
Undiagnosed cow’s milk allergy (CMA) may be immunoglobulin E (IgE)- or non-IgE-mediated, resulting in atopic symptoms including rhinitis, eczema, and gastrointestinal symptoms. CMA in infancy is associated with subsequent development of asthma and pediatric inflammatory bowel disease.13 CMA can also induce enterocolitis, which presents a strong potential for dehydration as a result of frequent vomiting episodes during the first months of life.13
Research has also shown us that CMA is a significant etiologic factor for constipation in infants and young children.10,14 Checking serum levels of IgE to cow milk proteins is helpful, although not definitive for diagnosis. Based on this limited study, tolerance is better achieved after 12 months of strict cow’s milk elimination.14
Risks Associated with Dairy Removal
Several studies have demonstrated a direct relationship between lower dairy intake, lower BMD, and skeletal malformations.1,2,10,15-19 A direct relationship exists between lower dairy intake and smaller stature, lower total bone density, lower z-scores, lower serum calcium, higher parathyroid hormone (PTH), and higher alkaline phosphatase (ALP).1,2,10,15-19 The outcome appears to be a result of inadequate dietary calcium intake and concurrent vitamin D deficiency, in some cases leading to the development of rickets.15,17 Given that vitamin D regulates calcium absorption, it is understandable that these would be linked. Vitamin D deficiency is a widespread problem, particularly in northern latitudes. Supplementation here may be required to ensure adequacy.
Removal of dairy is often replaced with non-dairy calcium sources, which can be high in phytates and oxalates, both of which impair calcium absorption. Examples of these include spinach, almonds, chard, and grains.20 Phytic acid content in grains and legumes can be reduced by soaking, fermenting, or germinating for a number of hours prior to cooking and preparation.21
Concerns have also been expressed regarding protein, fat, vitamin B2, and niacin.1 Lower intakes of protein and fat are generally correlated with an overall lower calorie intake. Vitamin B2 and B3 deficiencies are rare, as non-dairy food sources are readily available, such as eggs, meat, vegetables, and whole grains.
Another concern with dairy elimination is the possibility of disordered eating patterns later in life. Maslin K et al showed that removal of cow’s milk in infancy affected adolescent eating behaviors of 101 individuals.22 They ate more slowly and were more likely to avoid certain foods and food groups, suggesting a negative eating behavior.22
Evaluating the Patient
When removing dairy, attention should be paid to the chief concern and reason for the dairy removal. If signs and symptoms resolve, suggesting an allergy or intolerance to dairy, evaluation of the diet should be taken into consideration to ensure adequate calcium and vitamin D intake. Daily requirements vary by age and can be found in Table 1.5 Consideration should also be paid to the levels of oxalate- and phytate-containing foods in order to ensure that absorption isn’t being hindered.20 Salt intake should be monitored, as dietary sodium will increase renal calcium excretion. Fussiness of infants’ and toddlers’ eating patterns should be evaluated to ensure they are tolerating potentially non-palatable foods.
Adolescents should be screened for disordered eating and negative eating patterns using clinical judgment or a standardized questionnaire. They also tend to have a lower intake of fruits and vegetables, a higher intake of sugar, fat, and meat, and greater sedentary time, all of which contribute to a lower bone density and increased cardiovascular risk factors.23 Activity levels and BMI should be monitored, as sedentary behavior will contribute to lower BMD.
Table 1. Daily Calcium & Vitamin D Requirements5
| AI | EAR | RDA | UL | |
| Calcium | ||||
| 0 to 6 months | 200 mg | 1000 mg | ||
| 6 to 12 months | 260 mg | 1500 mg | ||
| 1-3 years | 500 mg | 700 mg | 2500 mg | |
| 4-8 years | 800 mg | 1000 mg | 2500 mg | |
| 9-18 years | 1100 mg | 1300 mg | 3000 mg | |
| Vitamin D | ||||
| 0-6 months | 400 IU | 1000 IU | ||
| 6-12 months | 400 IU | 1500 IU | ||
| 1-3 years | 400 IU | 600 IU | 2500 IU | |
| 4-8 years | 400 IU | 600 IU | 3,000 IU | |
| 9-18 years | 400 IU | 600 IU | 4,000 IU |
(AI = Adequate Intake; EAR = Estimated Average Requirement; RDA = Recommended Dietary Allowance; UL = Upper Level Tolerable Intake)
Adapted from: IOM’s Dietary Reference Intakes for Calcium and Vitamin D; 2011.
Potential Signs of Deficiencies
On routine physical exam, signs of potential deficiencies should be monitored, although Aggarwal et al noted that 91% of hypocalcemic children were asymptomatic.15
- Calcium: Muscle and abdominal cramps, numbness or tingling, brittle or weak nails24
- Vitamin D: Frequent colds or illnesses, muscle pain, depression, fatigue
- Vitamin B2: Angular stomatitis24
- Overall growth and gait: Evaluation in reference to growth charts to ensure growth is not in a lower percentile, presence of bow-legging, delayed walking15
- BMI: A BMI >30 and increased adiposity is linked with lower vitamin D and higher PTH
Useful Laboratory Screens
Routine laboratory evaluation can detect potential deficiencies before they manifest physically. This should include:
- Serum total calcium: Low in many test subjects who did not eat dairy1,2,10,15-19
- PTH: Elevated in most cases where calcium was deficient
- Vitamin D: Particularly low in northern latitudes; however, several studies showed this was low even in sunnier climates15
- IgG and IgE antibodies to milk proteins: Remembering that atopy can be IgE- or non-IgE-mediated, an undiagnosed milk allergy should be investigated
- Bone density scan: If clinical presentation and blood work suggests a suspected deficiency, a bone density scan should be ordered to capture a baseline and dietary modification, and/or supplementation should be initiated
Treatment Implications
Early introduction of dairy may help lower the risk of a milk allergy, but may be dose-dependent, as research is uncertain.25 Regardless, it is safe and may be effective. Signs and symptoms should be monitored for individual reactions. Dairy allergies detected and removed in infancy may not be present by school age, and so reintroduction may be attempted on an occasional basis.26 If dairy is added back in the diet, it should be noted that butter has typically not induced an allergic response.27
Suggesting a removal of dairy from a child’s diet also provides an opportunity for naturopathic doctors to engage their patients and parents of patients in discovering new healthy alternatives to dairy consumption. Many children, particularly girls 9-18 years of age, are not reaching Recommended Daily Allowances (RDA) for calcium when focus is placed primarily on dairy intake for this goal.5
Furthermore, as discussed by the American Dietetic Association as well as the Dieticians of Canada,28,29 well-planned, nutrient-dense vegetarian and vegan diets are healthful and nutritionally adequate. In fact, many authors now cite the most healthful calcium sources to be those from green leafy vegetables and legumes.30
By providing alternate sources of calcium for those children at risk for the above-mentioned conditions, we can provide a nutrient-dense diet that is enriched by a variety of food choices. When dairy is removed, we must ensure adequate amounts of calcium and vitamin D via diet or through supplementation when necessary.5
The pediatric RDA for calcium ranges from 700 mg to 1300 mg, depending on the life stage of the child, to facilitate proper bone growth.5 As noted in Table 2,30,31 it is relatively easy to facilitate adequate calcium intake through non-dairy sources.5
Table 2. Non Dairy Sources of Calcium30,31
| Food Source | Serving Size | Amount of Calcium (mg) |
| Collard greens, frozen | 8 oz | 360 |
| Sardines, canned with bones | 3 oz | 325 |
| Almond, rice or soy milk, fortified | 8 oz | 300 |
| Orange and other fruit juices, fortified | 8 oz | 300 |
| Tofu, prepared | 4 oz | 205-800 |
| Broccoli rabe | 8 oz | 200 |
| Salmon, canned with bones | 3 oz | 180 |
| Kale, frozen | 8 oz | 180 |
| Soybeans, boiled | 8 oz | 175-260 |
| White beans, boiled | 8 oz | 160 |
| Bok choy, boiled | 8 oz | 160 |
| Oatmeal, fortified | 1 packet | 140 |
| Navy beans, boiled | 8 oz | 125 |
| Chickpeas, canned | 8 oz | 110 |
| Black turtle beans, boiled | 8 oz | 100 |
| English muffin, fortified | 1 muffin | 100 |
| Cereal, fortified | 8 oz | 100-1000 |
| Almonds | 1 oz | 75 |
| Sweet potato, boiled | 8 oz | 75 |
| Figs, dried | 2 | 65 |
| Broccoli, fresh or cooked | 8 oz | 60 |
| Oranges | 1 | 55 |
Vitamin D is important for the absorption of calcium into our bones. Without adequate amounts of vitamin D, only 10-15% of dietary calcium intake may be absorbed.32 It can be more difficult to provide adequate sources of vitamin D through dietary intervention, especially in areas of low sunlight.5 However, we can provide at least some of the RDA for vitamin D, which is 600 IU per day,5 by recommending daily intake of the foods found in Table 3.33,34 If necessary, there are also well-absorbed and safe supplementation options for vitamin D as well.
Table 3. Non-Dairy Sources of Vitamin D33,34
| Food Source | Serving Size | Amount of Vitamin D (IU) |
| Halibut, baked or broiled | 75 g | 1054 |
| Carp, baked or broiled | 75 g | 950 |
| Salmon, canned, drained without skin and bones | 75 g | 631 |
| Cod liver oil | 5 mL | 427 |
| Maitake mushroom | 125 mL | 411 |
| Salmon, wild, baked or broiled | 75 g | 338 |
| Cereal: Special K | 30 g | 113 |
| Tuna, baked or broiled | 75 g | 106 |
| Cashew milk alternative, enriched | 250 mL | 90 |
| Soy milk alternative, enriched | 250 mL | 86 |
| Almond milk alternative, enriched | 250 mL | 85 |
| Egg, chicken whole, cooked | 2 large | 84 |
| Pork side ribs, simmered, roasted | 75 g | 78 |
| Mackerel, Atlantic, cooked | 75 g | 78 |
| Coconut milk alternative, enriched | 250 mL | 76 |
| Morel mushroom, raw | 125 mL | 72 |
| Orange juice, fortified with vitamin D | 125 mL | 50 |
Care regarding the level of phytates and oxalates in the diet (Table 4) requires management. Reduction of phytic acid levels in grains and legumes can be reduced by soaking (up to 55% reduction), fermenting (up to 88% reduction), or germinating (up to 40% reduction).21 Soaking should be done with a mild acid solution, such as by adding vinegar to the soaking water for 2-12 hours. The soaking method also increases bioavailability of some minerals, such as iron and zinc, by 2-12%.21 Encouraging parents to purchase dried legumes and preparing them at home would be optimal.
Table 4. Foods Highest in Phytates21
| Food Source | Phytic Acid Content, g/100 g (dry weight) |
| Corn | 6.39 |
| Wheat bran | 2.1-7.3 |
| Rice bran | 2.56-8.7 |
| Barley | 0.38-1.16 |
| Oats | 0.42-1.16 |
| Kidney beans | 0.61-2.38 |
| Peas | 0.22-1.51 |
| Chickpeas | 0.28-1.60 |
| Lentils | 0.27-1.51 |
| Soybeans | 1.0-2.22 |
| Peanuts | 0.17-4.47 |
| Almonds | 0.35-9.42 |
| Walnuts | 0.2-6.69 |
| Cashews | 0.19-4.98 |
Conclusion
Removal of dairy can produce relief from many pediatric complaints, but does carry its own risk. Care should be taken to ensure that no nutrient deficiencies result, particularly of calcium and vitamin D, which could impair the child later in life.
 Lindsay Self, BA (Hons), ND, graduated in 2010 and completed her 2-year clinical residency at Canadian College of Naturopathic Medicine (CCNM). She currently practices in Brooklin, Ontario. She encourages a strong foundation in nutrition for each patient, and uses herbal medicine, nutritional supplementation, acupuncture, and Chinese Medicine to restore health. She helped to create and is Vice-President of NDI-Canada.
Lindsay Self, BA (Hons), ND, graduated in 2010 and completed her 2-year clinical residency at Canadian College of Naturopathic Medicine (CCNM). She currently practices in Brooklin, Ontario. She encourages a strong foundation in nutrition for each patient, and uses herbal medicine, nutritional supplementation, acupuncture, and Chinese Medicine to restore health. She helped to create and is Vice-President of NDI-Canada.
 Mary MacDonald, ND, BSc, BComm, graduated from CCNM in 2006 and currently is busy in naturopathic practice in Ontario, Canada. Mary combines her expertise in scientifically researched and naturally-based health care with her patients’ knowledge of their body’s physical, mental, and emotional health. She enjoys working with patients of all ages to help them achieve their true state of health. Through education and empowerment using dietary changes, nutritional supplementation, botanical medicine, acupuncture, and homeopathic medicine, Mary affects substantial change in the quality of her patient’s lives.
Mary MacDonald, ND, BSc, BComm, graduated from CCNM in 2006 and currently is busy in naturopathic practice in Ontario, Canada. Mary combines her expertise in scientifically researched and naturally-based health care with her patients’ knowledge of their body’s physical, mental, and emotional health. She enjoys working with patients of all ages to help them achieve their true state of health. Through education and empowerment using dietary changes, nutritional supplementation, botanical medicine, acupuncture, and homeopathic medicine, Mary affects substantial change in the quality of her patient’s lives.
References
- Henriksen C, Eggesbø M, Halvorsen R, Botten G. Nutrient intake among two-year-old children on cows’ milk-restricted diets. Acta Paediatr. 2000;89(3):272-278.
- Medeiros, LC, Speridião PG, Sdepanian VL, et al. Nutrient intake and nutritional status of children following a diet free from cow’s milk and cow’s milk by-products. J Pediatr (Rio J). 2004;80(5):363-370.
- Infante D, Tormo R. Risk of inadequate bone mineralization in diseases involving long-term suppression of dairy products. J Pediatr Gastroenterol Nutr. 2000;30(3):310-313.
- Fulgoni VL 3rd, Huth PJ, DiRienzo DB, Miller GD. Determination of the optimal number of dairy servings to ensure a low prevalence of inadequate calcium intake in Americans. J Am Coll Nutr. 2004;23(6):651-659.
- Institute of Medicine; Ross A, Taylor C, Yaktine A, Del Valle H, eds. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011:7-498.
- Agostoni C, Turck D. Is cow’s milk harmful to a child’s health? J Pediatr Gastroenterol Nutr. 2011;53(6):594-600.
- Lönnerdal B. Calcium and iron absorption–mechanisms and public health relevance. Int J Vitam Nutr Res. 2010;80(4-5):293-299.
- Cox KA, Parkin PC, Anderson LN, et al. TARGet Kids! Collaboration. Association Between Meat and Meat-Alternative Consumption and Iron Stores in Early Childhood. Acad Pediatr. 2016 Jan 20. pii: S1876-2859(16)00019-X. [Epub ahead of print]
- Katta R, Schlichte BSc. Diet and dermatitis: food triggers. J Clin Aesthet Dermatol. 2014;7(3):30-36.
- Hidvégi E, Arató A, Cserháti E, et al. Slight decrease in bone mineralization in cow milk-sensitive children. J Pediatr Gastroenterol Nutr. 2003;36(1):44-49.
- Jirapinyo P, Densupsoontorn N, Kangwanpornsiri C, Limlikhit T. Lower prevalence of atopic dermatitis in breast-fed infants whose allergic mothers restrict dairy products. J Med Assoc Thai.2013;96(2):192-195.
- Colson D, Kalach N, Soulaines P, et al. The impact of dietary therapy on clinical and biologic parameters of pediatric patients with eosinophilic esophagitis. J Allergy Clin Immunol Pract. 2014;2(5):587-593.
- Virta LJ, Kautiainen H, Kolho KL. Symptoms suggestive of Cow’s milk allergy in infancy and pediatric inflammatory bowel disease. Pediatr Allergy Immunol. 2016;27(4):361-367.
- El-Hodhod MA, Younis NT, Zaitoun YA, Daoud SD. Cow’s milk allergy related pediatric constipation: appropriate time of milk tolerance. Pediatr Allergy Immunol. 2010;21(2 Pt 2):e407-e412.
- Aggarwal V, Seth A, Aneja S et al. Role of calcium deficiency in development of nutritional rickets in Indian children: a case control study. J Clin Endocrinol Metab. 2012;97(10):3461-3466.
- Black RE, Williams SM, Jones IE, Goulding A. Children who avoid drinking cow milk have low dietary calcium intakes and poor bone health. Am J Clin Nutr. 2002;76(3):675-680.
- Davidovits M, Levy Y, Avramovitz T, Eisenstein B. Calcium-deficiency rickets in a four-year-old boy with milk allergy. J Pediatr. 1993;122(2):249-251.
- Infante D, Tormo R. Risk of inadequate bone mineralization in diseases involving long-term suppression of dairy products. J Pediatr Gastroenterol Nutr. 2000;30(3):310-313.
- Voloc A, Esterle L, Nguyen TM, et al. High prevalence of genu varum/valgum in European children with low vitamin D status and insufficient dairy products/calcium intakes. Eur J Endocrinol. 2010;163(5):811-817.
- Schlemmer U, Frølich W, Prieto RM, Grases F. Phytate in foods and significance for humans: food sources, intake, processing, bioavailability, protective role and analysis. Mol Nutr Food Res. 2009;53 Suppl 2:S330-S375.
- Gupta RK, Gangoliya SS, Singh NK. Reduction of phytic acid and enhancement of bioavailable micronutrients in food grains. J Food Sci Technol. 2015;52(2):676-684.
- Maslin K, Grundy J, Glasbey G, et al. Cows’ milk exclusion diet during infancy: Is there a long-term effect on children’s eating behaviour and food preferences? Pediatr Allergy Immunol. 2016;27(2):141-146.
- Moreno LA, Gottrand F, Huybrechts I, et al. Nutrition and lifestyle in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Adv Nutr. 2014;5(5):615S-623S.
- Marz R. Medical Nutrition From Marz. 2nd ed. Portland, OR: Omni-Press; 1998.
- Perkin MR, Logan K, Tseng A, Raji B, et al. Randomized Trial of Introduction of Allergenic Foods in Breast-Fed Infants. N Engl J Med. 2016;374(18):1733-1743.
- Doğruel D, Bingöl G, Yılmaz M, Altıntaş DU. The ADAPAR Birth Cohort Study: Food Allergy Results at Five Years and New Insights. Int Arch Allergy Immunol. 2016;169(1):57-61.
- Yanagida N, Minoura T, Kitaoka S. Butter Tolerance in Children Allergic to Cow’s Milk. Allergy Asthma Immunol Res. 2015;7(2):186-189.
- American Dietetic Association; Dieticians of Canada. Position of the American Dietetic Association and Dietitians of Canada: Vegetarian diets. J Am Diet Assoc.2003;103(6):748-765.
- Craig WJ, Mangels AR; American Dietetic Association. Position of the American Dietetic Association: vegetarian diets. J Am Diet Assoc.2009;109(7):1266-1282.
- Physicians Committee for Responsible Medicine. Protecting Your Bones. PCRM Web site. http://www.pcrm.org/sites/default/files/pdfs/health/Nutrition-Fact-Sheets/Protecting-Your-Bones.pdf. Accessed April 11, 2016.
- National Osteoporosis Foundation. A Guide to Calcium-Rich Foods. NOF Web site. https://www.nof.org/patients/treatment/calciumvitamin-d/a-guide-to-calcium-rich-foods/. Accessed April 11, 2016.
- Holick MF, Garabedian M. Vitamin D: Photobiology, Metabolism, Mechanism of Action, and Clinical Applications. In: Favus MJ, ed. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism. 6th ed. Washington, DC: American Society for Bone and Mineral Research; 2006:129-137.
- Health Canada. The Canadian Nutrient File. Modified December 12, 2015. Health Canada Web site. http://www.hc-sc.gc.ca/fn-an/nutrition/fiche-nutri-data/cnf_aboutus-aproposdenous_fcen-eng.php. Accessed April 13, 2016.
- Dieticians of Canada. Food Sources of Vitamin D. February 25, 2014. Dieticians of Canada Web site. http://www.dietitians.ca/Your-Health/Nutrition-A-Z/Vitamins/Food-Sources-of-Vitamin-D.aspx. Accessed April 13, 2016.